Quinolones
| Home | | Pharmacology |Chapter: Essential pharmacology : Sulfonamides, Cotrimoxazole And Quinolones
These are synthetic antimicrobials having a quinolone structure that are active primarily against gram-negative bacteria, though newer fluorinated compounds also inhibit gram-positive ones.
QUINOLONES
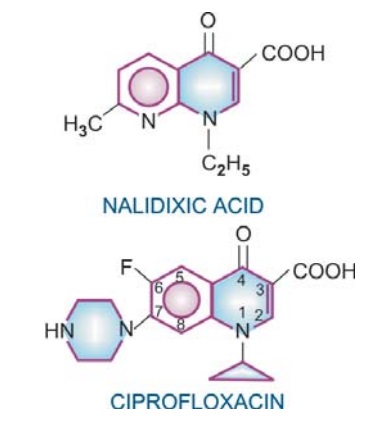
These are synthetic antimicrobials having a quinolone structure that are active primarily against gram-negative bacteria, though newer fluorinated compounds also inhibit gram-positive ones. The first member Nalidixic acid introduced in mid1960s had usefulness limited to urinary and g.i. tract infections because of low potency, modest blood and tissue levels, limited spectrum and high frequency of bacterial resistance. A breakthrough was achieved in the early 1980s by fluorination of the quinolone structure at position 6 and introduction of a piperazine substitution at position 7 resulting in derivatives called fluoroquinolones with high potency, expanded spectrum, slow development of resistance, better tissue penetration and good tolerability.
Nalidixic acid
It is active against gram-negative bacteria, especially coliforms: E. coli, Proteus, Klebsiella, Enterobacter, Shigella but not Pseudomonas. It acts by inhibiting bacterial DNA gyrase and is bactericidal. Resistance to nalidixic acid develops rather rapidly.
Nalidixic acid is absorbed orally, highly plasma protein bound and partly metabolized in liver: one of the metabolites is active. It is excreted in urine with a plasma t½ ~8 hrs. Concentration of the free drug in plasma and most tissues attained with the usual doses is nontherapeutic for systemic infections (MIC values for most susceptible bacteria just approach the ‘breakpoint’ concentration). However, high concentration attained in urine (20–50 times that in plasma) is lethal to the common urinary pathogens.
Adverse Effects
These are relatively infrequent, consist mostly of g.i. upset and rashes.
Most important toxicity is neurological—headache, drowsiness, vertigo, visual disturbances, occasionally seizures (especially in children).
Phototoxicity is rare. Individuals with G6PD deficiency may develop haemolysis. Nalidixic acid is contraindicated in infants.
Dose: 0.5–1 g TDS or QID; GRAMONEG, WINTOMYLON, URODIC, 0.5 g tab, 0.3 g/5 ml syrup.
Use
1. Nalidixic acid is primarily used as a urinary antiseptic, generally as a second line drug in recurrent cases or on the basis of sensitivity reports.
Nitrofurantoin should not be given concurrently—antagonism occurs.
2. It has also been employed in diarrhoea caused by Proteus, E. coli, Shigella or Salmonella, and has a special place in ampicillin resistant Shigella enteritis.
FLUOROQUINOLONES
These are quinolone antimicrobials having one or more fluorine substitutions. The ‘first generation’ fluoroquinolones (FQs) introduced in 1980s have one fluoro substitution. In the 1990s, compounds with additional fluoro and other substitutions have been developed—further extending antimicrobial activity to gram-positive cocci and anaerobes, and/or confering metabolic stability (longer t½). These are referred to as ‘second generation’ FQs.
First Generation Fluoroquinolones
Norfloxacin Ofloxacin
Ciprofloxacin Pefloxacin
Second Generation Fluoroquinolones
Lomefloxacin Sparfloxacin
Levofloxacin Gatifloxacin
Moxifloxacin
Mechanism Of Action
The FQs inhibit the enzyme bacterial DNA gyrase, which nicks double-stranded DNA, introduces negative supercoils and then reseals the nicked ends. This is necessary to prevent excessive positive supercoiling of the strands when they separate to permit replication or transcription. The DNA gyrase consists of two A and two B subunits: The A subunit carries out nicking of DNA, B subunit introduces negative supercoils and then A subunit reseals the strands. FQs bind to A subunit with high affinity and interfere with its strand cutting and resealing function. Recent evidence indicates that in gram-positive bacteria the major target of FQ action is a similar enzyme topoisomerase IV which nicks and separates daughter DNA strands after DNA replication. Greater affinity for topoisomerase IV may confer higher potency against gram-positive bacteria. The bactericidal action probably results from digestion of DNA by exonucleases whose production is signalled by the damaged DNA.
In place of DNA gyrase or topoisomerase IV, the mammalian cells possess an enzyme topoisomerase II (that also removes positive supercoils) which has very low affinity for FQs— hence the low toxicity to host cells.
Mechanism Of Resistance
Because of the unique mechanism of action, plasmid mediated transferable resistance probably does not occur. Resistance noted so far is due to chromosomal mutation producing a DNA gyrase or topoisomerase IV with reduced affinity for FQs, or due to reduced permeability/increased efflux of these drugs across bacterial membranes. In contrast to nalidixic acid which selects single step resistant mutants at high frequency, FQ-resistant mutants are not easily selected. Therefore, resistance to FQs has been slow to develop. However, increasing resistance has been reported among Salmonella, Pseudomonas, staphylococci, gonococci and pneumococci.
Ciprofloxacin (prototype)
It is the most potent first generation FQ active against a broad range of bacteria, the most susceptible ones are the aerobic gram-negative bacilli, especially the Enterobacteriaceae and Neisseria. The MIC of ciprofloxacin against these bacteria is usually < 0.1 μg/ml, while gram-positive bacteria are inhibited at relatively higher concentrations. The spectrum of action is summarized below:
Highly Susceptible
E. coli
Neisseria gonorrhoeae
K. pneumoniae
N. meningitidis
Enterobacter
H. influenzae
Salmonella typhi
H. ducreyi
other Salmonella
Campylobacter jejuni
Shigella
Yersinia enterocolitica
Proteus
Vibrio cholerae
Moderately Susceptible
Pseudomonas aeruginosa
Legionella
Staph. aureus
Brucella
(including few MRSA)
Listeria
Staph. epidermidis
Bacillus anthracis
Branhamella catarrhalis
Mycobact. tuberculosis
Organisms which have shown low/variable susceptibility are: Strep. pyogenes, Strep. faecalis, Strep. pneumoniae, Mycoplasma, Chlamydia, Mycobact. kansasii, Mycobact. avium.
Notable resistant bacteria are: Bacteroides fragilis, Clostridia, anaerobic cocci.
The remarkable microbiological features of ciprofloxacin (also other FQs) are:
· Rapidly bactericidal activity and high potency: MBCs are close to MICs.
· Relatively long post-antibiotic effect on Enterobacteriaceae, Pseudomonas and Staph.
· Low frequency of mutational resistance.
· Low propensity to select plasmid type resistant mutants.
· Protective intestinal streptococci and anaerobes are spared.
· Active against many βlactam and aminoglycoside resistant bacteria.
· Less active at acidic pH.
Pharmacokinetics
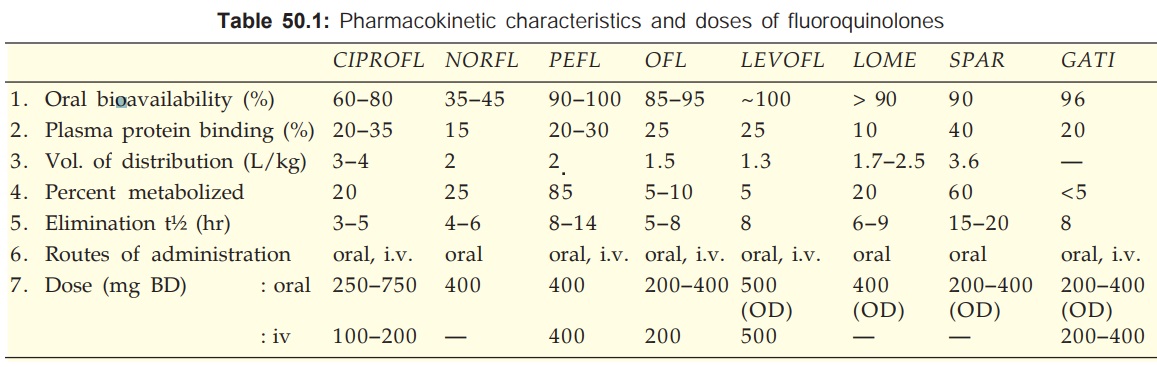
Ciprofloxacin is rapidly absorbed orally, but food delays absorption, and first pass metabolism occurs. The pharmacokinetic characteristics are given in Table 50.1. The most prominent feature of ciprofloxacin (and other FQs) is high tissue penetrability: concentration in lung, sputum, muscle, bone, prostate and phagocytes exceeds that in plasma, but CSF and aqueous levels are lower. It is excreted primarily in urine, both by glomerular filtration and tubular secretion. Urinary and biliary concentrations are 10–50 fold higher than plasma.
Adverse Effects
Ciprofloxacin has good safety record: side effects occur in ~10% patients, but are generally mild; withdrawal is needed only in 1.5%.
· Gastrointestinal: nausea, vomiting, bad taste, anorexia. Because gut anaerobes are not affected—diarrhoea is infrequent.
· CNS: dizziness, headache, restlessness, anxiety, insomnia, impairment of concentration and dexterity (caution while driving), tremor. Seizures are rare, occur only at high doses or when predisposing factors are present: possibly reflect GABA antagonistic action of FQs.
· Skin/hypersensitivity: rash, pruritus, photosensitivity, urticaria, swelling of lips, etc. Serious cutaneous reactions are rare.
· Tendonitis and tendon rupture: a few cases have been reported.
Ciprofloxacin and other FQs are contraindicated during pregnancy.
On the basis of the finding that administered to immature pups ciprofloxacin (and other FQs) caused cartilage damage in weight bearing joints, the FQs have been contraindicated in children. However, under pressing situations like Pseudomonas pneumonia in cystic fibrosis and multi-resistant typhoid, ciprofloxacin has been administered to millions of children in India and elsewhere. Though a few cases of joint pain and swelling have been reported, cartilage damage has not occurred. Caution may seem prudent while using FQs in children.
Interactions
· Plasma concentration of theophylline, caffeine and warfarin are increased by ciprofloxacin (also by norfloxacin and pefloxacin) due to inhibition of metabolism: toxicity of these drugs can occur.
· NSAIDs may enhance the CNS toxicity of FQs; seizures are reported.
· Antacids, sucralfate and iron salts given concurrently reduce absorption of FQs.
CIFRAN, CIPLOX, CIPROBID, QUINTOR, CIPROLET 250, 500, 750 mg tab, 200 mg/100 ml i.v. infusion, 3 mg/ ml eye drops.
Uses
Ciprofloxacin is effective in a broad range of infections including some difficult to treat ones. Because of wide-spectrum bactericidal activity, oral efficacy and good tolerability, it is being extensively employed for blind therapy of any infection, but should not be used for minor cases or where gram-positive organisms and/or anaerobes are primarily causative. In severe infections, therapy may be initiated by i.v. infusion and then switched over to oral route.
1. Urinary Tract Infections: High cure rates, even in complicated cases or those with indwelling catheters/prostatitis, have been achieved. Chronic Pseudomonas infections respond less completely.
2. Gonorrhoea: Initially a single 500 mg dose was nearly 100% curative in nonPPNG as well as PPNG infections, but cure rate has declined in the recent years due to emergence of resistance.
3. Chancroid: 500 mg BD for 3 days is an excellent alternative to ceftriaxone/erythromycin.
4. Bacterial Gastroenteritis: Severe cases due to EPEC, Shigella, Salmonella and Campy. jejuni respond quickly. It has also been used to reduce stool volume in cholera.
5. Typhoid: Ciprofloxacin is the first choice drug in typhoid fever since chloramphenicol, ampicillin and cotrimoxazole have become unreliable due to development of resistance. In India and elsewhere up to 95% S. typhi isolates are sensitive to ciprofloxacin. However, increasing number of nonresponsive cases are being reported. A dose of 500–750 mg BD for 10 days is recommended. Patients unable to take the drug orally may be treated with 200 mg. i.v. 12 hourly in the beginning. Being bactericidal the advantages of ciprofloxacin are:
• Quick defervescence: On an average fever subsides in 4–5 days.
• Early abetment of symptoms; low incidence of complications and relapse.
• Prevention of carrier state due to cidal action, good penetration into infected cells, high biliary and intestinal mucosal concentration.
It can also be used to treat typhoid carriers (750 mg BD for 4–8 weeks) . This has been found to achieve 92% eradication rate compared to 50% by ampicillin.
6. Bone, Soft Tissue, Gynaecological And Wound Infections: caused by resistant Staph. and gram-negative bacteria: high cure rates have been obtained but prolonged treatment with high doses is required in osteomyelitis and joint infections. Used along with clindamycin/ metronidazole (to cover anaerobes) it is a good drug for diabetic foot.
7. Respiratory Infections: Ciprofloxacin should not be used as the primary drug because pneumococci and streptococci have low and variable susceptibility. However, it can treat Mycoplasma, Legionella, H. influenzae, Branh. catarrhalis and some streptococcal and pneumococcal infections besides gram-negative ones.
The USFDA has approved use of ciprofloxacin for post exposure treatment of inhalational anthrax which may occur due to bioterrorism.
8. Tuberculosis It is now frequently used as a component of combination chemotherapy against multidrug resistant tuberculosis. Recently, even FQresistant TB (extensively drug resistant or XDRTB) have arisen.
9. Gram-Negative Septicaemias: Parenteral ciprofloxacin may be combined with a third generation cephalosporin or an aminoglycoside.
10. Meningitis: Though penetration in CSF is not very good, ciprofloxacin has been successfully used in gram-negative bacterial meningitis, especially that occurring in immunocompromised patients or those with CSF shunts.
11. Prophylaxis: of infections in neutropenic/ cancer and other susceptible patients.
12. Conjunctivitis: by gram-negative bacteria: topical therapy is effective.
Alternative Drugs For Typhoid Fever
1. Other fluoroquinolones: Ofloxacin (400 mg BD), levofloxacin (500 mg OD/BD) and pefloxacin (400 mg BD) are nearly equally efficacious alternatives to ciprofloxacin.
2. Ceftriaxone: Currently, it is the most reliable and fastest acting bactericidal drug for enteric fever. Practically all S. typhi isolates, including multidrug resistant ones, are susceptible. However, it has to be injected i.v. (4 g daily for 2 days followed by 2 g/day till 2 days after fever subsides; children 75 mg/kg/day) and is expensive. Generally 7–10 days treatment is required. Being bactericidal, it also prevents relapses and carrier state. Ceftriaxone is to be preferred over FQs in children, pregnant women and in areas with FQ resistance.
Cefoperazone and cefotaxime are the other third generation cephalosporins used in typhoid.
3. Chloramphenicol : Since majority of S. typhi strains are now chloramphenicol resistant, it has become clinically unreliable. It is seldom used, only in case the local strain is known to be sensitive and clinical experience supports its use. It is administered orally (0.5 g 6 hourly till fever subsides, then 0.25 g 6 hourly for another 5–7 days), and is inexpensive.
4. Cotrimoxazole: It was effective in typhoid till plasmid mediated multidrug resistance spread among S. typhi. Now it is rarely used.
5. Ampicillin/amoxicillin: These antibiotics are no longer dependable therapy for typhoid because of multidrug resistance. Response rate is low and defervescence takes longer even in patients who respond.
6. Combination therapy: There is no evidence that combination of any two or more AMAs is better than the single drug to which the infecting strain of S. typhi is responsive.
Norfloxacin
It is less potent than ciprofloxacin: MIC values for most gram-negative bacteria are 2–4 times higher. Many Pseudomonas and gram-positive organisms are not inhibited at clinically attained concentrations. Moreover, it attains lower concentration in tissues. It is metabolized as well as excreted unchanged in urine.
Norfloxacin is primarily used for urinary and genital tract infections. It is also good for bacterial diarrhoeas, because high concentrations are present in the gut and anaerobic flora is not disturbed. Norfloxacin is not recommended for respiratory and other systemic infections, particularly where gram-positive cocci are involved.
NORBACTIN, NORFLOX 200, 400, 800 mg tab, 3 mg/ ml eye drops; UROFLOX, NORILET 200, 400 mg tab. BACIGYL 400 mg tab, 100 mg/5 ml syr.
Pefloxacin
It is the methyl derivative of norfloxacin; more lipid soluble, completely absorbed orally, penetrates tissues better and attains higher plasma concentrations. Passage into CSF is higher than other FQs—preferred for meningeal infections. It is highly metabolized—partly to norfloxacin which contributes to its activity. Pefloxacin has longer t½: cumulates on repeated dosing achieving plasma concentrations twice as high as after a single dose. Because of this it is effective in many systemic infections in addition to those of the urinary and g.i. tract, though the in vitro activity is similar to norfloxacin. Dose of pefloxacin needs to be reduced in liver disease, but not in renal insufficiency.
Pefloxacin is an alternative to ciprofloxacin for typhoid. However, it is less effective in gram-positive coccal and Listeria infections.
PELOX, 200, 400 mg tab, to be taken with meals; 400 mg/5 ml inj (to be diluted in 100–250 ml of glucose solution but not saline since it precipitates in presence of Cl¯ ions), PERTI, 400 mg tab.
Ofloxacin
This FQ is intermediate between ciprofloxacin and norfloxacin in activity against gram-negative bacteria, but it is comparable to or more potent than ciprofloxacin for gram-positive organisms and certain anaerobes. Good activity against Chlamydia and Mycoplasma has been noted: it is an alternative drug for nonspecific urethritis, cervicitis and atypical pneumonia. It also inhibits M. tuberculosis; can be used in place of ciprofloxacin. It is highly active against M. leprae: is being used in alternative multidrug therapy regimens.
Ofloxacin is relatively lipid soluble; oral bioavailability is high: attains higher plasma concentrations. Food does not interfere with its absorption. It is excreted largely unchanged in urine; dose needs to be reduced in renal failure.
Ofloxacin is comparable to ciprofloxacin in the therapy of systemic and mixed infections. It is particularly suitable for chronic bronchitis and other respiratory or ENT infections. Inhibition of theophylline metabolism is less marked.
Gonorrhoea has been treated with a single 200 mg dose. It is also useful in nongonococcal urethritis.
ZANOCIN, TARIVID 100, 200, 400 mg tab; 200 mg/100 ml i.v. infusion, ZENFLOX also 50 mg/5 ml susp. ZANOCIN, OFLOX, EXOCIN 0.3% eye drops.
Levofloxacin
It is the levoisomer of ofloxacin having improved activity against Strep. pneumoniae and some other gram-positive and gram-negative bacteria. Anaerobes are moderately susceptible. Oral bioavailability of levofloxacin is nearly 100%; oral and i.v. doses are similar. It is mainly excreted unchanged and a single daily dose is sufficient because of slower elimination.
Theophylline, warfarin, cyclosporine and zidovudine pharmacokinetics has been found to remain unchanged during levofloxacin treatment. The primary indication of levofloxacin is community acquired pneumonia and exacerbations of chronic bronchitis in which 87–96% cure rate has been obtained. High cure rates have been noted in sinusitis, enteric fevers, pyelonephritis and skin/soft tissue infections as well.
TAVANIC, GLEVO 500 mg tab, 500 mg/100 ml inj.
Lomefloxacin
It is a second generation difluorinated quinolone, equal in activity to ciprofloxacin but more active against some gram-negative bacteria and chlamydia. Because of longer t½ and persistence in tissues, it is suitable for single daily administration. It is primarily excreted unchanged in urine; dose needs to be reduced in renal insufficiency. Interaction with theophylline has not been noted, but warfarin levels are increased.
LOMEF400, LOMEDON, LOMADAY 400 mg tab.
LOMIBACT, LOX 0.3% eye drops.
Sparfloxacin
This second generation difluorinated quinolone has enhanced activity against gram-positive bacteria (especially Strep. pneumoniae, Staphylococcus, Enterococcus), Bacteroides fragilis, other anaerobes and mycobacteria. Its major indications include pneumonia, exacerbations of chronic bronchitis, sinusitis and other ENT infections. Reports suggest good efficacy in tuberculosis, MAC infection in AIDS patients and in leprosy. Also used for chlamydial infections. It does not alter the pharmacokinetics of theophylline and warfarin. However, it has caused a higher incidence of phototoxic reactions: recipients should be cautioned not to go out in the sun. Slight prolongation of QTc interval has been noted in 3% recipients; should be avoided in patients taking cisapride, tricyclic antidepressants, phenothiazines, class IA and class III antiarrhythmics, etc. Because of longer t½ it is suitable for single daily dosing.
TOROSPAR 200, 400 mg tab; SPARTA, SPARQUIN, SPARDAC 100, 200 mg tab, ZOSPAR, SPARC, EYPAR 0.3% eye drops.
Gatifloxacin
Another 2nd generation FQ that has excellent activity against Strep. pneumoniae, many atypical respiratory pathogens including Chlamydia pneumoniae and certain anaerobes. M. tuberculosis is also inhibited. A greater affinity for topoisomerase IV may be responsible for improved activity against gram-positive cocci. The major indication of gatifloxacin is communityacquired pneumonia, exacerbation of chronic bronchitis, and other upper/lower respiratory tract infections.
MYGAT 200, 400 mg tab, 400 mg/200 ml inj; GATIQIN 200, 400 mg tab, GAITY 200, 400 mg tab, 400 mg/40 ml inj. GATICIN, GATIQUIN 0.3% eye drops.
Gatifloxacin has the potential to cause tachycardia and prolong QTc interval; contraindicated in hypokalaemia and with other drugs that can prolong QT. Phototoxicity, CNS effects and swelling over face are other side effects.
Changes in blood glucose level have been reported, and there is some risk of Torsades de pointes. It has been discontinued in USA, and is not available in the UK.
Moxifloxacin
It is also a long-acting 2nd generation FQ having high activity against Str. pneumoniae, other gram-positive bacteria including βlactam/macrolide resistant ones and some anaerobes. It is the most potent FQ against M. tuberculosis. Bacterial topoisomerase IV is the major target of action. Moxifloxacin is primarily used for pneumonias, bronchitis, sinusitis, otitis media, in which efficacy is comparable to βlactam antibiotics. However, it is not good for urinary tract infections. Side effects are similar to other FQs. It should not be given to patients predisposed to seizures and to those receiving proarrhythmic drugs, because it can prolong QTc interval. Phototoxicity occurs only rarely.
Dose: 400 mg OD; MOXIF 400 mg tab; STAXOM 400 mg tab, 400 mg/250 ml i.v. infusion.
MOXICIP, MILFLOX 0.5% eye drops for conjunctivitis caused by gram-positive as well as negative bacteria/.
