Progestins
| Home | | Pharmacology |Chapter: Essential pharmacology : Estrogens, Progestins and Contraceptives
These are substances which convert the estrogen primed endometrium to secretory and maintain pregnancy in animals spayed after conception (Progestin = favouring pregnancy).
PROGESTINS
These are substances which convert the estrogen primed
endometrium to secretory and maintain pregnancy in animals spayed after
conception (Progestin = favouring
pregnancy).
At the turn of the last century it became apparent that ovaries
secrete two hormones, and that corpus luteum was essential for maintenance of
pregnancy. Progesterone was isolated in 1929, but its full therapeutic
potential has been exploited only after the 1950s when a large number of orally
active synthetic progestins were developed.
Natural Progestin
Progesterone, a 21 carbon steroid, is the
natural progestin and is derived from cholesterol. It is secreted by the corpus
luteum (10–20 mg/day) in the later half of menstrual cycle under the influence
of LH. Its production declines a few days before the next menstrual flow. If
the ovum gets fertilized and implants—the blastocyst immediately starts
producing chorionic gonadotropin which is absorbed and sustains the corpus
luteum in early pregnancy. Placenta starts secreting lots of estrogens and
progesterone from 2nd trimester till term. Men produce 1–5 mg progesterone per
day from adrenals and testes— its role if any, in males is not known.
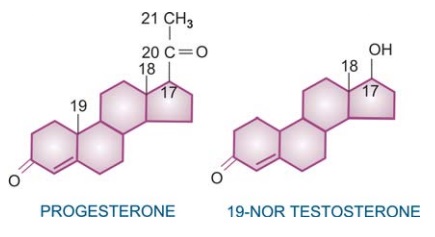
Synthetic Progestins
A number of synthetic progestins with high
oral activity have been produced. These are either progesterone derivatives (21
C) or 19nortestosterone derivatives (18 C).
The progesterone derivatives are almost pure progestins, have
weaker anti-ovulatory action and are used primarily as adjuvants to estrogens
for HRT in postmenopausal women, threatened abortion, endometriosis, etc. for
selective progestational effect. The older 19nortestosterone derivatives
developed in the 195060s have additional weak estrogenic, weak androgenic, anabolic
and potent anti-ovulatory action: are used primarily in combined contraceptive
pills. Norgestrel has a 13ethyl
substitution (termed gonane)—is more
potent (especially its levo isomer levonorgestrel).
In the 1980-90s a number of other gonane 19nortestosterone
compounds were introduced, of which desogestrel
has been marketed in India. Desogestrel and norgestimate
are prodrugs. In addition to being very potent progestins they have strong anti-ovulatory
action (gestodene inhibits ovulation
at as low as 40 μg/day dose), and little or no androgenic property. Therefore,
they do not antagonise the beneficial action of estrogens on lipid profile and
are preferable in women with hyperandrogenemia. High anti-ovulatory potency
allows reduction of ethinylestradiol dose when these are combined in oral
contraceptives.
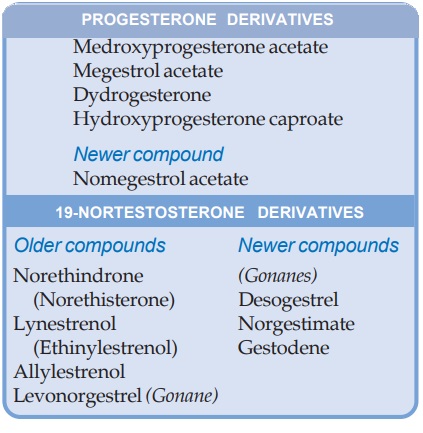
The newer 19norprogesterone
derivative nomegestrol has
antiandrogenic property, is less anti-ovulatory,
but has strong effect on endometrium.
Actions
The main function of
progesterone is preparation of the uterus for nidation and maintenance of
pregnancy. The latter is due to prevention of endometrial shedding, decreased
uterine motility and inhibition of immunological rejection of the foetus:
progesterone depresses Tcell function and cellmediated immunity (CMI).
1. Uterus
Progesterone brings about secretory changes in the estrogen primed endometrium:
hyperemia, tortuocity of glands and increased secretion occurs while epithelial
proliferation is suppressed. It is lack of progestational support which causes mucosal
shedding during menstruation.
Continued action of
progesterone (as when pregnancy occurs) brings about decidual changes in
endometrium—stroma enlarges and becomes spongy, glands atrophy. It also
decreases sensitivity of myometrium to oxytocin.
2. Cervix
Progesterone converts the watery cervical secretion induced by estrogens to
viscid, scanty and cellular secretion which is hostile to sperm penetration.
3. Vagina
Progesterone induces pregnancy like changes in the vaginal mucosa—leukocyte
infiltration of cornified epithelium.
4. Breast
Progesterone
causes proliferation of acini in the mammary
glands. Cyclic epithelial proliferation occurs during luteal phase, but continuous
exposure to progesterone during pregnancy halts mitotic activity and stabilizes
mammary cells. Acting in concert with estrogens, it prepares breast for
lactation. Withdrawal of these hormones after delivery causes release of
prolactin from pituitary and milk secretion starts.
5. CNS
High circulating concentration of progesterone (during pregnancy)
appears to have a sedative effect.
6. Body Temperature
It causes a slight (0.5oC) rise in body
temperature by resetting the hypothalamic thermostat and increasing heat
production. This is responsible for the higher body temperature seen during the
luteal phase.
7. Respiration
Progestins in relatively higher doses stimulate respiration, as occurs during
pregnancy.
8. Metabolism
Prolonged use of oral contraceptives impairs
glucose tolerance in some women. This has been ascribed to the progestational
component. Progestins, especially those with androgenic activity (19nortestosterone
derivatives) tend to raise LDL and lower HDL levels. This may reduce the
beneficial effect of estrogen used concurrently in HRT or in contraceptives.
Micronized oral progesterone formulation (referred to as ‘natural progesterone’ introduced recently has been shown not to
counteract the beneficial effect of estrogen on LDL and HDL.
9. Pituitary
Progesterone is a weak inhibitor of Gn secretion from
pituitary. It decreases the frequency of LH pulses by action on hypothalamic
pulse generator but increases the amount of LH secreted per pulse.
Administration of progestin during follicular phase suppresses the preovulatory
LH surge and prevents ovulation; synergises with estrogen for this action. The
gonane 19nortestosterone derivatives are potent anti-ovulatory drugs.
Mechanism Of Action
Unlike
other steroid receptors, the progesterone receptor (PR) has a limited
distribution in the body: confined mostly to the female genital tract, breast,
CNS and pituitary. The PR is normally present in the nucleus of target cells.
Analogous to ER, upon binding the hormone PR undergoes dimerization, attaches
to progesterone response element (PRE) of target genes and regulates
transcription through coactivators. The anti-progestins also bind to PR, but
the conformation assumed is different from agonist bound receptor and opposite
effects are produced by interaction with corepressors.
The
PR exists in a short (PRA) and a longer (PRB) isoforms. The two have differing
activities, but because the ligand binding domain of both is identical, all
agonists and antagonists display similar binding properties for them. Tissue
selective modulation of PR has not yet been possible, as has been in the case of
ER. Progesterone also acts on cell membrane receptors in certain tissues and
produces rapid effects, but they are probably not important physiologically.
Estrogens
have been shown to increase PR density, whereas progesterone represses ER and
enhances local degradation of estradiol.
Pharmacokinetics
Progesterone,
unless specially formulated, is inactive orally because of high first-pass
metabolism in liver. It is mostly injected i.m. in oily solution. Even after an
i.m. dose it is rapidly cleared from plasma, has a short t½ (5–7 min). It is
nearly completely degraded in the liver—major product is pregnanediol which is
excreted in urine as glucuronide and sulfate conjugates. However, effects of
progesterone last longer than the hormone itself.
A
micronized formulation of progesterone has been developed for oral
administration. Microfine particles of the drug are suspended in oil and
dispensed in gelatin capsules. Absorption occurs through lymphatics. Though
bioavailability is low, effective concentrations are attained in the body.
Most
of the synthetic progestins are orally active and are metabolized slowly; have
plasma t½ ranging from 8–24 hours.
Preparations And Dose
1.
Progesterone: 10–100 mg i.m. (as oily solution) OD; PROGEST, PROLUTON,
GESTONE 50 mg/ml inj., 1 and 2 ml amp; 100–400 mg OD oral: NATUROGEST, OGEST
100, 200, 400 mg caps containing micronized oily suspension.
2.
Hydroxyprogesterone caproate: 250–500 mg i.m. at 2–14 days intervals; PROLUTON DEPOT,
MAINTANE INJ, PROCAPRIN 250 mg/ml in 1 and 2 ml amp.
3. Medroxyprogesterone
acetate: 5–20 mg OD–BD oral, 50–150 mg i.m. at 1–3 month interval; FARLUTAL 2.5, 5, 10 mg tab., PROVERA,
MEPRATE, MODUS 2.5, 10 mg tab, DEPOTPROVERA 150 mg in 1 ml inj. (as contraceptive).
Has weak androgenic and antiestrogenic property.
4. Dydrogesterone:
5–10 mg OD/TDS oral; DUPHASTON 5 mg tab. It has poor anti-ovulatory
action: may be preferred when contraceptive effect is not required.
5. Norethindrone (Norethisterone): 5–10 mg OD–BD
oral; PRIMOLUTN, STYPTIN, REGESTRONE, NORGEST 5 mg tab; REGESTRONE
HRT, NORETA HRT 1 mg tab (for HRT); NORISTERAT 200 mg/ml
inj (as enanthate) for contraception 1 ml i.m every 2 months; has androgenic,
anabolic and antiestrogenic activity.
6.
Lynestrenol (Ethinylestrenol): 5–10 mg OD oral; ORGAMETRIL 5 mg tab. Has additional androgenic, anabolic and
estrogenic activity.
7. Allylestrenol:
10–40 mg/day; GESTANIN, FETUGARD, MAINTANE 5 mg tab. Has been especially used for
threatened/habitual abortion, PROFAR 25 mg tab.
8. Levonorgestrel:
0.1–0.5 mg/day; DUOLUTONL, OVRAL 0.25 mg+ ethinylestradiol 0.05 mg tab. Has androgenic, anabolic
and antiestrogenic property.
9. Desogestrel 150 μg + ethinylestradiol
30 μg (NOVELON) tab, 1 tab OD 3 week
on 1 week off cyclic therapy. (Other preparations are given with oral
contraceptives).
Adverse Effects
Ø Breast engorgement,
headache, rise in body temperature, edema, esophageal reflux, acne and mood
swings may occur with higher doses.
Ø Irregular bleeding or
amenorrhoea can occur if a progestin is given continuously.
ØThe 19nortestosterone
derivatives lower plasma HDL levels—may promote atherogenesis, but progesterone
and its derivatives have no such effect.
Ø Long-term use of
progestin in HRT may increase the risk of breast cancer.
Ø Blood sugar may rise
and diabetes may be precipitated by long-term use of potent agents like
levonorgestrel.
Ø Intramuscular
injection of progesterone is painful.
Ø Given in early pregnancy,
progestins can cause masculinization of female foetus and other congenital
abnormalities.
Their use for diagnosis
of pregnancy is now contraindicated.
Uses
a. As contraceptive Most common use (see later).
b. Hormone replacement therapy
(HRT) In nonhysterectomised postmenopausal women estrogen therapy is
supplemented with a progestin for 10–12 days each month to counteract the risk
of inducing endometrial carcinoma. A progesterone derivative lacking androgenic
activity is preferred.
c. Dysfunctional uterine bleeding It is often associated
with anovular cycles. Continued estrogenic action on endometrium (causing hyperplasia)
without progesterone induction and withdrawal resulting in incomplete sloughing
leads to irregular, often profuse bleeding. A progestin in relatively large
doses (norethindrone 20–40 mg/ day or equivalent) promptly stops bleeding and
keeps it in abeyance as long as given. Subsequently cyclic treatment
regularizes and normalizes menstrual flow. A progestin with inherent estrogenic
action is preferred; often supplemental dose of estrogen is combined.
d. Endometriosis It is due to the
presence of ectopic endometrium;
manifestations are dysmenorrhoea, painful pelvic swellings and infertility.
Continued administration of progestins induces an anovulatory, hypoestrogenic
state by suppressing Gn release. The direct action on endometrium prevents
bleeding in the ectopic sites by suppressing menstruation. Treatment for a few
months causes atrophy and regression of the ectopic masses; therapy can be withdrawn
in many cases after 6 months without reactivation. Fertility returns in a good
percentage. Progestin treatment of endometriosis is cheap and generally well
tolerated, but not all cases respond and recurrences are frequent. Danazol is
an effective alternative. Other drugs used are GnRH agonists and
antiprogestins.
e. Premenstrual syndrome/tension Some women develop headache, irritability, fluid
retention, distention and breast tenderness a few days preceding menstruation.
When depression predominates, it has been labelled ‘premenstrual dysphoric disorder’.
Fluoxetine and other SSRIs given daily on symptom days dampen irritability and
mood changes in majority of women. If severe, premenstrual syndrome requires
suppression of ovulation by combined estrogen-progesterone treatment given
cyclically. Relatively higher dose of progestin is generally used. Progestins
are added to estrogen when it is used for severe dysmenorrhoea.
f. Threatened/habitual abortion In most such patients there is no
progesterone deficiency; administration of excess hormone is of no benefit.
Progestin therapy may be considered in those patients who have established
deficiency. However, progestins are briskly promoted and almost routinely
prescribed in India. There is some recent evidence of its efficacy in
preventing premature delivery in high risk pregnancy. If such use is made—a
pure progestin without estrogenic or androgenic activity should be employed.
e. Endometrial carcinoma Progestins are palliative
in about 50% cases of advanced/ metastatic endometrial carcinoma. High doses
are needed.
Related Topics
