Parturition (Birth)
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Pregnancy and Development
Rhythmic muscular contractions begin moving from the top to the bottom of the uterus, which is the beginning of true labor.
Parturition
(Birth)
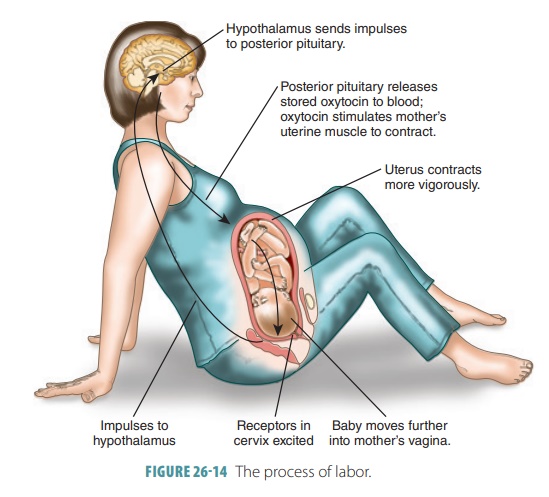
Pregnancy ends with the birth process, which begins hours or
days before birth. The act of giving birth is called labor. Progesterone declines and contrac-tions are no longer
suppressed. A prostaglandin is synthesized that promotes these contractions as
the cervix thins and opens. Late in pregnancy, the uter-ine and vaginal tissues
stretch. Nerve impulses are initiated to the hypothalamus, signaling oxytocin to be released from the posterior
pituitary gland. This hormone stimulates powerful uterine contrac-tions, aiding
in the later stages of labor. A false
labor occurs when irregular spasms occur in the uterine musculature.
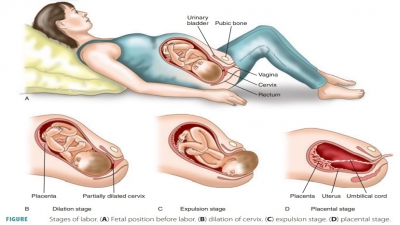
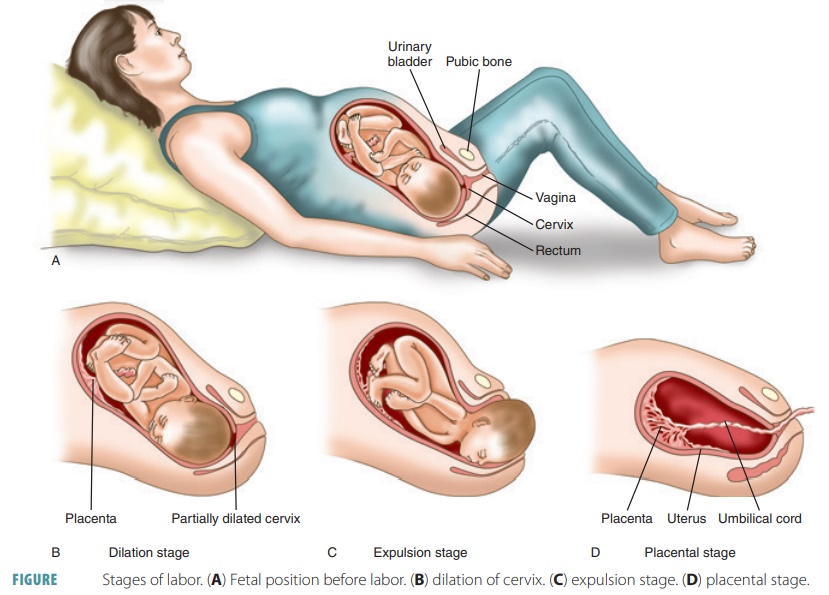
Stages of Labor
Rhythmic muscular contractions begin moving from the top to
the bottom of the uterus, which is the beginning of true labor. A positive feedback system is used to increase uterine
contraction strength. The cervix continues to dilate and more oxytocin is
released. Abdominal wall muscles con-tract, helping to force the fetus through
the cervix and vagina.
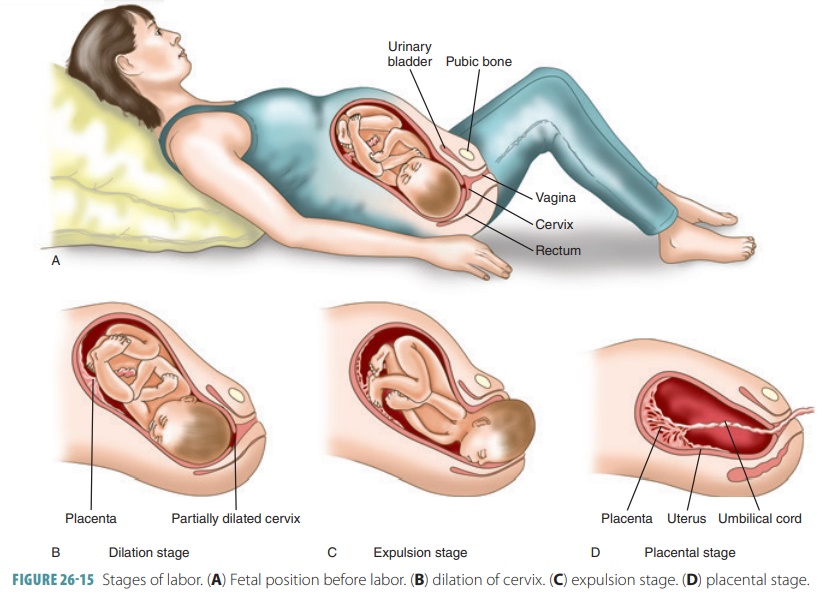
The Dilation Stage
The first stage of labor is the dilation of the cer-vix. It begins with the onset of true labor. The
fetus begins to move toward the cervical canal because of gravity and uterine
contractions. In the normal position, the fetus’ head is forced against the
cer-vix (FIGURE 26-14). This
stimulates even stronger labor contractions. Though the dilation stage can be
of variable length, most commonly it lasts for eight or more hours. When it
begins, labor contrac-tions occur once every 10–30 minutes and last up to 30
seconds each. Their frequency is steady. Later in this stage, the mother’s
“water breaks,” which is when the amniochorionic
membrane ruptures. If this should happen prior to other events of the
dilation stage, the fetus could develop an infection. If this risk is
significant, labor may be induced.
The Expulsion Stage
The second stage, called the expulsion stage, is when the fetus emerges from the
vagina. The cer-vix is pushed open and reaches a dilation of about 4 inches (10
cm). Contractions reach their maximum intensity, lasting for 60 seconds each
and occurring in 2–3 minute intervals. This stage continues until the fetus
emerges from the vagina. Usually, it lasts for less than two hours. The term delivery is used to describe the
emergence of the infant to the out-side environment, and is commonly known as birth. If the fetus cannot pass through
the vaginal canal because it is too narrow, an episiotomy may be per-formed, which temporarily enlarges the
passageway by cutting through the perineal musculature. The episiotomy prevents
the mother from experienc-ing jagged perineal tearing and can be sutured back
together easily after the birthing process is complete. When complications
occur during dilation or expul-sion, the infant can be delivered by cesarean section (C section). An
incision is made through the wall of the abdomen and the uterus is opened wide
enough to allow the infant’s head to pass. C sections today represent nearly
one-third of all live births.
After the birth of a newborn, health is assessed in five
ways: breathing, heart rate, skin color, muscle tone, and reflex response.
These are assessed in an Apgar score,
with each component given a score of between
0 and 2. A total score of 8–10 indicates the baby is healthy.
The Placental Stage
The final or placental
stage is when the placenta is expelled from the uterus. Once the fetus has been
born, the placenta separates from the uterine wall and is expelled through the
birth canal. This expul-sion is known as afterbirth
and is accompanied by bleeding because of the separation from the uter-ine
wall, which damages vascular tissues. Oxyto-cin compresses the bleeding vessels
and minimizes blood loss. Later, breastfeeding also contributes to returning
the uterus to its original size via stimula-tion of oxytocin release from the
posterior pituitary. FIGURE
26-15 illustrates the three stages of childbirth: dilation of the cervix, expulsion of the fetus,
and placental birth.
Multiple Births
Multiple births include twins, triplets, quadruplets, quintuplets, and more. Fraternal twins are clinically termed dizygotic and develop when two separate oocytes are ovulated and fertilized. Dizygotic twins occur in 70% of twin births. Identical twins are clin-ically termed monozygotic and develop when either the blastomeres separate early in cleavage or because of the splitting of the inner cell mass before gas-trulation. These twins have identical genetic make-ups because they are both formed from the same pair of gametes. Less commonly, conjoined twins may develop because of an incomplete splitting of blastomeres or the embryonic disc. Formerly known as Siamese twins, the conjoined infants often share certain organs, and the ability to be surgically sepa-rated is uncertain. Overall, twins are more common than triplets, which are more common than quadru-plets, and so on.
Premature Labor
When true labor begins prior to the fetus completing normal
development, premature labor occurs.
The chance of the newborn surviving is based on its body weight at the time of
delivery. Newborns weighting less than 14 ounces (400 g) at birth will not
survive, even with significant supportive efforts. This is mostly due to the
inability of their cardiovascular, respiratory, and urinary systems to support
life without help from the maternal systems. Therefore, a dividing line has
been set between spontaneous abortion and immature
delivery at 17.5 ounces (500 g),
which is the normal weight close to
the end of the second trimester.
The majority of fetuses born between weeks 25 and 27 of
gestation, which constitutes a birth weight of under 21.1 ounces (600 g), die,
even with intensive care measures. Those that survive have a significant risk
of development abnormalities. The term pre-mature
birth usually refers to birth at 28–36 weeks of development, with a birth weight of more than 2.2 pounds (1
kg). With sufficient care, these newborns have a good chance of survival and
nor-mal development.
Difficult Deliveries
For most pregnancies, at the end of gestation, the fetus has
rotated inside the uterus so that the infant’s head faces the birth canal and
mother’s sacrum. In about 6% of deliveries, the fetus faces the mother’s pubis.
They can be delivered normally if there is enough time, though risks to the
infant and mother are less-ened by a forceps
delivery. Forceps look like large salad tongs that are curved. They are
separated for insertion into the vaginal canal one side at a time. When they
are in place, they are reunited, and can grasp the head of the fetus. The
amount of pull applied with the for-ceps is described as intermittent, and resembles the forces upon the infant’s head that
occur during nor-mal delivery.
In only 3% to 4% of deliveries, a breech birth occurs, in which the infant’s legs or buttocks enter
the vaginal canal before the head. Breech births have higher risks of harm to
the infant. This is primarily because the umbilical cord can become constricted
and cut off placental blood flow. Normally, the widest part of the fetus is the
head. Sometimes, the moth-er’s cervix dilates enough to pass the baby’s legs
and body, but not the head. This can compress the umbilical cord, lengthen
delivery, and cause severe fetal distress or injury. When attempts to
reposition the fetus or promote additional dilation do not work over a short
period of time, delivery by C section may be indicated.
1. Describe the developmental milestones of the fetal period.
2. What are the significant components of fetal blood?
3. Explain
the stages of labor.