Renal Excretion
| Home | | Pharmacology |Chapter: Essential pharmacology : Pharmacokinetics; Metabolism Excretion Of Drugs, Kinetics Of Elimination
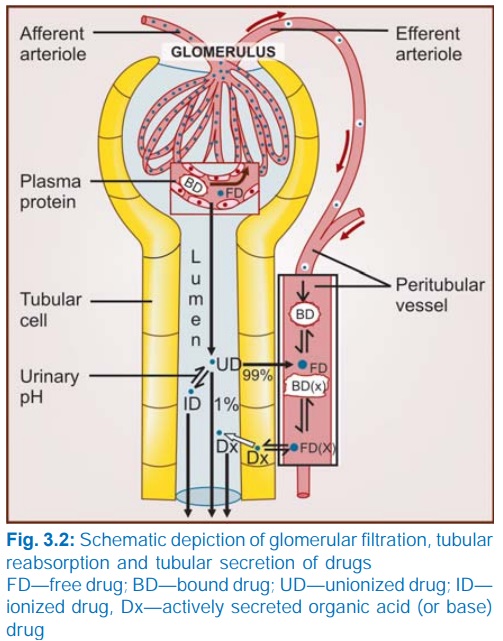
The kidney is responsible for excreting all water soluble substances. The amount of drug or its metabolites ultimately present in urine is the sum total of glomerular filtration, tubular reabsorption and tubular secretion.
RENAL EXCRETION
The kidney is
responsible for excreting all water soluble substances. The amount of drug or
its metabolites ultimately present in urine is the sum total of glomerular
filtration, tubular reabsorption and tubular secretion (Fig. 3.2).
Net renal =
(Glomerular filtration + tubular excretion)
Glomerular Filtration
Glomerular capillaries have pores larger than usual; all nonprotein
bound drug (whether lipidsoluble or insoluble) presented to the glomerulus is
filtered. Thus, glomerular filtration of a drug depends on its plasma protein
binding and renal blood flow. Glomerular filtration rate (g.f.r.), normally ~
120 ml/min, declines progressively after the age of 50, and is low in renal
failure.
Tubular Reabsorption
This occurs by passive diffusion and depends on lipid solubility and
ionization of the drug at the existing urinary pH. Lipidsoluble drugs filtered
at the glomerulus back diffuse in the tubules because 99% of glomerular
filtrate is reabsorbed, but nonlipidsoluble and highly ionized drugs are unable
to do so. Thus, rate of excretion of such drugs, e.g. aminoglycoside antibiotics,
quaternary ammonium compounds parallels g.f.r. (or creatinine clearance).
Changes in urinary pH affect tubular reabsorption of drugs that are partially
ionized
Weak bases ionize more and are less reabsorbed
in acidic urine.
Weak acids ionize more and are less reabsorbed
in alkaline urine.
This principle is
utilized for facilitating elimination of the drug in poisoning, i.e. urine is
alkalinized in barbiturate and salicylate poisoning. Though elimination of weak
bases (morphine, amphetamine) can be enhanced by acidifying urine, this is not
practiced clinically, because acidosis can induce rhabdomyolysis, cardiotoxicity
and actually worsen outcome. The effect of changes in urinary pH on drug
excretion is greatest for those having pKa values between 5 to 8, because only
in their case pH dependent passive reabsorption is significant.
Tubular Secretion
This
is the active transfer of organic acids and
bases by two separate classes of relatively nonspecific transporters (OAT and
OCT) which operate in the proximal tubules. In addition, efflux transporters Pgp
and MRP2 are located in the luminal membrane of proximal tubular cells. If
renal clearance of a drug is greater than 120 mL/min (g.f.r.), additional
tubular secretion can be assumed to be occurring.
Active
transport of the drug across tubules reduces concentration of its free form in
the tubular vessels and promotes dissociation of protein bound drug, which
again is secreted (Fig. 3.2). Thus, protein binding, which is a hinderance for
glomerular filtration of the drug, is not so (may even be facilitatory) to
excretion by tubular secretion.
(a) Organic
acid transport (through OATP ) for penicillin, probenecid, uric acid,
salicylates, indomethacin, sulfinpyrazone, nitrofurantoin, methotrexate, drug
glucuronides and sulfates, etc.
(b) Organic base transport (through OCT) for thiazides, amiloride, triamterene, furosemide,
quinine, procainamide, choline, cimetidine, etc.
Inherently
both transport processes are bidirectional, i.e. they can transport their
substrates from blood to tubular fluid and vice
versa. However, for drugs and their metabolites (exogenous substances)
secretion into the tubular lumen predominates, whereas an endogenous substrate
like uric acid is predominantly reabsorbed.
Drugs
utilizing the same active transport compete with each other. Probenecid is an
organic acid which has high affinity for the tubular OATP. It blocks the active
transport of both penicillin and uric acid, but whereas the net excretion of
the former is decreased, that of the latter is increased.
This
is because penicillin is primarily secreted while uric acid is primarily
reabsorbed. Many drug interactions occur due to competition for tubular
secretion, e.g.
Salicylates block uricosuric action of probenecid and
sulfinpyrazone and decrease tubular secretion of methotrexate.
Probenecid decreases the concentration of nitrofurantoin in
urine, increases the duration of action of penicillin/ampicillin and impairs
secretion of methotrexate.
Sulfinpyrazone inhibits excretion of tolbutamide.
Quinidine decreases renal and biliary clearance of digoxin by inhibiting
efflux carrier Pgp.
Tubular
transport mechanisms are not well developed at birth. As a result, duration of
action of many drugs, e.g. penicillin, cephalosporins, aspirin is longer in
neonates. These systems mature during infancy. Renal function again
progressively declines after the age of 50 years; renal clearance of most drugs
is substantially lower in the elderly (>75 yr).
