Anatomy of the Male Reproductive System
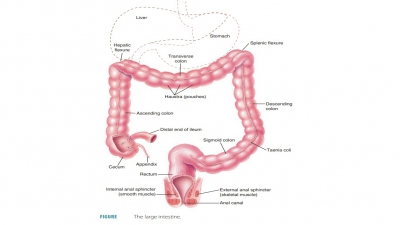
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Reproductive System
Anatomy and Structure of Scrotum, Testes, Penis, Male Duct System, Male Accessory Glands, Semen
Anatomy
of the Male Reproductive System
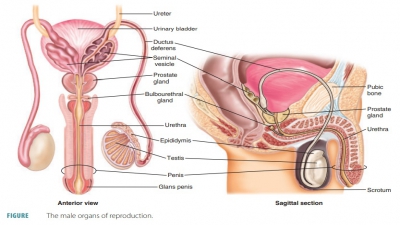
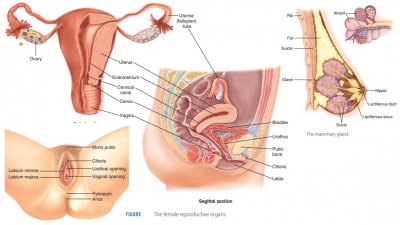
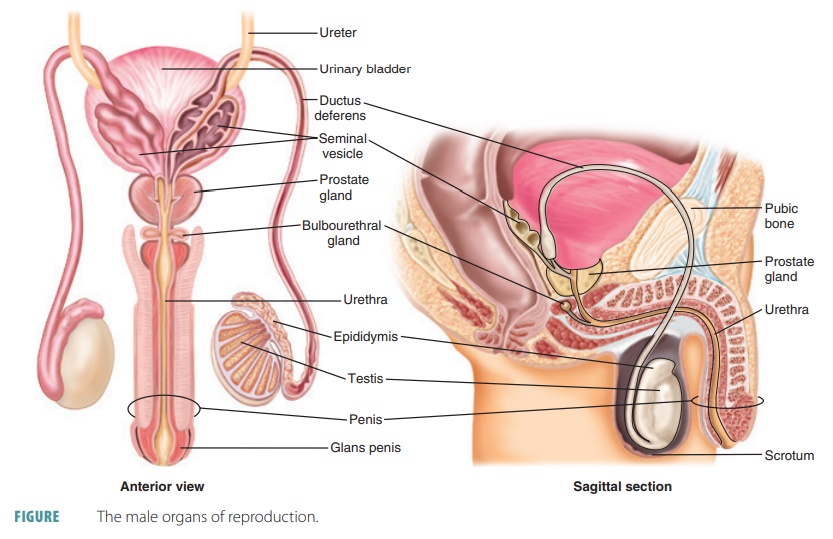
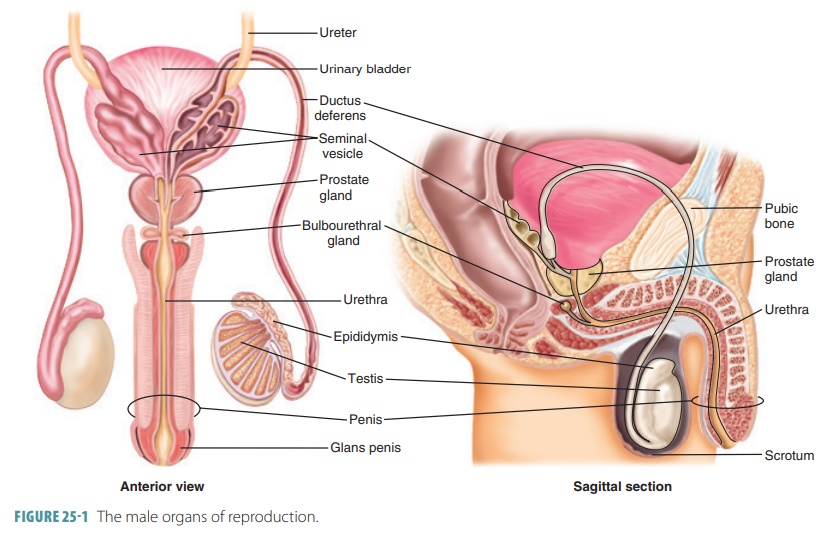
The structures of the male reproductive system include two
epididymides, two ductus deferentia, two ejacula-tory ducts, the urethra, two
seminal vesicles, the pros-tate gland, and two bulbourethral glands. Sperm
cells are produced and maintained by the male reproduc-tive organs, which also
transport these cells outside the body and secrete male sex hormones. The
primary sex organs or gonads of the
male consist of the two tes-tes, in which sperm cells and male sex hormones are
formed. The accessory sex organs are the internal and external reproductive
organs (FIGURE 25-1).
Scrotum
The male external reproductive organs consist of the scrotum and the penis. The
scrotum consists of a flesh pouch
of skin and subcutaneous tissue suspended below the perineum and anterior to
the anus. The scro-tum encloses the testes. Sparse hairs cover the scrotum
externally. Internally, the medial septum or raphe sub-divides it into two chambers, each enclosing a testis.
The scrotum protects and controls the temperature of the testes, which is
important for sex cell production.
When environmental temperatures are cold, the scrotum
contracts and wrinkles, moving the testes closer to the pelvic cavity to absorb
heat. When it is warmer outside, the scrotum relaxes and hangs loosely to
ensure the testes are about 3°C lower than body temperature. This is better for
the sperm cells to be produced and to survive. Viable sperm cannot be produced
at normal core body temperature, which is 98.6°F (37°C).
The scrotum contains two sets of muscles that respond to
temperature changes. Each dartos
muscle is a smooth muscle layer in the superficial fascia that acts
to wrinkle the scrotal skin. Bands of skeletal mus-cle arising from the
internal oblique muscles of the body’s trunk are known as the cremaster muscles, which act to elevate the testes
toward the body, to con-trol scrotal temperature.
Testes
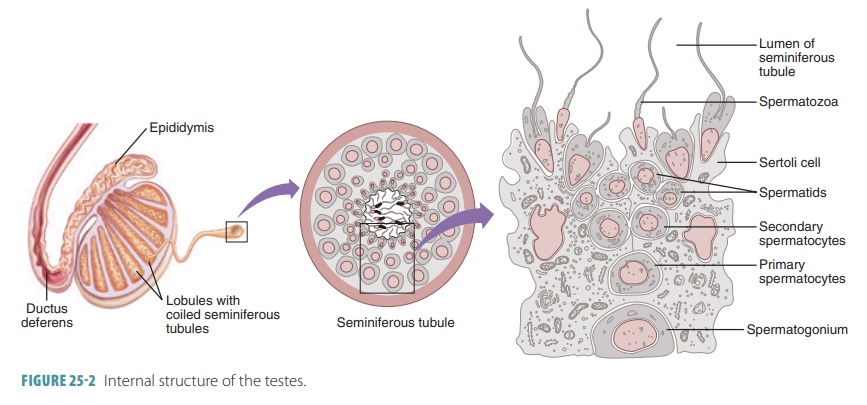
The testes are
oval-shaped structures, about 4 cm (1.5 inches) long and 2.5 cm (1 inch) wide,
located within the cavity of the scrotum. Each testis is also enclosed in two
tunics. The outer is the tunica vaginalis, which has two serous
layers and is formed from
a peritoneal outpocket. The inner tunic is the tunica albuginea and is a
fibrous capsule. Thin septa extend inward from the tunica albuginea and divide
the testis into approximately 250 lobules. Each wedge-shaped lobule contains
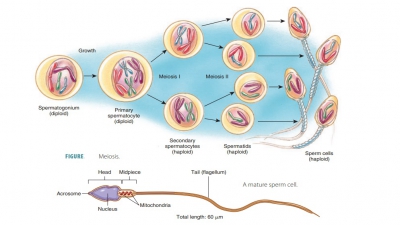
one to four highly coiled seminiferous tubules that, when uncoiled, may reach 80 cm in length. It is here where sperm are
actually formed. The seminiferous tubules are made up of a thickened stratified
epithelium that surrounds a central lumen filled with fluid. Spermatogenic cells are found in larger columnar cells known as sustenocytes. These cells play a
variety of roles in sperm formation.
Sperm are generated continuously. The sustenocytes maintain the blood-testis
barrier, support spermiogenesis, secrete inhibin hormone, and secrete
androgen-binding protein.
A normal testis contains nearly one-half of a mile of seminiferous
tubules. Each of these tubules forms a loop connected to a network of
passageways known as the rete
testis. Fifteen to 20 large efferent
ductules connect the rete testis to the epididymis.
This tube coils on the outer surface of the testis and becomes the ductus
deferens (FIGURE 25-2). Three
to five layers of myoid
cells, which resemble smooth muscle cells, surround each
seminiferous tubule. Rhythmic con-tractions of the myoid cells aid in squeezing
sperm and testicular fluids through the seminiferous tubules and out of the
testes. The rete testis receives sperm through a straight tubule formed by the seminiferous tubules
of each lobule, which leads into the epididymis for the maturation of sperm.
The epididymis wraps around the posterior external surface of each testis.
Immature sperm pass through the head and body of the epidid-ymis to be stored
in its “tail” portion until ejaculation.
Interstitial
endocrine cells, also known as Leydig
cells, lie inside the soft connective tissue that
surrounds the seminiferous tubules. They produce testosterone and less
important types of androgens. These substances are secreted into the
surround-ing interstitial fluid. The testes are supplied by long testicular arteries that branch from the
abdominal aorta, superior to the pelvis. The testes are drained by the testicular veins, which arise from a network known
as the pampiniform venous plexus. This
network surrounds each testicular artery inside the scrotum, winding around it.
In each pampiniform plexus, cooler venous blood absorbs heat from arterial
blood. Therefore, this blood becomes cooler before entering the testes, which
helps to keep the testes at their normal, cool, homeostatic temperature.
The testes are served by the sympathetic and para-sympathetic divisions of the autonomic nervous sys-tem. Forceful trauma to the testes transmits impulses, causing intense pain and nausea. In the testes, blood vessels, nerve fibers, lymphatic vessels, and the ductus deferens are enclosed by a connective tissue sheath. Together, these structures comprise the spermatic cord passing through the inguinal canal.
1. Explain the role of the scrotum in protection of the
testes.
2. Describe the two major functions of the testes.
3. Identify the structures in which sperm are actually formed.
Penis
The penis is
cylindrical in shape and conveys urine and semen through the urethra. When
erect, it stiff-ens and enlarges, enabling insertion into the vagina during
sexual intercourse. The penis is divided into three regions: the root, body,
and glans or glans penis.
The root of the penis is the fixed portion that attaches the penis to the body wall. At birth,
skin that covers the penis is loose. It slides distally over the head, forming
the foreskin or prepuce around the glans. The prepuce is
often removed surgically soon after birth in a procedure called a circumcision. This practice is more
common in the United States, where at least 65% of males are circumcised. In
the rest of the world, about 30% of males experience this procedure. Many
cultures are not familiar with circumcision, including some Hispanic cultures
and many European and Asian cultures. Most males from Muslim and Jew-ish
cultures are circumcised. It is widely believed that circumcision reduces risk
of acquiring HIV or other reproductive system infections.
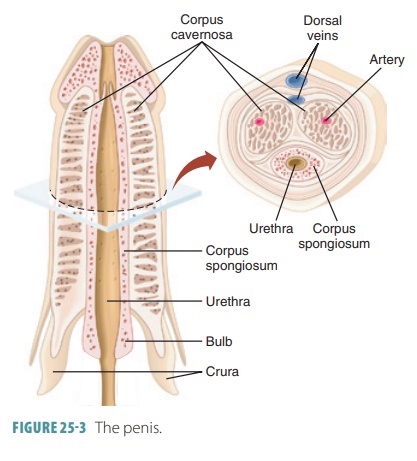
The dorsal and ventral surfaces of the penis are actually
named in relation to the penis being erect, not flaccid. The shaft or body of the penis is the tubular, movable
portion of the organ. It contains three columns of erectile tissue. It has two
dorsal corpora cavernosa and one ventral corpus spongiosum (FIGURE 25 -3). The corpora cavernosa
is the erectile tis-sue that is located on the anterior surface of the penis.
The urethra is surrounded by the corpus spongiosum. Dense connective tissue
surrounds each column in a capsule. The penis is enclosed by a layer of
connective tissue, a thin layer of subcutaneous tissue, and skin. The erectile
tissue of the penis contains many vascular spaces. These spaces fill with blood
during sexual stimulation.
Male
Duct System
When sperm are produced by the testes, they move out of the
body via a system of ducts. These ducts are the epididymis, ductus deferens,
ejaculatory duct, and urethra.
Epididymis
The cup-shaped epididymis can be
felt through the skin of the scrotum. It is coiled and twisted to take up only
a small amount of space, about 3.8 cm or 1.5 inches. The head of the epididymis
contains effer-ent ductules and lies above the superior aspect of each testis.
The body and tail of the epididymis are found on the posterolateral area of
each testis.
The epididymis controls the composition of the fluid
produced by the seminiferous tubules. It also absorbs and recycles damaged spermatozoa
and absorbs cellular debris. The products of the break-down of enzymes are
released into the surrounding interstitial fluids for pickup by the epididymal
blood vessels. The epididymis also stores and protects sper-matozoa and
facilitates their functional maturation.
Most epididymides are tightly coiled tubes about 6 m or 20
feet in length, connected to the posterior border of the testes. These tubes
are also described as the ducts of
the epididymides. They course upward to become the ductus deferens. In the
duct mucosa, certain pseudostratified epithelial cells have stereocilia, which are long, nonmoving
microvilli. Having a large surface area, the stereocilia can absorb extra
testicular fluid and pass nutrients to the millions of sperm cells temporarily
stored in the lumen.
Immature sperm cells are nonmotile when they reach the epididymis; therefore, rhythmic peristal-tic contractions move them through the duct as they mature. The surrounding fluid contains antimicrobial proteins such as defensins. The transfer of sperm from the testes and through the epididymides takes approx-imately 20 days. Once mature, sperm cells can move independently to fertilize egg cells, but usually do not actually “swim” until after ejaculation. This occurs from the epididymides and not the testes. The secretions of the seminal vesicles are discharged into the ejaculatory duct at emission. This is when peristaltic contractions are occurring in the ductus deferens, seminal vesicles, and prostate gland. These contractions are controlled by the sympathetic nervous system. Although sperm are normally stored in the epididymides for several months, longer storage results in them being phagocy-tized by the epithelial cells there.
Ductus Deferens and Ejaculatory Duct
The ductus
deferentia, also called the vasa
deferentia, are muscular tubes
approximately 45 cm (18 inches) in
length. Singularly, each ductus defer-ens is called a vas deferens. They each pass upward, as part of the spermatic cord,
along the medial side of a testis, through the inguinal canal in the lower
abdominal wall to enter the pelvic cavity. They end behind the urinary bladder,
uniting just outside the prostate gland with the duct of a seminal vesicle.
This forms an ejaculatory
duct, which is a short structure passing through the prostate
gland to empty into the urethra. The vas deferens is the duct that is altered
when a male undergoes a vasectomy.
Each ductus deferens can easily be felt as it passes
anterior to the pubic bone, looping medially over the ureter and descending
along the posterior wall of the bladder. The terminus portion expands to form
an ampulla, joining
the duct of a seminal vesicle. The mucosa of the ductus deferens is, like the
epidid-ymis, pseudostratified epithelium. It differs in that its muscular layer
is very thick. During ejaculation, the smooth muscle of its walls creates
peristaltic waves, quickly squeezing sperm forward into the urethra.
Male Accessory Glands
The male accessory glands consist of a pair of seminal
glands and bulbourethral glands, plus a single prostate gland.
Seminal Glands
The seminal glands are also called seminal vesicles and are sac-like structures lying
on the posterior bladder surface. They are approximately 5 cm long, attached to
the ductus deferens near the base of the bladder. Each seminal vesicle is a
tubular gland having a total uncoiled length of about 15 cm. However, these
glands are normally coiled back on themselves, mak-ing their coiled size only
5–7 cm. During ejaculation, they are emptied by a thick layer of smooth muscle
that contracts inside their fibrous capsules. They have glandular tissue
linings that contribute nearly 60% of semen volume.
The seminal vesicles secrete a slightly alkaline fluid that
is yellowish in color and viscous. This fluid helps to regulate the pH of the
tubular contents as sperm cells travel to outside the body. The yellow color of
seminal fluid comes from a pigment that becomes flu-orescent under ultraviolet
light, a fact that is used for the investigation of certain crimes. Seminal
fluid con-tains fructose, a monosaccharide that provides energy for sperm
cells, as well as prostaglandins that stimu-late muscular contractions within
the female repro-ductive organs. These contractions aid the movement of sperm
cells toward the egg cell. The fluid from the seminal glands also contains
citric acid and a coagu-lating enzyme known as vesiculase.
Remember that the duct of each seminal gland joins the duct
of the ductus deferens on the same side, forming the ejaculatory duct. Here,
seminal fluid mixes with sperm, entering the prostatic urethra simultaneously
during ejaculation. Semen, therefore,
is 70% made up by seminal gland secretions.
Prostate
The prostate
gland surrounds the proximal portion of the urethra, slightly
inferior to the urinary bladder. It is a chestnut- or doughnut-shaped, muscular
struc-ture that is approximately 4-cm wide and 3-cm thick. It is surrounded by
a thick connective tissue capsule and made up of 20–30 branched tubular glands
with ducts that open into the urethra. These glands are embedded in a stroma,
which is a mass of dense con-nective tissue and smooth muscle.
The prostatic smooth muscle contracts during ejaculation.
Prostatic secretions are squeezed into the prostatic urethra through several
ducts. The secretions consist of a milky fluid that is slightly acidic.
Prostatic fluid enhances the motility of the sperm cells and helps neutralize
the vagina’s highly acidic secretions. It makes up to one-third of the volume
of the semen. Prostatic fluid contains citrate, which provides nutri-ents,
prostate-specific antigen, and enzymes such as fibrinolysin, acid phosphatase,
and hyaluronidase.
Bulbourethral Glands
The bulbourethral
glands, also known as Cowper’s glands, are about 1 cm in diameter
and lie inferior to the prostate gland surrounded by the external urethral
sphincter muscle’s fibers. These glands have tubes with epithelial linings
secreting a thick, clear mucous-like fluid as a response to sexual stimulation.
The fluid lubricates the end of the penis to prepare for sexual intercourse,
even though females secrete most of the lubricating fluid needed for sexual
intercourse. The fluid from the bulbourethral glands also neutralizes any
urine, which is acidic.
Semen
The milky white, slightly sticky fluid the male ure-thra
conveys to outside of the body during ejacula-tion is known as semen. It is made up of sperm cells from the testes and
secretions of the seminal vesicles, prostate gland, and bulbourethral glands.
Semen has an alkaline pH of between 7.2 and 8.0, and includes prostaglandins
and nutrients. It helps to neutralize the acidic environment of the male
urethra and the female vagina. Under acidic conditions, the sperm “swim” more
slowly than normal.
Between 2 and 5 mL of semen are released at one time, with
between 20 and 150 million sperm/mL. How-ever, sperm only make up about 10% of
the semen. Sperm cells begin to swim as they mix with accessory gland
secretions. They acquire the ability to fertilize a female egg cell once they
are inside the female reproductive tract in a process called capacitation, which is due to the weakening of
the sperm cells’ acrosomal membranes.
Mature sperm do not contain significant amounts of stored
nutrients or cytoplasm. Nearly all energy needed for sperm adenosine
triphosphate synthe-sis is provided by the catabolism of fructose in sem-inal
gland secretions. The prostaglandins in semen decrease viscosity in the
femalecervix, stimulating reverse
peristalsis. This speeds up the movement of sperm through the female reproductive tract. Semen also contains
the hormone relaxin, various enzymes,
ingredients that suppress the immune response in the female reproductive tract,
antibiotics that destroy certain bacteria, and clotting factors. Just after
ejacu-lation, the clotting factors coagulate the semen, which causes the sperm
to stick to the vaginal walls of the female so they do not drain out of the
vagina. Fibri-nolysin then liquefies the sticky mass, allowing the sperm to
swim along their journey to the ovum.
Related Topics