Vitamin D
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs Affecting Calcium Balance
Vitamin D is the collective name given to antirachitic substances synthesized in the body and found in foods activated by UV radiation.
VITAMIN D
Vitamin D is the
collective name given to antirachitic substances synthesized in the body and
found in foods activated by UV radiation.
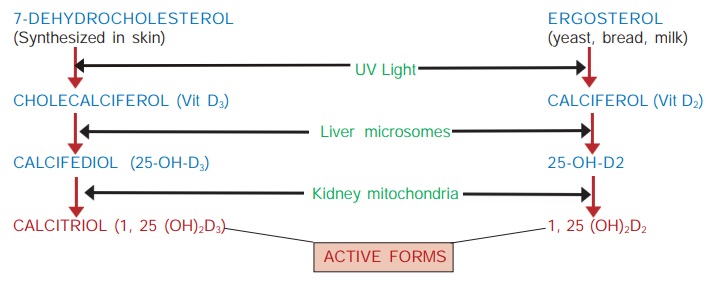
D3 : cholecalciferol — synthesized in the skin under
the influence of UV rays.
D2 : calciferol—present in irradiated food— yeasts,
fungi, bread, milk.
D1 : mixture of antirachitic substances found in food—only
of historic interest.
In 1919 it was
established that rickets was due to deficiency of a dietary factor as well as
lack of exposure to sunlight. McCollum (1922) showed that this fat soluble
dietary factor was different from vit A and its structure was determined in
1935. The interrelation between calciferol and cholecalciferol and their
activation in the body has been fully understood only in the 1970s.
Activation of Vit D
It takes place in the following manner—
Ergosterol differs
from 7dehydrocholesterol in having an extra double bond between C22–23 and a
methyl group at C24. In man vit D2 and D3 are equally
active and calcitriol (active form of
D3) is more important physiologically; 25OH D3 is
released in blood from the liver and binds loosely to a specific vit D binding
globulin. The final hydroxylation in kidney is rate limiting and is controlled
by many factors. This step is activated or induced by calcium/vit D deficiency
as well as by PTH, estrogens and prolactin, while calcitriol inhibits it in a
feedback manner.
Thus, vit D should be considered a hormone because:
a) It is synthesized in
the body (skin); under ideal conditions it is not required in the diet.
b) It is transported by
blood, activated and then acts on specific receptors in the target tissues.
c) Feedback regulation of
vit D activation occurs by plasma Ca2+ level and by the active form itself.
Actions
1. Calcitriol enhances
absorption of calcium and phosphate from intestine.
This is brought about by increasing the synthesis of calcium channels and a
carrier protein for Ca2+ called ‘calcium binding protein’ (Ca BP) or Calbindin. The action of calcitriol is
analogous to that of steroid hormones. It binds to a cytoplasmic vitamin D
receptor (VDR) → translocate to the nucleus → increase synthesis of
specific mRNA → regulation of protein
synthesis. Another line of evidence suggests that activation of VDR promotes
endocytotic capture of calcium and transports it across the duodenal mucosal
cell in vesicular form. At least part of vit D action is quick (within minutes)
and, therefore, appears to be exerted by mechanisms not involving gene
regulation.
2. Calcitriol enhances
resorption of calcium and phosphate from bone
by promoting recruitment and differentiation of osteoclast precursors in the
bone remodeling units, but mature osteoclasts lack VDR. Like PTH, calcitriol
induces RANKL in osteoblasts which may then activate the osteoclasts.
Osteoblastic cells express VDR and respond to calcitriol by laying down
osteoid, but it mainly appears to help bone mineralization indirectly by
maintaining normal plasma calcium and phosphate concentration. Its action is
independent of but facilitated by PTH.
3. Calcitriol enhances
tubular reabsorption of calcium and phosphate in the kidney, but the action is less marked than that of PTH. However, in
hypervitaminosis D, influence of hypercalcaemia overrides the direct action and
more calcium is excreted in urine.
4.
Other actions Actions of calcitriol on immunological cells, lymphokine
production, proliferation and differentiation of epidermal and certain
malignant cells, neuronal and skeletal muscle function have also been
demonstrated.
Vit D Deficiency
Plasma calcium and phosphate
tend to fall due to inadequate intestinal absorption. As a consequence, PTH is
secreted → calcium is mobilized
from bone in order to restore plasma Ca2+. The bone fails to mineralize
normally in the newly laid area, becomes soft → rickets in children
and osteomalacia in adults. However, in contrast to osteoporosis, the organic matrix (osteoid) is normal in these conditions.
Hypervitaminosis D
It may occur due to
chronic ingestion of large doses (~50,000 IU/day) or due to increased
sensitivity of tissues to vit D. Manifestations are due to elevated plasma
calcium and its ectopic deposition.
Hypercalcaemia,
weakness, fatigue, vomiting, diarrhoea, sluggishness, polyuria, albuminuria,
ectopic Ca2+ deposition (in soft tissues, blood vessels, parenchymal organs),
renal stones or nephrocalcinosis, hypertension, growth retardation in children.
Even coma has been reported. Treatment: consists
of withholding the vitamin, low calcium diet,
plenty of fluids and corticosteroids. Recovery may be incomplete in many cases.
Pharmacokinetics
Vit D is well absorbed
from the intestines in the presence of bile salts, mainly through lymphatics.
Absorption of D3 form is somewhat better than that of D2.
Malabsorption and steatorrhoea interfere with its absorption.
In the circulation, it
is bound to a specific α globulin and is stored in the body, mostly in
adipose tissues, for many months. It is hydroxylated in the liver to active and
inactive metabolites. The t½ of different forms varies from 1–18 days: 25OHD 3,
having the longest t½ , constitutes the primary circulating form. Calcitriol is
cleared rapidly.
Metabolites of vit D
are excreted mainly in bile.
Unitage And Preparations
1 μg of cholecalciferol =
40 IU of vit D.
The daily requirement varies, depending on
exposure to sunlight. It is estimated that if no vit D3 is synthesized in the
body, a dietary allowance of 400 IU/day will prevent deficiency symptoms. The
forms in which vit D is supplied are—
1. Calciferol (Ergocalciferol, vit D2) As solution in oil, filled in gelatin
capsules 25,000 and 50,000 IU caps.
2. Cholecalciferol (vit D3) As granules for oral
ingestion and oily solution for i.m. injection.
ARACHITOL 300,000 IU (7.5 mg) and 600,000 IU
(15 mg) per ml inj.
CALCIROL 60,000 IU in 1 g granules—given at 3–4 weeks intervals, and then
every 2–6 months.
3. Calcitriol 0.25–1 μg orally daily or on
alternate days; CALTROL, ROLSICAL, ROCALTROL 0.25 μg cap. CALCIBEST 1 μg in 1 ml aqueous inj;
0.5–1 μg i.v. on alternate days.
Hypercalcaemia is the main adverse effect;
must be watched for and therapy promptly stopped if plasma Ca2+ rises.
4. Alfacalcidol It is 1 αOHD3—a
prodrug that is rapidly hydroxylated in the liver to 1, 25 (OH)2
D3 or calcitriol. Therefore, it does not require hydroxylation at position 1
which is the limiting step in the generation of the active form of vit D, and
which takes place in the kidney. As such, it is effective in renal bone
disease, vit D dependent rickets, vit D resistant rickets, hypoparathyroidism,
etc.— indications for which calcitriol is needed. It is also being used in
osteoporosis.
Alfacalcidol is orally
active and clinically equally effective on long term basis to calcitriol. Its
metabolic activation in liver does not pose a problem even in severe liver
disease.
Dose: 1–2 μg/day, children <
20 kg 0.5 μg/day. Repeated serum calcium measurements are
essential for regulation of maintenance dose. Hypercalcaemia should be watched
for and therapy promptly interrupted for few days when it develops.
ONE ALPHA, ALPHA D3,
ALPHADOL 0.25 and 1 μg caps, ALFACAL 0.25, 0.5 μg caps.
a) Dihydrotachysterol (DHT) A synthetic analogue
of vit D2—less
active in antirachitic tests, but directly mobilizes calcium from bone: does
not require PTH dependent activation in the kidney—particularly useful in
hypoparathyroidism and renal bone disease.
Dose: 0.25–0.5 mg/day.
Combination
preparations of vit D are listed in Table 67.2.
Use
1. Prophylaxis
(400 IU/day) and treatment (3000–4000 IU/day) of nutritional vit D deficiency which causes rickets
in children and osteomalacia in adults. Alternatively 300,000–600,000 IU can be
given orally or i.m. once in 2–6 months. Prophylactic treatment may be given in
obstructive jaundice, steatorrhoea and other conditions which predispose to vit
D deficiency.
2. Metabolic
rickets These are a group of conditions in which tissues do not respond
to normal doses of vit D.
(a) Vit D resistant rickets: Xlinked hereditary disease in which
vit D metabolism is normal but calcium and phosphate metabolism is deranged.
Administration of phosphate with high dose of calcitriol or alfacalcidol is
beneficial.
(b) Vit D dependent rickets: Another
genetic disorder due to deficiency of renal hydroxylating mechanism which
converts 25OHD3 into calcitriol. Administration of calcitriol or alfacalcidol
is effective in normal doses.
(c) Renal rickets:
Conversion of 25OHD3 into calcitriol does not
occur due to chronic renal disease. Calcitriol/alfacalcidol or dihydrotachysterol
are needed in usual doses.
3. Senile Or Postmenopausal Osteoporosis Agerelated decrease in
calcium absorption from gut has been noted. Vit D3 + calcium have
been shown to improve calcium balance in osteoporotic females and elderly
males. However, benefit in terms of improved bone mass or reduced fracture risk
is controversial or marginal (see p.
327). But this does not apply to active therapy with calcitriol/alfacalcidol
for patients with established osteoporosis, because it suppresses parathyroids
and reduces bone remodeling. Vit D deficiency results in secondary hyperparathyroidism
which contributes to osteoporosis. Though bone mineral density may be improved,
calcitriol therapy carries the risk of hypercalcaemia, calcium stones and
metastatic calcification.
4. Hypoparathyroidism Dihydrotachysterol or calcitriol/alfacalcidol
are more effective than vit D2 or D3 because they act
quickly and directly without the need for hydroxylation in kidney which needs
PTH. Alternatively, conventional preparations of vit D3 may be given
in high doses (25000100,000 IU/day).
5. Fanconi Syndrome Vit D can raise the lowered phosphate levels
that occur in this condition.
6. A nonhypercalcaemic
analogue of vit D Calcipotriol (DAIVONEX 0.005% oint)
is used locally in
plaque type psoriasis, and has yielded good results (see Ch. No. 64). Systemically it has been tried in skin cancer and
immunological disorders.
Interactions
1. Cholestyramine and chronic use of liquid paraffine can reduce
vit D absorption.
2. Phenytoin and phenobarbitone reduce the responsiveness of
target tissues to calcitriol; their prolonged use (for epilepsy) can cause
rickets/ osteomalacia. It was believed earlier that these drugs enhance
degradation of vit D. However, now it has been shown that plasma level of
calcitriol is normal, but its effect on intestine and bone is diminished.
Related Topics
