Tricyclic Antidepressants (TCAS)
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs Used In Mental Illness: Antidepressant And Antianxiety Drugs
Imipramine, an analogue of CPZ was found during clinical trials (1958) to selectively benefit depressed but not agitated psychotics. In contrast to CPZ, it inhibited NA and 5HT reuptake into neurones.
TRICYCLIC ANTIDEPRESSANTS (TCAS)
Imipramine, an analogue of CPZ was found during clinical trials (1958) to selectively benefit depressed but not agitated psychotics. In contrast to CPZ, it inhibited NA and 5HT reuptake into neurones. A large number of congeners were soon added and are collectively called tricyclic antidepressants (TCAs).
Pharmacological Actions
The most prominent action of TCAs is their ability to inhibit norepinephrine transporter (NET) and serotonin transporter (SERT) located at neuronal/platelet membrane at low and therapeutically attained concentrations.
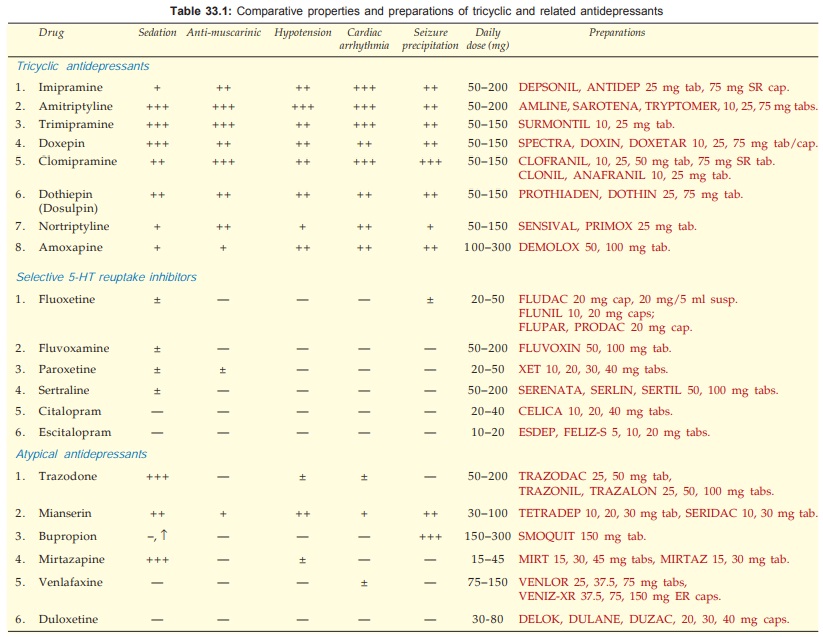
The TCAs inhibit monoamine reuptake and interact with a variety of receptors viz. muscarinic, α adrenergic, histamine H1, 5HT1, 5 HT2 and occasionally dopamine D2. However, relative potencies at these sites differ among different compounds. The newer selective serotonin reuptake inhibitors (SSRIs) and atypical antidepressants interact with fewer receptors and have more limited spectrum of action (produce fewer side effects). The actions of imipramine are described as prototype.
1. CNS
Effects differ in normal individuals and the depressed.
In normal individuals It induces a peculiar clumsy feeling, tiredness, light-headedness, sleepiness, difficulty in concentrating and thinking, unsteady gait. These effects tend to provoke anxiety. There is no mood elevation or euphoria; effects are rather unpleasant and may become more so on repeated administration.
In depressed patients Little acute effects are produced, except sedation (in the case of drugs which have sedative property). After 2–3 weeks of continuous treatment, the mood is gradually elevated, patients become more communicative and start taking interest in self and surroundings. Thus, TCAs are not euphorients but only antidepressants. In depressed patients who have preponderance of REM sleep, this phase is suppressed and awakenings during night are reduced. The EEG effects of low doses are similar to hypnotics but high doses cause desynchronization. Sedative property varies among different compounds: (see Table 33.1). The more sedative ones are suitable for depressed patients showing anxiety and agitation. The less sedative or stimulant ones are better for withdrawn and retarded patients.
The TCAs lower seizure threshold and produce convulsions in overdose. Clomipramine, maprotiline and bupropion have the highest seizure precipitating potential. Amitriptyline and imipramine depress respiration in overdose only.
Mechanism Of Action
The TCAs and related drugs inhibit active reuptake of biogenic amines NA and 5HT into their respective neurones and thus potentiate them. They, however, differ markedly in their selectivity and potency for different amines (see classification above).
Most of the compounds do not inhibit DA uptake, except bupropion. Moreover, amphetamine and cocaine (which are not antidepressants but CNS stimulants) are strong inhibitors of DA uptake. However, it has been proposed that TCAs indirectly facilitate dopaminergic transmission in forebrain that may add to the mood elevating action.
Reuptake inhibition results in increased concentration of the amines in the synaptic cleft in the CNS and periphery. Tentative conclusions drawn are:
• Inhibition of DA uptake correlates with stimulant action; but is not primarily involved in antidepressant action.
• Inhibition of NA and 5HT uptake is associated with antidepressant action.
Several findings indicate that uptake blockade is not directly responsible for antidepressant action, e.g. uptake blockade occurs quickly but antidepressant action develops after weeks; mianserin is antidepressant but has no uptake blocking action. Initially the presynaptic α2 and 5HT1 autoreceptors are activated by the increased amount of NA/5HT in the synaptic cleft resulting in decreased firing of locus coeruleus (noradrenergic) and raphe (serotonergic) neurones. However, on long-term administration, antidepressants desensitise presynaptic α2, 5HT1A, 5HT1D autoreceptors and induce other adaptive changes in the number and sensitivity of pre and post synaptic NA and/or 5HT receptors as well as in amine turnover of brain, the net effect of which is enhanced noradrenergic and serotonergic transmission. Thus, uptake blockade appears to initiate a series of time-dependent changes that culminate in antidepressant effect.
Trimipramine is a weak NA/5HT reuptake blocker, but an equally effective antidepressant. None of these compounds, except amoxapine and to some extent maprotiline, block DA receptors or possess antipsychotic activity.
2. ANS
Most TCAs are potent anticholinergics—cause dry mouth, blurring of vision, constipation and urinary hesitancy as side effect. The anticholinergic potency is graded in Table 33.1
They potentiate exogenous and endogenous NA by blocking uptake, but also have weak α1 adrenergic blocking action. Some, e.g. amitriptyline, doxepin, trimipramine have slight H1 antihistaminic action as well.
3. CVS Effects on cardiovascular function are prominent, occur at therapeutic concentrations and may be dangerous in overdose.
Tachycardia: due to anticholinergic and NA potentiating actions.
Postural Hypotension: due to inhibition of cardiovascular reflexes and α1 blockade.
ECG Changes And Cardiac Arrhythmias: T wave suppression or inversion is the most consistent change. Arrhythmias occur in overdose due to interference with intraventricular conduction, combination of NA potentiating + ACh blocking actions and direct myocardial depression. Older patients are more susceptible. The SSRIs and atypical antidepressants are safer in this regard.
Tolerance And Dependence
Tolerance to the anticholinergic and hypotensive effects of imipramine like drugs develops gradually, though antidepressant action is sustained.
Psychological dependence on these drugs is rare, because their acute effects are not pleasant.
There is some evidence of physical dependence occurring when high doses are used for long periods—malaise, chills, muscle pain may occur on discontinuation and have been considered withdrawal phenomena. Gradual withdrawal is recommended, but antidepressants do not carry abuse potential.
Pharmacokinetics
The oral absorption of TCAs is good, though often slow. They are highly bound to plasma and tissue proteins—have large volumes of distribution (~20 L/kg). They are extensively metabolized in liver; the major route for imipramine and amitriptyline is demethylation whereby active metabolites—desipramine and nortriptyline respectively are formed. Few others also produce active metabolites. Inactivation occurs by oxidation and glucuronide conjugation. Various CYP isoenzymes like CYP2D6, CYP 3A4, CYP 1A2 and others metabolise tricylic and related anti-depressants. Metabolites are excreted in urine over 1–2 weeks. The plasma t½ of amitriptyline, imipramine and doxepin range between 16–24 hours. The t½ is longer for some of their active metabolites. Because of relatively long t½s, once daily dosing (at bed time) is practicable in the maintenance phase.
An unusual therapeutic window phenomenon has been observed, i.e. optimal antidepressant effect is exerted at a narrow band of plasma concentrations (between 50–200 ng/ml of imipramine, amitriptyline, nortriptyline). Both below and above this range, beneficial effects are suboptimal.
Wide variation in the plasma concentration attained by different individuals given the same dose has been noted. Thus, doses need to be individualized and titrated, but plasma concentrations are not a reliable guide for adjusting the dose of TCAs.
Adverse Effects
Side effects are common with tricyclic antidepressants.
• Anticholinergic: dry mouth, bad taste, constipation, epigastric distress, urinary retention (especially in males with enlarged prostate), blurred vision, palpitation.
• Sedation, mental confusion and weakness, especially with amitriptyline and more sedative congeners.
• Increased appetite and weight gain is noted with most TCAs and trazodone, but not with SSRIs and bupropion.
• Some patients receiving any antidepressant may abruptly switch over to a dysphoricagitated state or to mania. Most likely, these are cases of bipolar depression, the other pole being unmasked by the antidepressant. Patients receiving higher doses and TCAs are at greater risk than those receiving lower doses and SSRIs or bupropion.
• Sweating and fine tremors are relatively common.
• Seizure threshold is lowered—fits may be precipitated, especially in children. Bupropion, maprotiline, clomipramine, amoxapine have greater propensity, while desipramine and SSRIs are safer in this regard.
• Postural hypotension, especially in older patients; less severe with desipramine-like drugs and insignificant with SSRIs.
• Cardiac arrhythmias, especially in patients with ischaemic heart disease—may be responsible for sudden death in these patients. Amitriptyline and dosulpin are particularly dangerous in overdose; higher incidence of arrhythmias is reported.
• Rashes and jaundice due to hypersensitivity are rare. Mianserin is more hepatotoxic.
Acute Poisoning
It is frequent; usually self-attempted by the depressed patients, and may endanger life. Manifestations are:
Excitement, delirium and other anticholinergic symptoms as seen in atropine poisoning, followed by muscle spasms, convulsions and coma. Respiration is depressed, body temperature may fall, BP is low, tachycardia is prominent. ECG changes and ventricular arrhythmias are common.
Treatment is primarily supportive with gastric lavage, respiratory support, fluid infusion, maintenance of BP and body temperature. Acidosis must be corrected by bicarbonate infusion.
Diazepam may be injected i.v. to control convulsions and delirium. Most important is the treatment of cardiac arrhythmias, for which propranolol/lidocaine may be used; class IA and IC antiarrhythmics and digoxin prolong cardiac conduction—are contraindicated.
Physostigmine (0.5–2 mg i.v.) reverses many central and peripheral anticholinergic and sometimes cardiac effects. However, it is seldom used since arrhythmias are occasionally worsened and hypotension accentuated by this treatment.
Interactions
· TCAs potentiate directly acting sympathomimetic amines (in cold/asthma remedies). Adrenaline containing local anaesthetic should be avoided. However TCAs attenuate the actions of indirect sympathomimetics (ephedrine, tyramine).
· TCAs abolish the antihypertensive action of guanethidine and clonidine by preventing their transport into adrenergic neurones.
· TCAs potentiate CNS depressants, including alcohol and antihistaminics.
· Phenytoin, phenylbutazone, aspirin and CPZ can displace TCAs from protein binding sites and cause toxicity.
· Phenobarbitone induces as well as competitively inhibits imipramine metabolism.
· Carbamazepine and other enzyme inducers enhance metabolism of TCAs.
· SSRIs inhibit metabolism of several drugs (see later) including TCAs—dangerous toxicity can occur if the two are given concurrently.
· By their anticholinergic property, TCAs delay gastric emptying and retard their own as well as other drug’s absorption. However, digoxin and tetracyclines may be more completely absorbed. When used together, the anticholinergic action of neuroleptics and TCAs may add up.
· MAO inhibitors—dangerous hypertensive crisis with excitement and hallucinations has occurred when given with TCAs.
Amoxapine
This tetracyclic compound is unusual in that it blocks dopamine D2 receptors in addition to inhibiting NA reuptake. It is chemically related to the antipsychotic drug loxapine and has mixed antidepressant + neuroleptic properties—offers advantage for patients with psychotic depression. Risk of extrapyramidal side effects is also there. Seizures (including status epilepticus) occur in its overdose.
Reboxetine
This is a newer selective NA reuptake blocker with weak effect on 5HT reuptake. Antimuscarinic and sedative actions are minimal. It appears to produce fewer side effects and may be safer in overdose than the older TCAs. Usual side effects are insomnia, dry mouth, constipation, sexual distress and urinary symptoms.
Dose: 4 mg BD or 8 mg OD.
NAREBOX 4, 8 mg tab.
Related Topics
