Antifungal Antibiotics
| Home | | Pharmaceutical Microbiology | | Pharmaceutical Microbiology |Chapter: Pharmaceutical Microbiology : Antibiotics And Synthetic Antimicrobial Agents: Their Properties And Uses
There has been a significant increase in the number of both systemically and topically acting antifungal agents in recent years; this has been prompted in part by the increase in patients with impaired immunity who are particularly vulnerable to such infections. For much of the second half of the 20th century nystatin, amphotericin and griseofulvin were the principal antifungal antibiotics available.
ANTIFUNGAL
ANTIBIOTICS
There has been a significant increase
in the number of both systemically and topically acting
antifungal agents in recent
years; this has been prompted
in part by the increase in
patients with impaired immunity who are
particularly vulnerable to such infections. For much of the
second half of the 20th
century nystatin, amphotericin and griseofulvin were
the principal antifungal antibiotics available, and these were supplemented with a
range of synthetic
imidazoles which were used primarily for superficial rather than systemic
fungal infections. The introduction
of the triazole
antifungals in the 1980s was a major
advance and, more
recently, the echinocandins have further increased the range of drugs available
for severe infections.
Lack of toxicity is, as
always, of paramount importance, but
the differences between
bacterial and fungal cells in both structure and biosynthetic
processes mean that the low-toxicity antibacterial antibiotics are usually inactive against fungi.
This limitation is further complicated by the fact that both fungal and human cells are
eukaryotic in structure, which means that
there are few differences
that can be exploited in order to achieve selective
toxicity towards fungi whilst leaving
the human cells unharmed. Fungal infections are normally less
virulent in nature than are bacterial or viral ones but may, nevertheless, pose major treatment problems in individuals with a depressed
immune system, particularly in the case of systemic
infection.
A)
AZOLES
The azoles
may be considered as two subgroups: the older
imidazole drugs,
the majority of which were introduced
as topical
products or pessaries for the treatment of superficial infections by dermatophytes (skin
pathogens), Pityriasis species (causing flaky
skin and dandruff) and C. albicans, and the more recently developed, more versatile and, in some
cases, much more
expensive, triazoles.
a)
Imidazoles
The imidazoles are a large
and diverse group
of compounds with activity
against bacteria and protozoa (metronidazole and tinidazole), helminths
(mebendazole) and fungi (clotrimazole, miconazole, ketoconazole, econazole,
sulconazole and tioconazole). Table 11.8 lists infections for which the common
antifungal drugs are employed; other imidazoles are available in various countries.
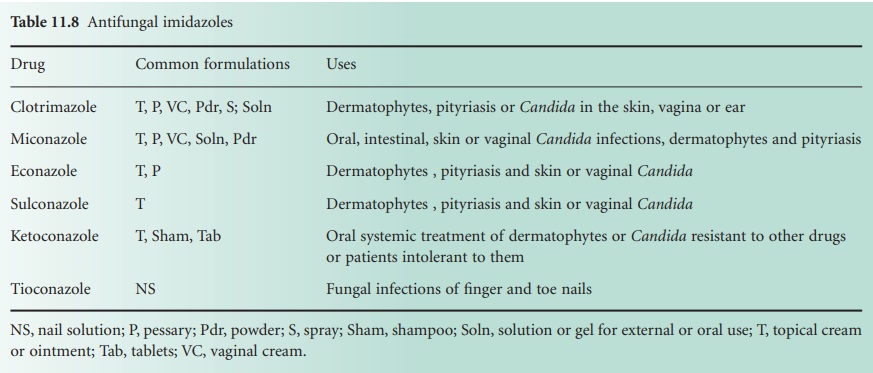
As Table 11.8 indicates, the imidazoles are available in a wide variety
of dosage forms,
but most of them have the same uses. They exhibit
modest activity against
some Gram-positive bacteria, but they are all essentially fungistatic drugs which
might exert fungicidal action during prolonged exposure to high concentrations.
Miconazole may be given orally
for the treatment of intestinal fungal infections, and in this
situation may show
some absorption into the systemic
circulation, although this may be more
of a problem from the perspective of potential drug interactions than a benefit. Ketoconazole, however,
achieves
greater absorption from the gastrointestinal tract, but it has been largely superseded by newer and less
toxic drugs
so its use tends to be restricted to situations where resistance or patient intolerance to those drugs
is a problem.
b)
Triazoles
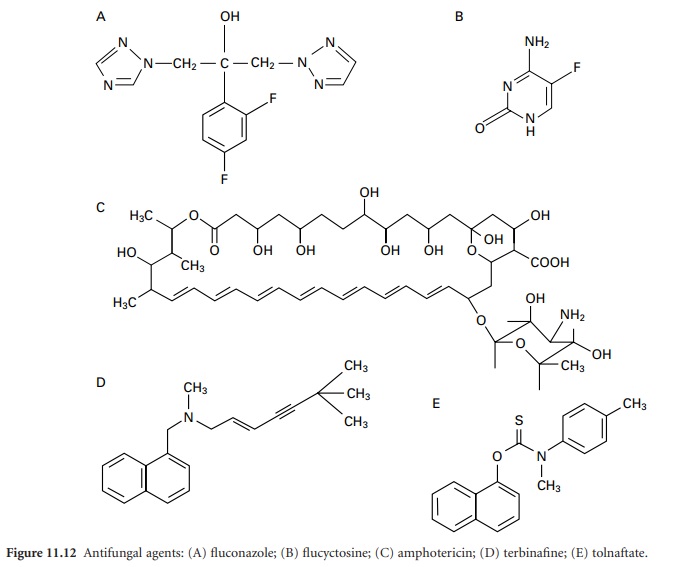
Fluconazole (Figure
11.12A) and itraconazole were introduced in the 1980s and
posaconazole and voriconazole much more recently. The two earlier
drugs are more widely used, whilst
the recent ones tend to be reserved
for severe, possibly life-threatening infections, in which
other antibiotics have failed
or are inappropriate. All four of the
triazole drugs are orally active
and all but posaconazole
are available in
injection form.
Fluconazole is better
absorbed from the gastrointestinal tract than
itraconazole and, in addition to the treatment of dermatophytes, pityriasis and Candida infections, it is valuable in cases of cryptococcosis which,
although uncommon, is very
dangerous in immunocompromised patients. Itraconazole is used for similar infections to fluconazole but, in addition, it is more commonly selected as an alternative to amphotericin (see below) in cases of systemic Aspergillus infection (again, more common in
the immunocompromised) and other rare systemic mycoses. It is more frequently associated with liver toxicity
than fluconazole.
B)
POLYENES
Polyene antibiotics are characterized by possessing a large
ring containing a lactone group and a hydrophobic
region consisting of a sequence
of four to seven conjugated double bonds. The only
important polyenes are amphotericin B and nystatin.
Amphotericin B (Figure 11.12C)
is active against
most fungal pathogens and is used
for systemic mycoses
as a potentially more toxic, but possibly more
effective, alternative to itraconazole. It is poorly
absorbed from the gastrointestinal tract and is thus usually
administered by intravenous injection
under strict medical supervision. Lipid-based and liposomal formulations of
amphotericin are available which exhibit lower toxicity than conventional aqueous formulations; they may therefore be given in higher doses. Nystatin is administered orally
in the treatment of C. albicans infections in the intestine or the mouth (often referred
to as thrush), and by cream or pessary for skin
or vaginal infections by that organism. It is rarely used for the treatment of other infections and is too toxic to be given by injection.
C) ECHINOCANDINS
The echinocandins are a new class of semisynthetic
lipopeptide antibiotics that are fungicidal towards
Aspergillus spp., Candida spp. and Pneumocystis jirovecii (previously known as P. carinii). Caspofungin, the first member of the class,
is given as an intravenous infusion recommended for invasive aspergillosis or candidiasis that
is unresponsive to treatment with amphotericin or itraconazole. Anidulafungin and micafungin are similarly injectable products
licensed for the treatment
of invasive
candidiasis, and they, like caspofungin, tend to be used as reserve drugs,
both to minimize the risk of resistance development and due to cost
considerations.
D)
OTHER ANTIFUNGAL AGENTS
Flucytosine (5-fluorocytosine, Figure 11.12B) is a narrow-spectrum antifungal agent with
greatest activity against yeasts such as Candida, Cryptococcus and
Torulopsis. It is normally used in combination with fluconazole or as a synergistic combination with amphotericin which permits amphotericin dose
reduction and a lower risk
of toxicity. Terbinafine (Figure
11.12D), a member of the allylamine class
of antimycotics, is orally active,
fungicidal, effective against
a broad range of dermatophytes and yeasts and is the drug
of choice for fungal nail
infections. Griseofulvin too is employed
for the treatment of dermatophyte infections of hair, skin and nails, but usually only when topical therapy
has failed, and with the exception of Trichophyton infections in children, it is no longer regarded as a drug
of choice. It is orally
active, although the particle size of the powder used to manufacture the tablets
has a significant effect on bioavailability. Tolnaftate (Figure 11.12E) is a synthetic thiocarbamate which is used topically in the treatment or prophylaxis of tinea (commonly referred to as ringworm, although not due to worms
at all) and amorolfine is used as a cream or nail lacquer for the same purpose.
Related Topics
