Stages of Anaesthesia
| Home | | Pharmacology |Chapter: Essential pharmacology : General Anaesthetics
GAs cause an irregularly descending depression of the CNS, i.e. the higher functions are lost first and progressively lower areas of the brain are involved, but in the spinal cord lower segments are affected somewhat earlier than the higher segments.
STAGES OF ANAESTHESIA
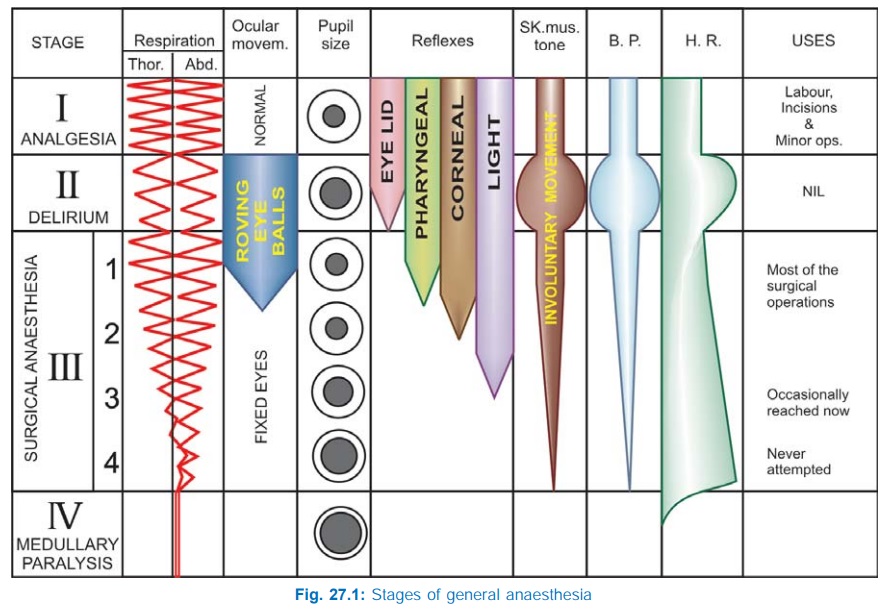
GAs cause an irregularly descending depression of the CNS, i.e. the higher functions are lost first and progressively lower areas of the brain are involved, but in the spinal cord lower segments are affected somewhat earlier than the higher segments. The vital centres located in the medulla are paralysed the last as the depth of anaesthesia increases. Guedel (1920) described four stages with ether anaesthesia, dividing the stage into 4 planes. These clearcut stages are not seen nowadays with the use of faster acting GAs, premedication and employment of many drugs together. The precise sequence of events differs somewhat with anaesthetics other than ether. However, ether continues to be used in India and description of these stages still serves to define the effects of light and deep anaesthesia. Important features of different stages are depicted in Fig. 27.1.
I. Stage Of Analgesia
Starts from beginning of anaesthetic inhalation and lasts upto the loss of consciousness. Pain is progressively abolished. Patient remains conscious, can hear and see, and feels a dream like state; amnesia develops by the end of this stage. Reflexes and respiration remain normal.
Though some minor operations can be carried out during this stage, it is rather difficult to maintain—use is limited to short procedures.
II. Stage Of Delirium
From loss of consciousness to beginning of regular respiration. Apparent excitement is seen—patient may shout, struggle and hold his breath; muscle tone increases, jaws are tightly closed, breathing is jerky; vomiting, involuntary micturition or defecation may occur. Heart rate and BP may rise and pupils dilate due to sympathetic stimulation.
No stimulus should be applied or operative procedure carried out during this stage. This stage is inconspicuous in modern anaesthesia.
III. Surgical Anaesthesia
Extends from onset of regular respiration to cessation of spontaneous breathing. This has been divided into 4 planes which may be distinguished as:
Plane 1 Roving eyeballs. This plane ends when eyes become fixed.
Plane 2 Loss of corneal and laryngeal reflexes.
Plane 3 Pupil starts dilating and light reflex is lost.
Plane 4 Intercostal paralysis, shallow abdominal respiration, dilated pupil.
As anaesthesia passes to deeper planes, progressively—muscle tone decreases, BP falls, HR increases with weak pulse, respiration decreases in depth and later in frequency also— thoracic lagging behind abdominal.
IV. Medullary Paralysis
Cessation of breathing to failure of circulation and death. Pupil is widely dilated, muscles are totally flabby, pulse is thready or imperceptible and BP is very low.
Many of the above indices have been robbed by the use of atropine (pupillary, heart rate), morphine (respiration, pupillary), muscle relaxants (muscle tone, respiration, eye movements, reflexes) etc. and the modern anaesthetist has to depend on several other observations to gauge the depth of anaesthesia.
a) If eyelash reflex is present and patient is making swallowing movements—stage II has not been reached.
b) Loss of response to painful stimulus (e.g. pressure on the upper nasal border of orbit)
— stage III has been reached.
c) Incision of the skin causes reflex increase in respiration, BP rise or other effects; insertion of endotracheal tube is resisted and induces coughing, vomiting, laryngospasm; tears appear in eye; passive inflation of lungs is resisted—anaesthesia is light.
d) Fall in BP, cardiac and respiratory depression are signs of deep anaesthesia.
In the present day practice anaesthesia is generally kept light; adequate analgesia, amnesia and muscle relaxation are produced by the use of intravenous drugs. Premedication with CNS depressants and opioids or their concurrent use lowers MAC of the inhaled anaesthetic. When a combination of two inhalational anaesthetics (e.g. N2O + isoflurane) is used, their MACs are additive: lower concentration of each is required. The doseresponse relationship of inhaled anaesthetics is very steep; just 10% higher concentration (1.1 MAC) immobilizes >90% subjects. Concentrations of inhalational anaesthetics exceeding 1.2 MAC are rarely used, and 2–3 MAC is often lethal.
Related Topics
