Probiotics
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Alternative Strategies For Antimicrobial Therapy
Probiotics are defined as living microorganisms that confer some health benefits when utilized in sufficient numbers. The use of harmless bacteria to replace pathogenic ones (bacteriotherapy) is not a new concept but has gained renewed interest in recent years.
PROBIOTICS
Probiotics are defined as living
microorganisms that confer some health benefits when utilized in sufficient
numbers. The use of harmless bacteria to replace pathogenic ones
(bacteriotherapy) is not a new concept but has gained renewed interest in recent
years. Particularly, they have been strongly marketed as a prophylactic
approach to the promotion of well-being. In addition, bacteriotherapy has been
used in the treatment of a variety of gastrointestinal conditions (including
diarrhoea), respiratory infections, recurrent bacterial vaginitis, recurrent
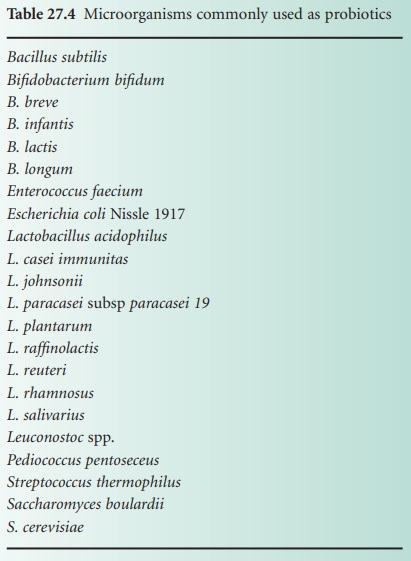
otitis media, streptococcal tonsillitis and infected burns. The microorganisms
most frequently used are normal components of the gut microflora and include
the lactic acid bacteria such as lactobacilli, lactococci, bifidobacteria,
enterococci and streptococci (see Table 27.4).
Other bacteria such as Bacillus species
and yeasts such as Saccharomyces may
also be utilized. Since each of these organisms possesses different
characteristics and requirements for growth it is likely that they do not have
a common mechanism of action.
A)
Gastrointestinal
Conditions
Probiotics for oral administration are
marketed as dairy products such as yoghurt drinks, but also as powders, tablets
or capsules. Irrespective of the nature of the product, there is a need to
consume in the region of 109–1011 microorganisms in order to bring about any
effect. A number of studies have highlighted issues of inconsistency in the
content of viable microorganisms within various products. The precise manner in
which probiotics bring about their health benefits is unclear, but a
prerequisite property is the ability to colonize the gut. The orally
administered organisms must first, therefore, be able to survive passage
through the stomach acid and then compete with the indigenous flora in the
intestine. A competitive edge will be provided by the ability to colonize the
gut wall and the capacity to produce bacteriocins. Probiotics have been administered
rectally to overcome the necessity for acid tolerance, but there is a risk of
spreading faecal pathogens.
Probiotics have been found to be of benefit in the treatment of
infectious diarrhoea in children. When used as a supplement to breast milk in premature
infants they were found to reduce the incidence and severity of necrotizing
enterocolitis. A recent review summarizing the available clinical trial data
has suggested value in the treatment of ulcerative colitis, but the results for
Crohn’ s disease were disappointing and the authors stated that the use of
probiotics could not be recommended on the available evidence.
Clostridium difficile is a Gram positive, spore-forming anaerobic rod which, in certain
conditions, can overgrow in the intestinal tract and produce toxins causing
diarrhoea and damage to the epithelial lining of the gut. This condition is a
particular problem in elderly hospitalized patients who have received courses
of broad-spectrum antibiotics. Since the colitis is caused by overgrowth of a
pathogenic bacterium in the intestinal tract it would seem to be potentially
amenable to probiotic treatment. However, a recent Cochrane review of the
current clinical trial data found that only treatment with Saccharomyces boulardii had any significant
effect. Many hospitals use a range of commercially available probiotic yoghurt
preparations but the effectiveness of these is currently unproven.
B)
Infected Burn Wounds
Burn wounds are devoid of
microorganisms immediately after the injury has been sustained, but fairly
quickly thereafter they will become colonized with microflora from the adjacent
intact skin and also by environmental microbes. These bacteria are mainly
Gram-positive coagulase-negative staphylococci, but they may be gradually replaced
by more harmful Gram-negative bacteria such as Ps.
aeruginosa and Acinetobacter spp.
over the following few days. These bacteria are notorious for being highly
antibiotic resistant and they flourish, often forming biofilms, because the
usual defensive properties of intact skin are no longer present. Colonization
with these organisms delays healing, can inhibit grafting and may lead to
systemic infection. Studies have shown that applications of Lactobacillus plantarum were as effective as
silver sulphadiazine in the management of infected burn wounds. This may be of
relevance in those countries where the costs of conventional antibiotic
treatment are prohibitive or where there is a high level of antibiotic
resistance.
C)
Recurrent Vaginitis
Many women suffer from vaginitis,
caused by either bacteria or Candida albicans, which
may lead on to urinary tract infections. In these cases the normal vaginal
microflora which comprises mainly lactobacilli is overrun by various other,
sometimes pathogenic, bacteria or fungi. The usual approach to treatment is the
administration of antibiotics, but recurrence is commonplace. The vaginal
administration of probiotic cultures has proved to be beneficial in these
cases; however, strains of bacteria isolated from dairy products are not always
suitable. The lactobacilli should be those that have the capacity to bind
specifically to vaginal epithelial cells.
D)
Acute Otitis Media
This is a very common condition in
young children in which bacteria normally present in the nasopharynx transfer
via the eustachian tube into the middle ear. The predominant bacteria are Streptococcus pneumoniae and Haemophilus influenzae. Antibiotic therapy is
frequently unsuccessful and recurrences are common. As we have seen in the
examples outlined above, the picture is once again one of undesirable bacteria
replacing normal commensal flora and causing disease. Studies have been reported
in which children were treated with suspensions of α-haemolytic streptococci
sprayed into the ear to inhibit the growth of the invading pathogens and
recolonize the infected site. The results showed that the treated patients had
significantly better outcomes than the placebo group.
Some workers have highlighted the fact
that probiotics should be used with caution in those patients whose immune
system is impaired because there have been reported incidences of invasive
infections occurring in immunocompromised adults. In addition, Lactobacillus bacteraemia has been reported
following probiotic therapy in two children who had received multiple courses
of antibiotics and who were suffering from other serious underlying conditions.
The currently available data suggest that probiotics may have some value
in certain selected conditions, but a great deal more background scientific
information is required before this can be moved forward substantially. The
approach of using a single culture for a whole spectrum of conditions is
untenable. It is clear that the probiotic bacteria will act in a variety ways,
producing arange of interfering substances and having different abilities to
adhere to epithelial cells. Individual cultures may therefore need to be
developed for use in specific conditions and once this has been achieved
large-scale trials are needed to verify their value.
