Chemotherapy - Control of Protozoan Parasites
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Protozoa
The origins of chemotherapy are closely linked to the development of antiparasitic agents, but there has been slow progress in the development of new and novel antiprotozoal agents over the past 30 years.
CHEMOTHERAPY
The origins of chemotherapy
are closely linked to the development of antiparasitic agents, but there has
been slow progress in the development of new and novel antiprotozoal agents
over the past 30 years. Recently, with the support of the WHO and government sponsored
research, new antiparasitic drugs are slowly coming into the market.
Interestingly there are still a number of protozoan parasite infections such as
cryptosporidiosis for which there is no effective treatment.
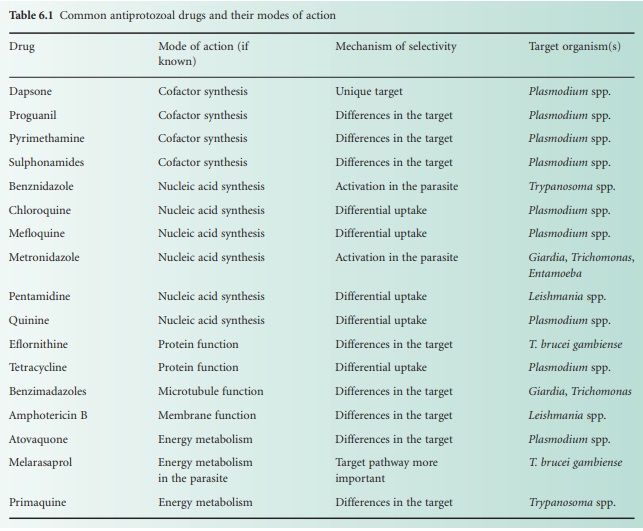
Mechanisms of action and selective toxicity
For many of the commonly
used antiprotozoal drugs the modes of action and mechanisms of selective
toxicity are well understood, although for some the precise mechanism remains
unclear. The most common antiprotozoal drugs and their modes of action are shown
in Table 6.1.
Considering the drugs in
relation to modes of action, dapsone and the sulphonamides block the
biosynthesis of tetrahydrofolate by inhibiting dihydropteroate synthetase,
while the 2,4diaminopyrimidines (proguanil and pyrimethamine) block the same
pathway but at a later step catalysed by dihydrofolate reductase.
The drugs that interfere
with nucleic acid synthesis include those that bind to the DNA and intercalate
with it such as chloroquine, mefloquine and quinine, and also pentamidine, which
is unable to intercalate but probably interacts ionically. Other compounds such
as benznidazole and metronidazole may alkylate DNA through activation of nitro
groups via a one-electron reduction step. Several of these compounds, however,
including chloroquine, mefloquine, quinine and metronidazole, have more than
one potential mode of action. Chloroquine, for example, inhibits the enzyme
haem polymerase, which functions to detoxify the cytotoxic molecule haem that
is generated during the degradation of haemoglobin. Metronidazole is reduced in
the parasite cell and forms a number of cytotoxic intermediates, which can
cause damage not only to DNA but also to membranes and proteins.
Tetracycline targets
protein synthesis in Plasmodium via a
similar mechanism to that seen in bacteria: inhibition of chain elongation and
peptide bond formation. Eflornithine interferes with the metabolism of the
amino acid ornithine in T. brucei
gambiense by acting as a suicide substrate for the enzyme ornithine
decarboxylase.
Albendazole has recently
been shown to have significant anti-giardial activity, although its mode of action
is unclear. In Leishmania,
amphotericin B binds to ergosterol in the membrane making it leaky to ions and
small molecules (e.g. amino acids), while the anti protozoal drugs atovaquone and primaquine bind
to the cytochrome bc 1 complex and inhibit electron
flow. The anti-trypanosomal drug melarsaprol is most likely to act by blocking
glycolytic kinases, especially the cytoplasmic pyruvate kinase, although it may
also disrupt the reduction of trypanothione.
Drug resistance
As with bacteria, drug
resistance in some parasites such as Plasmodium
is a major problem and tends to appear where chemotherapy has been used
extensively. This problem is exacerbated by the fact there are so few drugs
available for the control of some parasites, which utilize the same five basic
resistance mechanisms that are displayed by bacteria: (1) metabolic
inactivation of the drug; (2) use of efflux pumps; (3) use of alternative
metabolic pathways; (4) alteration of the target; (5) elevation of the amount
of target enzyme.
Related Topics
