Uses of Insulin
| Home | | Pharmacology |Chapter: Essential pharmacology : Insulin, Oral Hypoglycaemic Drugs and Glucagon
Diabetes Mellitus : The purpose of therapy in diabetes mellitus is to restore metabolism to normal, avoid symptoms due to hyperglycaemia and glucosuria, prevent shortterm complications (infection, ketoacidosis, etc.) and longterm sequelae (cardiovascular, retinal, neurological, renal, etc.)
USES OF
INSULIN
Diabetes Mellitus
The
purpose of therapy in diabetes mellitus is
to restore metabolism to normal, avoid symptoms due to hyperglycaemia and
glucosuria, prevent shortterm complications (infection, ketoacidosis, etc.) and
longterm sequelae (cardiovascular, retinal, neurological, renal, etc.)
Insulin is effective
in all forms of diabetes mellitus and is a must for type 1 cases, as well as
for post pancreatectomy diabetes and gestational diabetes. Many type 2 cases
can be controlled by diet, reduction in body weight and appropriate exercise.
Insulin is needed by such patients when:
· Not controlled by diet and exercise or when
these are not practicable.
· Primary or secondary failure of oral hypoglycaemics
or when these drugs are not tolerated.
· Under weight patients.
· Temporarily to tide over infections, trauma,
surgery, pregnancy. In the perioperative period and during labour, monitored
i.v. insulin infusion is preferable.
· Any complication of diabetes, e.g. ketoacidosis,
nonketotic hyperosmolar coma, gangrene of extremities.
When
instituted, insulin therapy is generally started with regular insulin given
s.c. before each major meal. The requirement is assessed by testing urine or
blood glucose levels (glucose oxidase based spot tests and glucometers are
available). Most type 1 patients require 0.4–0.8 U/kg/day. In type 2 patients,
insulin dose varies (0.2–1.6 U/ kg/day) with the severity of diabetes and body
weight: obese patients require proportionately higher doses due to relative
insulin resistance. A suitable regimen for each patient is then devised by
including modified insulin preparations.
Any
satisfactory regimen should provide basal control by inhibiting hepatic glucose
output, as well as supply extra amount to meet postprandial needs for disposal
of absorbed glucose and amino acids. Often mixtures of regular and
lente/isophane insulins are used. The total daily dose of a 30:70 mixture of
regular and NPH insulin is usually split into two (splitmixed regimen) and
injected s.c. before breakfast and before dinner. Several variables viz. site and depth of s.c. injection,
posture, regional muscular activity, injected volume, type of insulin can alter
the rate of absorption of s.c. injected insulin and can create mismatch between
the actual requirement (high after meals, low at night) and the attained insulin
levels.
Another preferred
regimen is to give a long-acting insulin (glargine) once daily either before
breakfast or before bedtime for basal coverage along with 2–3 mealtime injections
of a rapid acting preparation (insulin lispro or aspart). Such intensive
regimens have the objective of achieving round the clock euglycaemia. The large
multicentric diabetes control and complications trial (DCCT) among type 1
patients has established that intensive insulin therapy markedly reduces the
occurrence of primary diabetic retinopathy, neuropathy, nephropathy and slows
progression of these complications in those who already have them in comparison
to conventional regimens which attain only intermittent euglycaemia. Thus, the
risk of macrovascular disease appears to be related to the glycaemia control.
The UK prospective diabetes study (UK PDS, 1998) has extended these
observations to type 2 DM patients as well. Since the basis of pathological
changes in both type 1 and type 2 DM is accumulation of glycosylated proteins
and sorbitol in tissues as a result of exposure to high glucose concentrations,
tight glycaemia control can delay endorgan damage in all diabetic subjects.
However, regimens
attempting near normoglycaemia are associated with higher incidence of severe
hypoglycaemic episodes. Moreover, injected insulin fails to reproduce the
normal pattern of increased insulin secretion in response to each meal, and
liver is exposed to the same concentration of insulin as other tissues while
normally liver receives much higher concentration. As such, the overall
desirability and practicability of intensive insulin therapy has to be
determined in individual patients. Intensive insulin therapy is best avoided in
young children (risk of hypoglycaemic brain damage) and in the elderly (more
prone to hypoglycaemia and its serious consequences).
Diabetic Ketoacidosis (Diabetic Coma)
Ketoacidosis of
different grades generally occurs in insulin dependent diabetics. It is
infrequent in type 2 DM. The most common precipitating cause is infection;
others are trauma, stroke, pancreatitis, stressful conditions and inadequate
doses of insulin.
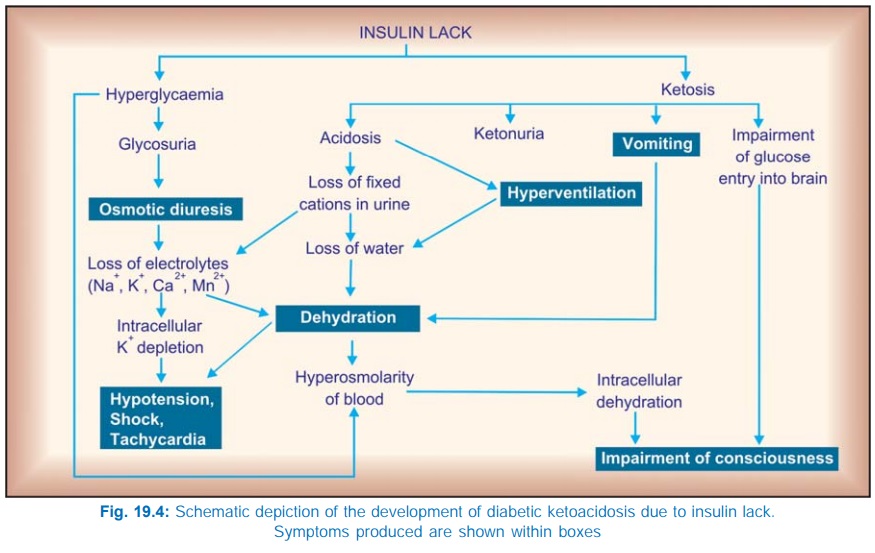
The development of cardinal
features of diabetic ketoacidosis is outlined in Fig. 19.4. Patients may
present with varying severity. Typically they are dehydrated, hyperventilating
and have impaired consciousness. The principles of treatment remain the same,
irrespective of severity, only the vigour with which therapy is instituted is
varied.
1. Insulin Regular insulin is
used to rapidly correct the metabolic
abnormalities. A bolus dose of 0.1–0.2 U/kg i.v. is followed by 0.1 U/kg/hr
infusion; the rate is doubled if no significant fall in blood glucose occurs in
2 hr. Fall in blood glucose level by 10% per hour can be considered adequate
response.
Usually, within 4–6
hours blood glucose reaches 300 mg/dl. Then the rate of infusion is reduced to
2–3 U/hr. This is maintained till the patient becomes fully conscious and routine
therapy with s.c. insulin is instituted.
2. Intravenous fluids It is vital to correct
dehydration. Normal saline is infused i.v., initially at the rate of 1 L/hr, reducing
progressively to 0.5 L/4 hours depending on the volume status. Once BP and heart
rate have stabilized and adequate renal perfusion is assured change over to ½N
saline. After the blood sugar has reached 300 mg/ dl, 5% glucose in ½N saline
is the most appropriate solution because blood glucose falls before ketones are
fully cleared from the circulation. Also glucose is needed to restore the
depleted hepatic glycogen.
3. KCl Though upto 400 mEq of K+ may be lost in urine during
ketoacidosis, serum K+ is usually normal due to exchange with intracellular stores.
When insulin therapy is instituted ketosis subsides and K+ is driven
intracellularly— dangerous hypokalemia can occur. After 4 hours
it
is appropriate to add 10–20 mEq/hr KCl to the i.v. fluid. Further rate of
infusion is guided by serum K+ measurements and ECG.
4. Sodium bicarbonate It is not routinely
needed. Acidosis subsides as
ketosis is controlled. However, if arterial blood pH is < 7.1, acidosis is
not corrected spontaneously or hyperventilation is exhausting, 50 mEq of sod.
bicarbonate is added to the i.v. fluid. Bicarbonate infusion is continued
slowly till blood pH rises above 7.2.
5. Phosphate When serum PO4 is in the lownormal range, 5–10 m mol/hr of
sod./pot. phosphate infusion is advocated. However, routine use of PO4
in all cases is still controversial.
6. Antibiotics and other supportive measures and treatment of precipitating cause must be instituted simultaneously.
Hyperosmolar (Nonketotic Hyperglycaemic) Coma
This usually occurs in
elderly type 2 cases. Its cause is
obscure, but appears to be precipitated by the same factors as ketoacidosis,
especially those resulting in dehydration. Uncontrolled glycosuria of DM
produces diuresis resulting in dehydration and haemoconcentration over several
days → urine output is
finally reduced and glucose accumulates in blood rapidly to > 800 mg/dl,
plasma osmolarity is > 350 mOsm/L → coma, and death can occur if not vigorously
treated.
The general principles
of treatment are the same as for ketoacidotic coma, except that faster fluid
replacement is to be instituted and alkali is usually not required. These
patients are prone to thrombosis (due to hyperviscosity and sluggish
circulation), prophylactic heparin therapy is recommended.
Despite intensive therapy,
mortality in hyperosmolar coma remains high. Treatment of precipitating factor
and associated illness is vital.
