Structures of the Nephron
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Urinary System
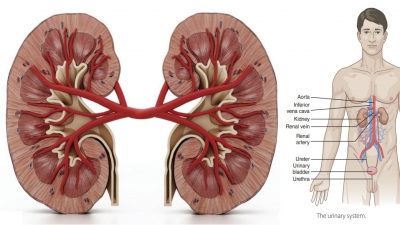
The functional units of the kidneys are the nephrons, in which 85% are cortical nephrons , located almost totally within the superficial cortex. There are about one million nephrons in a kidney, each consisting of renal corpuscle and a renal tubule.
Structures of the Nephron
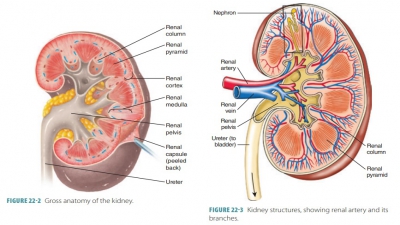
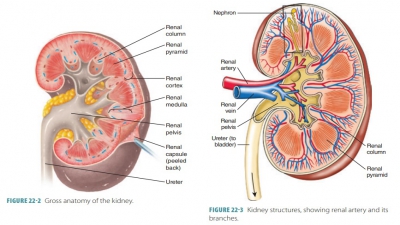
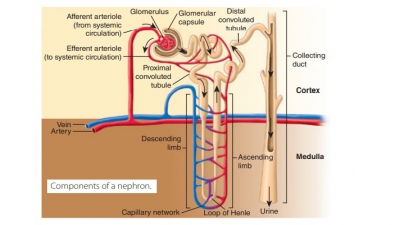
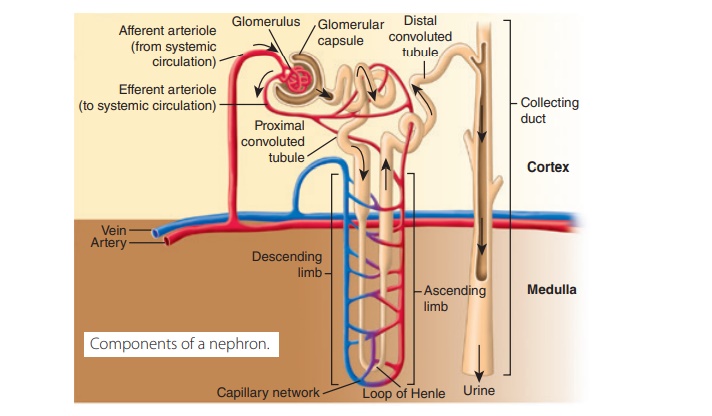
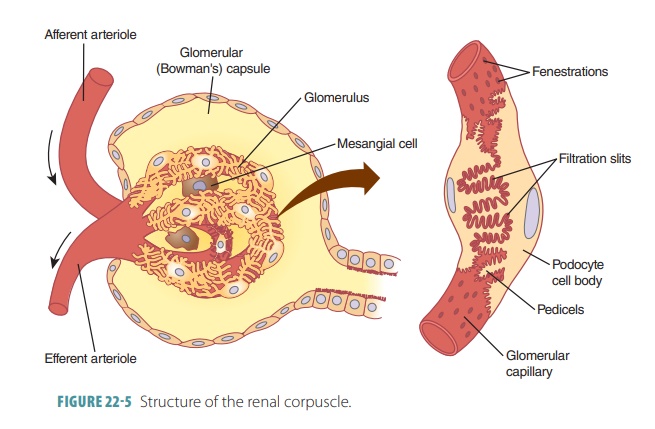
The functional units of the kidneys are the nephrons, in which 85% are cortical nephrons , located almost totally within the superficial cortex. There are about one million nephrons in a kidney, each consisting of renal corpuscle and a renal tubule (FIGURE 22-4). The renal corpuscle is a spherical structure. It consists of the glomerular (Bowman’s) capsule, which is a cup-shaped structure almost 200 micrometers in diameter and a capillary network that is called the glomerulus. The renal tubule is a long tube, up to 50 millimeters in length, and begins at the renal corpuscle. The three major sections of each renal tubule are the proximal convoluted tubule, nephron loop, and distal convoluted tubule. The renal tubule leaves the glomerular capsule as the highly coiled proximal convoluted tubule (FIGURE 22-5). This makes a tight loop called the nephron loop. It then winds and twists some more to become the distal convoluted tubule, which empties into a collecting duct. The outer wall of the glomerular capsule is lined with a simple squa-mous capsular epithelium that is continuous with the visceral epithelium covering the glomerular capillaries. The capsular and visceral epithelia are separated by a capsular space.
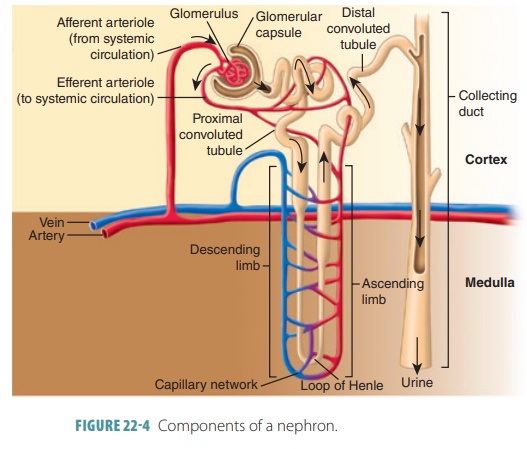
The proximal convoluted tubule cells reabsorb water, ions, organic nutrients, and plasma proteins when they are present from the tubular fluid. They are released into the peritubular fluid, which is the fluid that surrounds the renal tubule. Filtrate moves from the renal corpuscle through the proximal con-voluted tubule first, then the nephron loop, and finally the distal convoluted tubule. The many twists and turns of the renal tubules means they actually would be much longer if straightened out. These con-volutions also increase their ability to process filtrate. Both the renal tubule and collecting duct are made up of just one layer of polar epithelial cells above a basement membrane, but they differ in their histology. The distal convoluted tubule passes between afferent and efferent arterioles and also comes into contact with them.
Parts of the Renal Tubule
The walls of the proximal convoluted tubule are made up of cuboidal epithelial cells that have large mito-chondria. Dense microvilli are found on their luminal apical surfaces, forming a brush border that is similar to the one in the intestines. The brush border increases the surface area and reabsorption capabilities to a large degree. It easily reabsorbs water and solutes from the filtrate while secreting substances into it.
The proximal convoluted tubule dips toward the renal pelvis to form the descending limb of the U-shaped nephron loop, formerly called the loop of Henle. In this location, urine is concentrated. This structure is also described as having a “horseshoe shape.” The proximal area of the descending limb is continuous with the proximal tubule and has similar types of cells. It then curves toward the renal corpus-cle to form the ascending limb of the nephron loop. The ascending limb has a thick segment in most neph-rons, but in others its thin segment extends around a bend to form the ascending thin limb. This returns to the renal corpuscle region, coiling tightly to become the distal convoluted tubule. This tubule’s epithelial cells are similar to those of the proximal convoluted tubule, in that they are cuboidal and only found in the cortex. However, they are thinner and have very few microvilli. These tubules, which receive filtrate from several nephrons, merge to form collecting ducts in the renal cortexes. They pass into the renal medulla, resulting in tubes that empty into the minor calyces through openings in the renal papillae. The exchanges between the ascending and descending limbs of the nephron loop are referred to as countercurrent mul-tiplication, because the fluids are moving in opposite directions.
The collecting ducts are responsible for main-taining the water and sodium ion balance of the body. Their type A (principal cells) and type B (intercalated cells) play various roles in balancing acids and bases in the blood. Thousands of collecting ducts collect fluid, each one from many nephrons, and move it to the renal pelvis. The ducts run through medullary pyramids, causing them to appear striped. Nearing the renal pelvis, the collecting ducts become fused, delivering urine to the minor calyces through the papillae of the pyramids. Fusion of collecting ducts forms larger papillary ducts.
Capillary Beds of the Nephron
Each nephron’s renal tubule is linked to a glomerulus and the peritubular capillaries. Also, juxtamedullary nephrons use the vasa recta, which are specialized capillaries. A glomerulus is a tangled cluster of par-allel blood capillaries that comprises a renal corpuscle. All renal corpuscles are located in the renal cortex, but the renal tubules begin in the cortex and continue into the medulla, finally returning to the cortex. The glomerular capillaries are unique in that they are fed by an afferent arteriole and drained by an efferent arteriole (Figure 22-5). Blood, minus filtered fluids, is actually what drains out via the efferent arteriole. Having both types of arterioles keeps the pressure high in the glomerulus, so filtration can be effective.
Efferent arterioles are smaller in diameter than afferent arterioles and resist blood flow slightly. They branch into complex, interconnected capillary net-works, each called a peritubular capillary, which surrounds the renal tubule. The low-pressure blood inside eventually enters the venous system of the kidney. The peritubular capillaries are tightly located to renal tubules, emptying into local venules. Their pressure is low because they arise from efferent arteri-oles, which have high resistance. The porous peritubu-lar capillaries can, therefore, easily absorb water and solutes from renal tubule cells during their reclama-tion from the filtrate. Because the renal tubules are so closely aligned together, each nephron’s peritubular capillaries absorb substances from several nearby nephrons.
A lot of fluid is produced by filtration. Approx-imately, 99% of it is reabsorbed by renal tubule cells to be returned to the blood via the beds of the peritu-bular capillaries. The cortical radiate arteries running through the renal cortex give rise to the afferent arte-rioles. The peritubular capillaries or vasa recta are fed by various efferent arterioles.
The efferent arterioles that serve the juxtamedul-lary nephrons usually do not divide into peritubular capillaries but form bundles of long and straight vasa recta. The vasa recta are vessels extending deeply into the medulla, parallel to nephron loops, which are the longest found there. The vasa recta have very thin walls, helping to form concentrated urine.
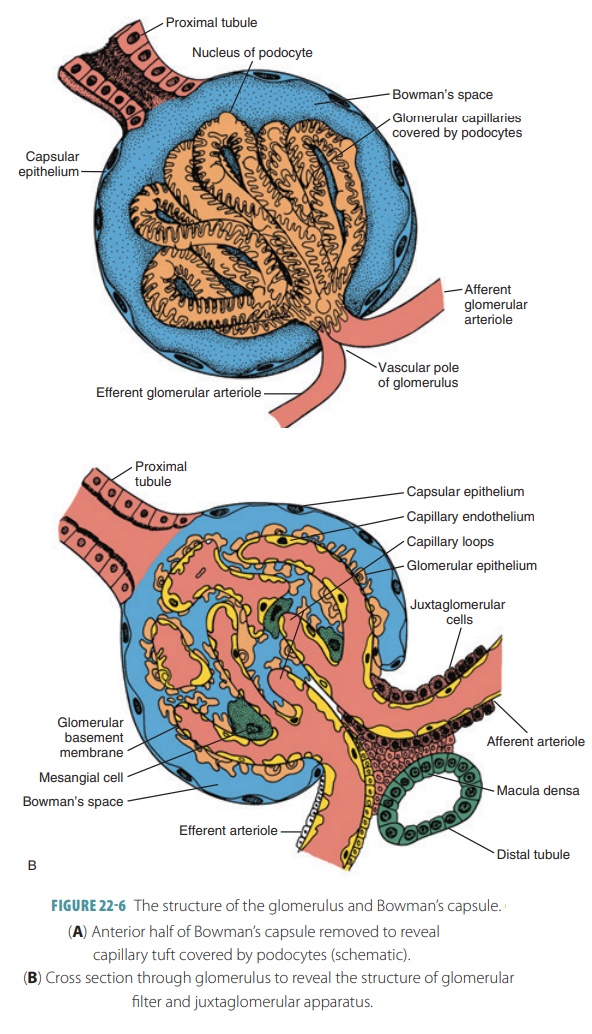
Juxtaglomerular Complex
The juxtaglomerular apparatus or complex of each nephron is where the ascending limb of the nephron loop’s most distal portion lies against an afferent arte-riole supplying the glomerulus (FIGURE 22- 6A and B). It may also lie against an efferent arteriole. Modifica-tions of structure exist where the ascending limb and afferent arteriole meet. Each juxtaglomerular appara-tus has three types of cells regulating filtrate formation rates and systemic blood pressure: the macula densa, granular cells, and extraglomerular mesangial cells.
The macula densa is a thickening in the wall of the distal tubule of the kidney nephron, at a point where it is in contact with the afferent glomerulus. The macula densa cells act as chemoreceptors. They monitor the filtrate’s sodium chloride content as it enters the dis-tal convoluted tubule. The granular or juxtaglomerular cells in the arteriolar walls are enlarged smooth muscle cells. They have large secretory granules containing renin, an enzyme. Granular cells act as mechanore-ceptors. They monitor blood pressure of the afferent arteriole. Extraglomerular mesangial cells between the arteriole and tubule cells are interconnected via gap junctions. They are believed to pass signals that have regulatory functions between the macula densa and granular cells.
1. Describe the structures of the nephron.
2. Define the terms “renal tubule,” “nephron loop,” and “glomerulus.”
3. Describe the tubular components of each nephron and how filtrate passes through them.
4. Contrast the glomerulus and peritubular capillaries.