Tetracyclines
| Home | | Pharmacology |Chapter: Essential pharmacology : Tetracyclines And Chloramphenicol (Broadspectrum Antibiotics)
All are obtained from soil actinomycetes. The first to be introduced was chlortetracycline in 1948 under the name aureomycin (because of the golden yellow colour of S. aureofaciens colonies producing it).
TETRACYCLINES
These are a class of antibiotics having a nucleus of four cyclic
rings.
All are obtained from
soil actinomycetes. The first to be introduced was chlortetracycline in 1948
under the name aureomycin (because of
the golden yellow colour of S.
aureofaciens colonies producing it). It contrasted markedly from penicillin and streptomycin (the
other two antibiotics available at that time) in being active orally and in
affecting a wide range of microorganisms—hence called ‘broadspectrum
antibiotic’. Oxytetracycline soon followed; others were produced later, either
from mutant strains or semisynthetically.
All tetracyclines are slightly bitter solids which are weakly
water soluble, but their hydrochlorides are more soluble. Aqueous solutions are
unstable. All have practically the same antimicrobial activity (with minor
differences). The subsequently developed members have high lipid solubility,
greater potency and some other differences. The tetracyclines still available
in India for clinical use are:
Tetracycline
Demeclocycline
Oxytetracycline
Doxycycline
Minocycline
Many others like
Chlortetracycline, Methacycline, Rolitetracycline, Lymecycline are no longer
commercially available.
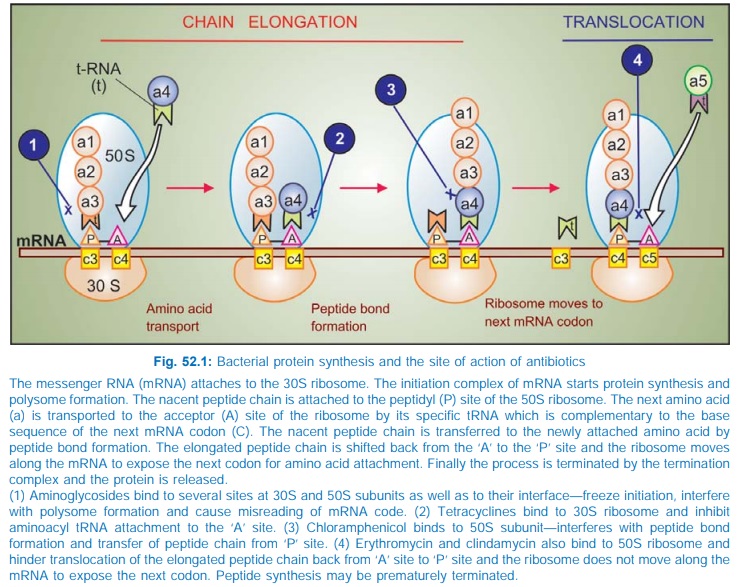
Mechanism Of Action
The tetracyclines are primarily bacteriostatic; inhibit protein
synthesis by binding to 30S ribosomes in susceptible organism. Subsequent to
such binding, attachment of aminoacylt-RNA to the m-RNA-ribosome complex is
interferred with (Fig. 52.1). As a result, the peptide chain fails to grow.
The sensitive organisms
have an energy dependent active transport process which concentrates
tetracyclines intracellularly. In gram-negative bacteria tetracyclines diffuse
through porin channels as well. The more lipid-soluble members (doxycycline,
minocycline) enter by passive diffusion also (this is partly responsible for
their higher potency). The carrier involved in active transport of
tetracyclines is absent in the host cells. Moreover, protein synthesizing
apparatus of host cells is less sensitive to tetracyclines. These two factors
are responsible for the selective toxicity of tetracyclines for the microbes.
Antimicrobial Spectrum
When originally introduced,
tetracyclines inhibited practically all types of pathogenic microorganisms
except fungi and viruses; hence the name ‘broad-spectrum antibiotic’. However,
promiscous and often indiscriminate use has gradually narrowed the field of
their usefulness.
1. Cocci: All gram-positive and gram-negative cocci were originally sensitive, but now many Strep. pyogenes, Staph. aureus and enterococci have become resistant. Responsiveness of Strep. pneumoniae has decreased somewhat. Tetracyclines (especially minocycline) are now active against few N. gonorrhoeae and N. meningitidis.
2. Most gram-positive
bacilli, e.g. Clostridia and other
anaerobes, Listeria, Corynebacteria, Propionibacterium acnes, B. anthracis are
inhibited but not Mycobacteria, except some atypical ones.
3. Sensitive gram-negative
bacilli are—H. ducreyi, Calymmatobacterium granulomatis, V. cholerae, Yersinia pestis,
Y. enterocolitica, Campylobacter, Helicobacter pylori, Brucella, Pasteurella
multocida, F. tularensis and many anaerobes; some H. influenzae have become insensitive.
Enterobacteriaceae are
now largely resistant. Notable bacilli that are not inhibited are Pseudomonas aeruginosa, Proteus, Klebsiella,
Salmonella typhi and many Bact.
fragilis. MIC against anaerobes
is relatively higher.
4. Spirochetes,
including T. pallidum and Borrelia are quite sensitive.
5. All rickettsiae (typhus, etc.) and chlamydiae are highly
sensitive.
6. Mycoplasma and Actinomyces are moderately sensitive.
7.
Entamoeba histolytica and
Plasmodia are inhibited at high concentrations.
Resistance
Resistance to
tetracyclines develops slowly in a graded
manner. In such bacteria, usually the tetracycline concentrating mechanism
becomes less efficient or the bacteria acquire capacity to pump it out. Another
mechanism is plasmid mediated synthesis of a ‘protection’ protein which
protects the ribosomal binding site from tetracycline. Elaboration of tetracycline
inactivating enzymes is an unimportant mechanism of tetracycline resistance.
Due to widespread use, tetracycline resistance has become common among gram-positive
cocci, E. coli, Enterobacter and many
others.
Nearly complete cross resistance is seen among different members
of the tetracycline group. However, some organisms not responding to other
tetracyclines may be inhibited by therapeutically attained concentrations of
minocycline (the most potent agent).
Partial cross resistance between tetracyclines and
chloramphenicol has been noted.
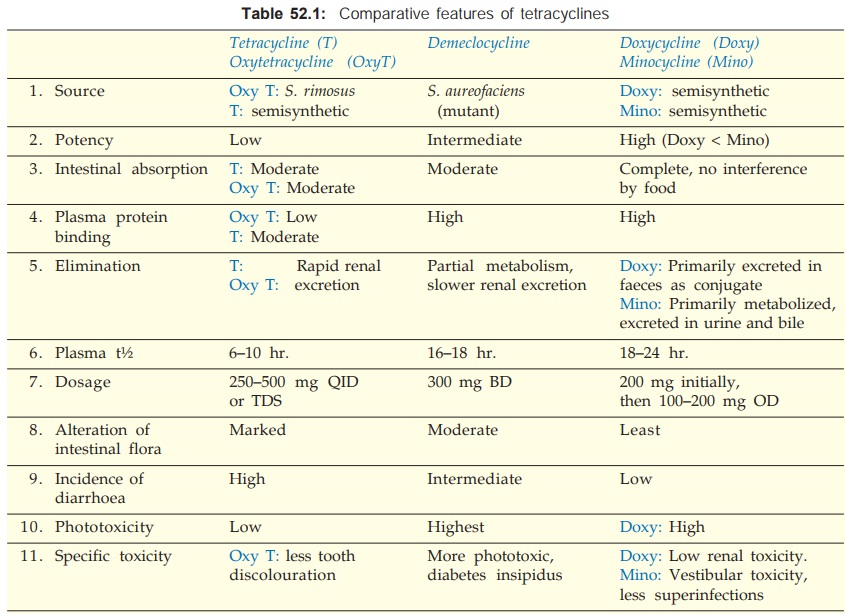
Pharmacokinetics
The pharmacokinetic differences between individual tetracyclines
are included in Table 52.1. The older tetracyclines are incompletely absorbed
from g.i.t.; absorption is better if taken in empty stomach. Doxycycline and
minocycline are completely absorbed irrespective of food. Tetracyclines have
chelating property—form insoluble and unabsorbable complexes with calcium and
other metals. Milk, iron preparations, non-systemic antacids and sucralfate reduce
their absorption. Administration of these substances and tetracyclines should
be staggered, if they cannot be avoided altogether.
Tetracyclines are
widely distributed in the body (volume of distribution > 1 L/kg). Variable
degree of protein binding is exhibited by different members. They are
concentrated in liver, spleen and bind to the connective tissue in bone and teeth.
Intracellularly, they bind to mitochondria. Minocycline accumulates in body
fat. The CSF concentration of most tetracyclines is about 1/4 of plasma
concentration, whether meninges are inflamed or not.
Most tetracyclines are
primarily excreted in urine by glomerular filtration; dose has to be reduced in
renal failure; doxycycline is an exception to this. They are partly metabolized
and significant amounts enter bile—some degree of enterohepatic circulation
occurs. They are secreted in milk in amounts sufficient to affect the suckling
infant.
Enzyme inducers like phenobarbitone
and phenytoin enhance metabolism and reduce the t½ of doxycycline.
Administration
Oral capsule is the
dosage form in which tetracyclines
are most commonly administered. The capsule should be taken ½ hr before or 2 hr
after food. Dry syrups and other liquid oral preparations have been banned and
discontinued to discourage use in children.
Tetracyclines are not
recommended by i.m. route because it is painful and absorption from the
injection site is poor. Slow i.v. injection may be given in severe cases, but
is rarely required now.
A variety of topical
preparations (ointment, cream, etc.) are available, but should not be used,
because there is high risk of sensitization. However, ocular application is not
contraindicated.
Preparations
1. Oxytetracycline: TERRAMYCIN 250, 500 mg
cap, 50 mg/ml in 10 ml vials inj; 3% skin oint, 1% eye/ear oint.
2. Tetracycline: ACHROMYCIN,
HOSTACYCLINE, RESTECLIN 250, 500 mg cap. 3% skin oint, 1% eye/ ear drops and
oint.
3. Demeclocycline
(Demethylchlortetracycline): LEDERMYCIN 150, 300 mg cap/tab.
4. Doxycycline:
TETRADOX,
BIODOXI, DOXT, NOVADOX 100 mg cap.
5. Minocycline: CYANOMYCIN 50, 100 mg
caps.
Adverse Effects
Irritative Effects Tetracyclines can
cause epigastric pain, nausea, vomiting and diarrhoea by their irritant
property. The irritative diarrhoea is to be distinguished from that due to
superinfection. Esophageal ulceration has occurred by release of the material
from capsules in the esophagus during swallowing, especially with doxycycline.
Intramuscular injection of tetracyclines is very painful; thrombophlebitis of
the injected vein can occur, especially on repeated use.
Dose Related Toxicity
1. Liver Damage Fatty infiltration of
liver and jaundice occurs
occasionally. Oxytetracycline and tetracycline are safer in this regard.
Tetracyclines are risky in pregnant women; can precipitate acute hepatic necrosis
which may be fatal.
2.
Kidney Damage It is prominent only
in the presence of existing
kidney disease. All tetracyclines, except doxycycline, accumulate and enhance
renal failure. A reversible Fancony syndrome like condition is produced by
outdated tetracyclines due to
proximal tubular damage caused by degraded products—epitetracycline,
anhydrotetracycline and epi-anhydrotetracycline. Exposure to acidic pH,
moisture and heat favours such degradation.
3. Phototoxicity A sunburnlike or other
severe skin reaction on
exposed parts is seen in some individuals. A higher incidence has been noted
with demeclocycline and doxycycline. Distortion of nails occurs occasionally.
4. Teeth and bones Tetracyclines have chelating property. Calcium-tetracycline chelate gets deposited in developing teeth and bone. Given from mid-pregnancy to 5 months of extrauterine life, the deciduous teeth are affected: brown discolouration, illformed teeth, more susceptible to caries. Tetracyclines given between 3 months and 6 years of age affect the crown of permanent anterior dentition. Repeated courses are more damaging.
Given during late
pregnancy or childhood, tetracyclines can cause temporary suppression of bone
growth. The ultimate effect on stature is mostly insignificant, but deformities
and reduction in height are a possibility with prolonged use.
5. Antianabolic Effect Tetracyclines reduce protein synthesis and have an overall
catabolic effect. They induce negative nitrogen balance and can increase blood
urea.
6. Increased Intracranial Pressure is noted in some infants.
7. Diabetes Insipidus Demeclocycline antagonizes
ADH action and reduces urine concentrating ability of the kidney. It has been
tried in patients with inappropriate ADH secretion.
8. Vestibular Toxicity Minocycline has produced
ataxia, vertigo and nystagmus, which subside when the drug is discontinued.
Hypersensitivity This is infrequent
with tetracyclines. Skin rashes, urticaria, glossitis, pruritus ani and vulvae,
even exfoliative dermatitis have been reported. Angioedema and anaphylaxis are
extremely rare. Complete cross sensitization is exhibited by different
tetracyclines.
Superinfection Tetracyclines are the
most common antibiotics responsible for superinfections, because they cause
marked suppression of the resident flora.
Though mouth, skin or
vagina may be involved, intestinal superinfection by Candida albicans is most prominent (details see p. 672); pseudomembranous enterocolitis is rare but serious.
Higher doses suppress flora more completely— greater chance of superinfection:
doses on the lower side of the range should be used whenever possible. The
tetracycline should be discontinued at the first sign of superinfection and
appropriate therapy instituted.
Doxycycline and
minocycline are less liable to cause diarrhoea, because only small amounts
reach the lower bowel in the active form.
Precautions
1.
Tetracyclines should not be used during
pregnancy, lactation and in children.
2.
They should be avoided in patients on diuretics:
blood urea may rise in such patients.
3.
They should be used cautiously in renal or
hepatic insufficiency.
4.
Preparations should never be used beyond their
expiry date.
5.
Do not mix injectable tetracyclines with
penicillin—inactivation occurs.
6.
Do not inject tetracyclines intrathecally.
Uses
Although tetracyclines
are broad-spectrum antibiotics, they should be employed only for those infections
for which a more selective and less toxic AMA is not available. Clinical use of
tetracyclines has very much declined due to availability of fluoroquinolones and
other efficacious AMAs.
1. Empirical
Therapy Tetracyclines are often employed when the nature
and sensitivity of the infecting organism cannot be reasonably guessed, but
they are not dependable for empirical treatment of serious/life-threatening
infections. They may also be used for initial treatment of mixed infections, although a combination of βlactam and an
aminoglycoside antibiotic or a third generation cephalosporin or a
fluoroquinolone are now preferred.
2. Tetracyclines
Are The First Choice Drugs: despite development of resistance by many
organisms in:
·
Venereal Diseases:
· Chlamydial nonspecific
urethritis/endocervicitis: 7 day doxycycline treatment is as effective as
azithromycin single dose.
·
Lymphogranuloma
venereum: resolves in 2–3 weeks.
· Granuloma inguinale: due to Calymm. granulomatis: a tetracycline administered for 3 weeks is the most effective treatment.
·
Atypical Pneumonia: due to Mycoplasma pneumoniae:
duration of illness is reduced by tetracycline therapy. Psittacosis is treated in 2 weeks by
tetracyclines.
·
Cholera: Tetracyclines have adjuvant
value by reducing stool volume
and limiting the duration of diarrhoea.
· Brucellosis: Tetracyclines are
highly efficacious; cause rapid
symptomatic relief; therapy of choice is doxycycline 200 mg/day + rifampin 600
mg/ day for 6 weeks. Gentamicin may be combined with doxycycline in acute
cases.
· Plague: Tetracyclines are
highly effective in both bubonic and
pneumonic plague. They are preferred for blind/mass treatment of suspected cases
during an epidemic, though streptomycin often acts faster.
·
Relapsing fever: due to Borrelia
recurrentis responds adequately.
· Rickettsial
infections: typhus, rocky mountain spotted fever, Q
fever, etc. respond dramatically. Chloramphenicol is an alternative.
3. Tetracyclines
Are Second Choice Drugs:
a)
To penicillin/ampicillin for tetanus, anthrax,
actinomycosis and Listeria
infections.
b) To ceftriaxone,
amoxicillin or azithromycin for gonorrhoea, especially for penicillin resistant
non-PPNG; also in patients allergic to penicillin, but response rate has
decreased.
c)
To ceftriaxone for syphilis in patients
allergic to penicillin; early syphilis can be treated in 2 weeks but late
syphilis requires 1 month.
d) To penicillin for
leptospirosis; doxycycline 100 mg BD for 7 days is curative. Weekly doxycycline
(200 mg) has been used as prophylactic in subjects at risk during an epidemic.
e)
To azithromycin for pneumonia due to Chlamydia pneumoniae. Oral as well as
topical tetracycline has been used in
trachoma.
f)
To ceftriaxone/azithromycin for chancroid.
g) To streptomycin for tularemia.
4. Other Situations
In Which Tetracyclines May Be Used Are:
(a) Urinary tract
infections: Odd cases in which the organism has been found sensitive.
(b) Community acquired
pneumonia, when a more selective antibiotic cannot be used.
(c) Amoebiasis: along
with other amoebicides for chronic intestinal amoebiasis.
(d) As adjuvant to
quinine or sulfadoxine-pyrimethamine for chloroquine-resistant P. falciparum
malaria.
(e) Acne vulgaris: prolonged
therapy with low doses may be used in severe cases (since Propionibacterium acnes is sensitive to tetracyclines), but simpler treatments are preferred in
most cases (see Ch. No. 64).
(f) Chronic obstructive
lung disease: prophylactic use may reduce the frequency of exacerbations, but
the risk : benefit ratio is controversial.
