Principles of Microbial Pathogenicity and Epidemiology
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Principles Of Microbial Pathogenicity And Epidemiology
Microorganisms are ubiquitous, and most of them are free-living and derive their nutrition from inert organic and inorganic materials. The association of humans with such microorganisms is generally harmonious, as the majority of those encountered are benign and, indeed, are often vital to commerce, health and a balanced ecosystem.
PRINCIPLES OF MICROBIAL
PATHOGENICITY AND EPIDEMIOLOGY
Introduction
Microorganisms are
ubiquitous, and most of them are free-living and derive their nutrition from
inert organic and inorganic materials. The association of humans with such
microorganisms is generally harmonious, as the majority of those encountered
are benign and, indeed, are often vital to commerce, health and a balanced
ecosystem. The ability of bacteria and fungi to establish infections of plants,
animals and humans varies considerably. Some are rarely, if ever, isolated from
infected tissues, while opportunist pathogens (e.g. Pseudomonas aeruginosa or Staphylococcus
epidermidis) can establish themselves only in compromised individuals. Only a few species of bacteria may be
regarded as obligate pathogens, for which animals or plants are the only
reservoirs for their existence (e.g. Neisseria
gonorrhoeae, Mycobacterium tuberculosis and Treponema pallidum). Viruses, on the other hand, must parasitize host cells in order to replicate
and are therefore inevitably associated with disease. Even among the viruses
and obligate bacterial pathogens the degree of virulence varies, in that some
(particularly the bacteria) are able to coexist with the host without causing
overt disease (e.g. Staph. aureus),
while others will always cause some detriment to the host (e.g. rabies virus).
Organisms such as these invariably produce their effects, directly or
indirectly, by actively growing on or in the host tissues.
Other groups of
microorganisms may cause disease through ingestion of substances (toxins)
produced during microbial growth on foods (e.g. Clostridium botulinum, botulism; Bacillus cereus, vomiting). In this case, the organisms themselves
do not have to proliferate in the host for the effects of the toxin to be
manifested.
Animals and plants
constantly interact with bacteria present within their environment. For an
infection to develop, such microorganisms must remain associated with host
tissues and increase their numbers more rapidly than they can be either
eliminated or killed. This balance relates to the ability of the bacterium to
mobilize nutrients and multiply in the face of innate defences and a developing
immune response by the now compromised host.
The greater the number
of bacterial cells associated with the initial challenge to the host, the
greater will be the chance of disease. If the pathogen does not arrive at its ‘portal
of entry’ to the body or directly at its target tissues in sufficient number,
then an infection will not ensue. The minimum number of viable microorganisms
that is required to cause infection and thereby disease is called the minimum infective number (MIN). The MIN
varies markedly between the various pathogens and is also affected by the
general health and immune status of the individual host. The course of an
infection can be considered as a sequence of separate events that includes
initial contact with the pathogen, its consolidation and spread between and
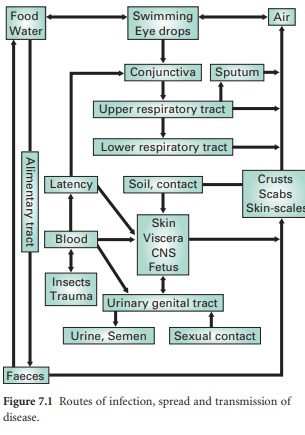
within organs and its eventual elimination (Figure 7.1). Growth and
consolidation of the microorganisms at the portal of entry commonly involves
the formation of a microcolony (biofilm), Biofilms and microcolonies are collections
of microorganisms that are attached to surfaces and enveloped within
exopolymers (biofilm matrix) composed of polysaccharides, glycoproteins and/or
proteins. Growth within the matrix not only protects the pathogens against
opsonization and phagocytosis by the host but also modulates their
micro-environment and reduces the effectiveness of many antibiotics. The
localized high cell densities present within the biofilm communities also
initiate production, by the colonizing organism, of extracellular virulence
factors such as toxins, proteases and siderophores (low molecular weight
ligands responsible for the solubilization and transport of iron (III) in
microbial cells). These are associated with a phenomenon termed quorum sensing and help the pathogen to combat the host’s innate defences and also promote the acquisition of
nutrients.
Related Topics
