Antitubercular Antibiotics
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Antibiotics And Synthetic Antimicrobial Agents: Their Properties And Uses
The antibiotics used for the treatment of tuberculosis belong to a variety of chemical classes, but it is convenient to consider them together in the same section..
ANTITUBERCULAR ANTIBIOTICS
The antibiotics used for the treatment of tuberculosis
belong to a variety
of chemical classes,
but it is convenient to consider them
together in the same section
for two reasons: first, most
of them are used exclusively for tuberculosis, and
second, therapy extends
over several months, during which time resistance development is a significant
possibility. This risk is minimized by the use of two or
three antibiotics in combination, so it is appropriate to consider them together because that
represents their normal
pattern of use.
Streptomycin, introduced in the late 1940s,
was the
first effective treatment for tuberculosis, but
its use in isolation was short lived
because of the ease with which the bacteria
became resistant to a single antibiotic.
Isoniazid, which became
available about 5 years later, was used first in combination with streptomycin then with
rifampicin after the latter was introduced in 1967. The combination of isoniazid and rifampicin has
been the mainstay of tuberculosis therapy
from that time until the present
day, although other drugs like pyrizinamide and ethambutol have been added
to the combination, and multidrug-resistant tuberculosis has become an increasing problem in recent years;
this is, by definition,
simultaneous resistance to isoniazid and rifampicin.
Tuberculosis
may be caused by any
one of three Mycobacterium
species, but all three
characteristically grow slowly in the body and may persist for long periods in a near dormant
state. Because the course of therapy is normally 4–6 months,
antibiotics that are orally effective are much preferred; this is because
unsupervised patients are more likely
to take oral
medicines, and in many countries
where patients may have difficulty travelling to clinics the daily
administration of injectable antibiotics
is not feasible. The ideal antitubercular drug should also have
the potential to kill rather
than merely inhibit the
growth of the infecting organism. Because mycobacteria can survive, and even reproduce, within macrophages, relying on the immune system to eradicate
an infection
following the use of a bacteristatic drug is
unlikely to be an effective strategy.
Rifampicin kills dormant bacteria, while pyrizinamide is active against bacteria that are slowly
reproducing in acidic
environments; isoniazid is most useful against more rapidly growing cells.
The current approach is
to treat tuberculosis in two phases:
an initial phase of 2 months using isoniazid, rifampicin and pyrizinamide (with
or without ethambutol), and a
4 month continuation phase with isoniazid and rifampicin. If, however,
the infecting organism
is resistant to any of the above,
second-line drugs may be
used and the duration of treatment possibly
extended. The status
of streptomycin is equivocal; it is now rarely
used in the UK and is not a first-choice treatment recommendation of the European
Respiratory Society either,
but it is more commonly
used in front-line therapy in the USA. Second-line drugs
available for infections caused by resistant organisms, or when first-line drugs cause unacceptable side effects, include amikacin, capreomycin, cycloserine, newer macrolides
(e.g. azithromycin and clarithromycin) and moxifloxacin. Drug regimens are
often indicated using a shorthand notation with single letters to indicate the drugs employed, initial numbers indicating
months of therapy and following numbers (which
may be in parentheses or subscripts) indicating days per week. For example, 2RHZ(E)/4HR(3) or 2RHZ(E)/4HR3 would mean 2 months of rifampicin, isoniazid and pyrizinamide (with the possible
addition of ethambutol) followed by 4 months of isoniazid and rifampicin three times
per week. Several
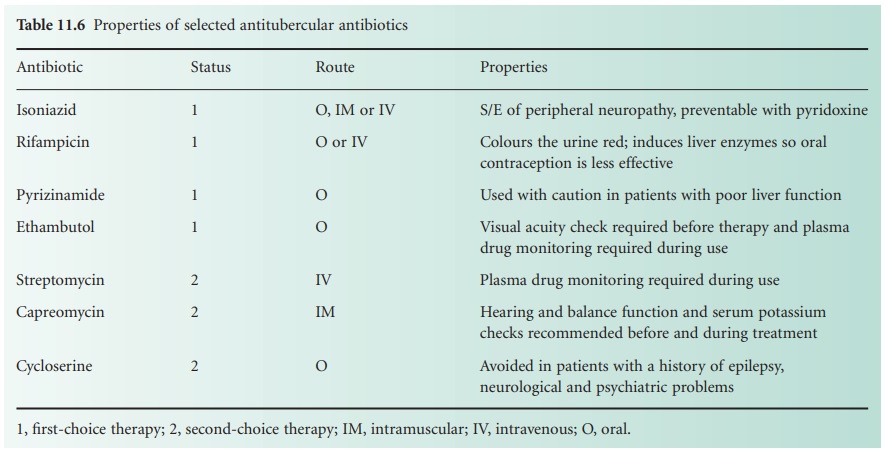
of the antitubercular drugs have specific contraindications or require monitoring during
use; some of these requirements and cautions are shown in Table 11.6.
Rifampicin is the only
one of the common antitubercular drugs that is used in the treatment of
non-mycobacterial infections. It is active
against Gram-positive bacteria and some Gram-negative species, but not
Enterobacteriaceae or
pseudomonads. Rifampicin possesses significant bactericidal activity at very low concentrations against staphylococci.
Unfortunately, resistant mutants may arise
very rapidly, both
in vitro and in vivo, so it has been recommended that rifampicin should be
combined with another antibiotic, e.g. vancomycin, in the
treatment of staphylococcal infections. Rifabutin, a semisynthetic
rifamycin, may be used in the prophylaxis of M.
avium complex infections in immuno-compromised patients and in the treatment, with other drugs,
of pulmonary
tuberculosis and non-tuberculous mycobacterial infections.
Related Topics
