Thiazide and Related Diuretics
| Home | | Pharmacology |Chapter: Essential pharmacology : Diuretics
Chlorothiazide was synthesized as a CAse inhibitor variant which produced urine that was rich in Cl¯, and diuresis occurred in alkalosis as well as acidosis.
THIAZIDE AND RELATED DIURETICS
(Inhibitors of Na+Cl¯ symport)
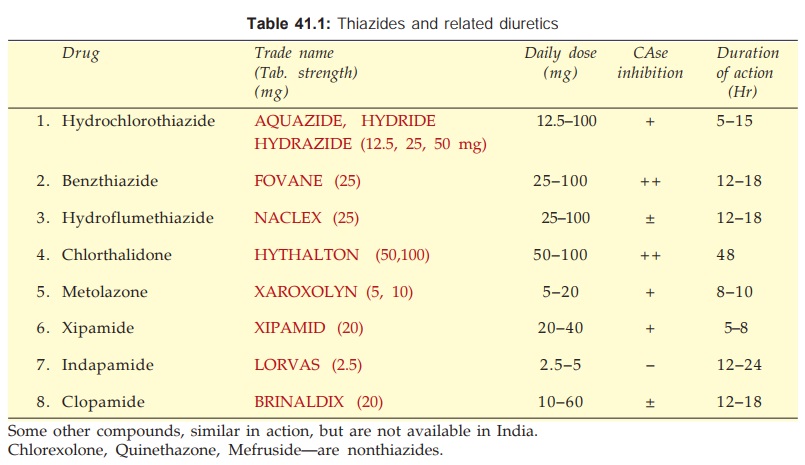
Chlorothiazide was synthesized as a CAse inhibitor variant which produced urine that was rich in Cl¯, and diuresis occurred in alkalosis as well as acidosis. A large number of congeners were developed subsequently and the thiadiazine ring was replaced by other heterocyclic rings, but the type of activity remained the same. The important features of agents marketed in India are presented in Table 41.1.
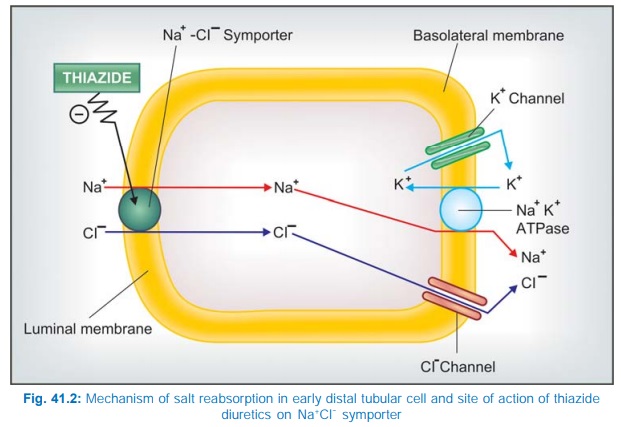
These are medium efficacy diuretics with primary site of action in the cortical diluting segment or the early DT (Site III). Here they inhibit Na+–Cl¯ symport at the luminal membrane. They do not affect the corticomedullary osmotic gradient indicating lack of action at the medullary thick AscLH. Positive free water clearance is reduced (very dilute urine cannot be passed in the absence of ADH), but negative free water clearance (in the presence of ADH) is not affected. This strengthens the view that the site of action is in between thick AscLH and late DT. These drugs gain access to their site of action via organic acid secretory pathway in PT and then along the tubular fluid to early DT, where they bind to specific receptors located on the luminal membrane. Like the Na+ K+2Cl¯ cotransporter, the Na+Cl¯ symporter is also a glycoprotein with 12 membrane spanning domains that binds thiazides but not furosemide or any other class of diuretics. It has been cloned and shown to be selectively expressed on the luminal membrane in the DT. The site of action of thiazide diuretics is shown in Fig. 41.2.
Some of the thiazides and related drugs have additional CAse inhibitory action in PT; intensity of this action differs among different compounds (Table 41.1), but it is generally weak and clinically insignificant. However, it may confer some proximal tubular action to the compounds.
Under their action, increased amount of Na+ is presented to the distal nephron, more of it exchanges with K+ → urinary K+ excretion is increased in parallel to the natriuretic response. The maximal diuresis induced by different agents falls in a narrow range; though potency (reflected in daily dose) differs markedly. Nevertheless, they are moderately efficacious diuretics because nearly 90% of the glomerular filtrate has already been reabsorbed before it reaches their site of action. They have a flat dose response curve; little additional diuresis occurs when the dose is increased beyond 100 mg of hydrochlorothiazide or equivalent. They do not cause significant alteration in acid-base balance of the body.
By their action to reduce blood volume, as also intrarenal haemodynamic changes, they tend to reduce g.f.r. This is one reason why thiazides are not effective in patients with low g.f.r. They decrease renal Ca2+ excretion and increase Mg2+ excretion by a direct distal tubular action. They also decrease urate excretion by the same mechanism as furosemide.
The extrarenal actions of thiazides consist of a slowly developing fall in BP in hypertensives and elevation of blood sugar in some patients due to decreased insulin release which probably is a consequence of hypokalaemia.
Pharmacokinetics
All thiazides and related drugs are well absorbed orally; are administered only by this route. Their action starts within 1 hour, but the duration varies from 8–48 hours (Table 41.1). The more lipidsoluble agents have larger volumes of distribution (some are also tissue bound), lower rates of renal clearance and are longer acting. The protein binding is also variable. Most of the agents undergo little hepatic metabolism and are excreted as suCh. No. They are filtered at the glomerulus as well as secreted in the PT by organic anion transport. Tubular reabsorption depends on lipid solubility: the more soluble ones are highly reabsorbed—prolonging duration of action.
Chlorthalidone It is a particularly long acting agent with a t½ 40–50 hours, used exclusively as antihypertensive.
Metolazone In common with loop diuretics, it is able to evoke a clinically useful response even in severe renal failure (g.f.r. ~15 ml/min), and has marked additive action when combined with furosemide. An additional proximal tubular action has been demonstrated; PO4 reabsorption that occurs in PT is inhibited. It is excreted unchanged in urine.
Xipamide It has a pronounced diuretic action similar to low doses of furosemide. Because of longer duration of action—hypokalemia is more prominent.
Indapamide It has little diuretic action in the usual doses, probably because it is highly lipidsoluble, is extensively metabolized and only small quantity of unchanged drug is present in the tubular fluid. However, it retains antihypertensive action and is used for that purpose only.
Uses
Edema: Thiazides may be used for mild-to-moderate cases. For mobilization of edema fluid more efficacious diuretics are preferred, but thiazides may be considered for maintenance therapy. They act best in cardiac edema, less effective in hepatic or renal edema. They are powerless in the presence of renal failure. Cirrhotics often develop refractoriness to thiazides due to development of secondary hyperaldosteronism.
Hypertension: Thiazides and related diuretics, especially chlorthalidone are one of the first line drugs (Ch. No. 40).
Diabetes Insipidus: They reduce urine volume (see Ch. No. 42).
Hypercalciuria with recurrent calcium stones in the kidney. Thiazides act by reducing Ca2+ excretion.
Complications Of High Ceiling And Thiazide Type Diuretic Therapy
Most of the adverse effects of these drugs are related to fluid and electrolyte changes caused by them. They are remarkably safe in low doses used over short periods. Many subtle metabolic effects have been reported in their long-term use as antihypertensives at the relatively higher doses used in the past (see Ch. No. 40).
1. Hypokalaemia: This is the most significant problem. It is rare at low doses, but may be of grave consequence when brisk diuresis is induced or on prolonged therapy, especially if dietary K+ intake is low. Degree of hypokalaemia appears to be related to the duration of action of the diuretic; longer acting drugs causing more K+ loss. The usual manifestations are weakness, fatigue, muscle cramps; cardiac arrhythmias are the serious complications. Hypokalaemia is less common with standard doses of high ceiling diuretics than with thiazides, possibly because of shorter duration of action of the former which permits intermittent operation of compensatory repletion mechanisms. It can be prevented and treated by:
(a) High dietary K+ intake or
(b) Supplements of KCl (24–72 mEq/day) or
(c) Concurrent use of K+ sparing diuretics.
Measures (b) and (c) are not routinely indicated, but only when hypokalaemia has been documented or in special risk situations, e.g. cirrhotics, cardiac patients—especially post MI, those receiving digitalis, antiarrhythmics, or tricyclic antidepressants and elderly patients.
Serum K+ levels are only a rough guide to K+ depletion, because K+ is primarily an intracellular ion. Nevertheless, an attempt to maintain serum K+ at or above 3.5 mEq/L should be made.
Combined tablets of diuretics and KCl are not recommended because:
· they generally contain insufficient quantity of K+ (8–12 mEq only).
· may cause gut ulceration by releasing KCl at one spot.
· K+ is retained better if given after the diuresis is over.
K+ sparing diuretics are more efficacious and more convenient in correcting hypokalaemia than are K+ supplements. ACE inhibitors/AT1 antagonists given with thiazides tend to prevent development of hypokalaemia.
Alkalosis may occur with hypokalaemia, because more H+ exchanges with Na+ in DT when less K+ is available for exchange.
2. Acute Saline Depletion: Over enthusiastic use of diuretics, particularly high ceiling ones, may cause dehydration and fall in BP (especially in erect posture). Serum Na+ and Cl¯ levels remain normal because isotonic saline is lost. It should be treated by saline infusion.
3. Dilutional Hyponatraemia: Occurs in CHF patients when vigorous diuresis is induced with high ceiling agents, rarely with thiazides. Kidney tends to retain water, though it is unable to retain salt due to the diuretic; e.c.f. gets diluted, hyponatraemia occurs and edema persists despite natriuresis. Patients feel very thirsty. Treatment of this distortion of fluidelectrolyte balance is difficult: withhold diuretics, restrict water intake and give glucocorticoid which enhances excretion of water load. If hypokalaemia is present, its correction helps.
4. GIT and CNS Disturbances: Nausea, vomiting and diarrhoea may occur with any diuretic. Headache, giddiness, weakness, paresthesias, impotence are occasional complaints with thiazides as well as loop diuretics.
5. Hearing Loss: Occurs rarely, only with high ceiling diuretics and when these drugs are used in the presence of renal insufficiency. Increased
salt content of endolymph and a direct toxic action on the hair cells in internal ear appear to be causative.
6. Allergic Manifestations: Rashes, photosensitivity occur, especially in patients hypersensitive to sulfonamides. Blood dyscrasias are rare; any diuretic may be causative.
7. Hyperuricaemia: Long-term use of higher dose thiazides in hypertension has caused rise in blood urate level. This is uncommon now due to use of lower doses (see Ch. No. 40). Furosemide produces a lower incidence of hyperuricaemia. This effect can be counteracted by allopurinol. Probenecid is better avoided, because it may interfere with the diuretic response, particularly of loop diuretics.
8. Hyperglycaemia and Hyperlipidemia: Have occurred in the use of diuretics as antihypertensive (see Ch. No. 40). These metabolic changes are minimal at low doses now recommended.
9. Hypercalcaemia: Occurs with thiazides, while hypocalcaemia occurs with high ceiling diuretics when these are administered chronically.
10. Magnesium Depletion: It may develop after prolonged use of thiazides as well as loop diuretics, and may increase the risk of ventricular arrhythmias, especially after MI or when patients are digitalized. K+ sparing diuretics given concurrently minimise Mg2+ loss.
11. Thiazides have sometimes aggravated renal insufficiency, probably by reducing g.f.r.
12. Brisk diuresis induced in cirrhotics may precipitate mental disturbances and hepatic coma. It may be due to hypokalaemia, alkalosis and increased blood NH3 levels.
13. Diuretics should not be used in toxaemia of pregnancy in which blood volume is low despite edema. Diuretics may further compromise placental circulation → miscarriage, foetal death. Thus, diuretics are contraindicated in pregnancy induced hypertension.
Interactions
1. Thiazides and high ceiling diuretics potentiate all other antihypertensives. This interaction is intentionally employed in therapeutics.
2. Hypokalaemia induced by these diuretics:
· Enhances digitalis toxicity.
· Increases the incidence of polymorphic ventricular tachycardia due to quinidine and other antiarrhythmics.
· Potentiates competitive neuromuscular blockers and reduces sulfonylurea action.
3. High ceiling diuretics and aminoglycoside antibiotics are both ototoxic and nephrotoxic; produce additive toxicity; should be used together cautiously.
4. Cotrimoxazole given with diuretics has caused higher incidence of thrombocytopenia.
5. Indomethacin and other NSAIDs diminish the action of high ceiling diuretics. Inhibition of PG synthesis in the kidney, through which furosemide and related drugs induce intrarenal haemodynamic changes which secondarily affect salt output, appears to be the mechanism. Antihypertensive action of thiazides and furosemide is also diminished by NSAIDs.
6. Probenecid competitively inhibits tubular secretion of furosemide and thiazides: decreases their action by reducing the concentration in the tubular fluid, while diuretics diminish uricosuric action of probenecid.
7. Serum lithium level rises when diuretic therapy is instituted. This is due to enhanced reabsorption of Li+ (and Na+) in PT.
Resistance To High Ceiling Diuretics
Refractoriness (progressive edema despite escalating diuretic therapy) is more common with thiazides, but occurs under certain circumstances with high ceiling diuretics as well. The causes and mechanism of such resistance include:
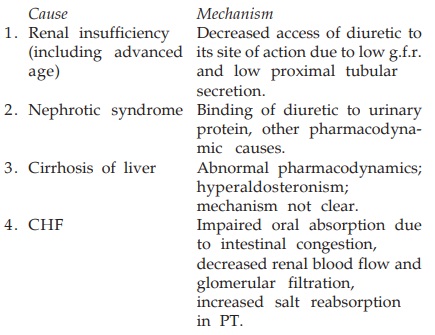
Long-term use of loop diuretics causes distal nephron hypertrophy → resistance. Addition of metolazone, or to some extent a thiazide, which act on distal tubule overcome the refractoriness in many cases. Further increase in dose and/or fractionation of daily dose may restart diuresis. Bedrest may also help.
Related Topics
