Pharmacological Actions & Pharmacokinetics
| Home | | Pharmacology |Chapter: Essential pharmacology : Anticholinergic Drugs And Drugs Acting On Autonomic Ganglia
The actions of atropine can be largely predicted from knowledge of parasympathetic responses. Prominent effects are seen in organs which normally receive strong parasympathetic tone. It blocks all subtypes of muscarinic receptors.
PHARMACOLOGICAL ACTIONS
(Atropine As Prototype)
The
actions of atropine can be largely predicted from knowledge of parasympathetic
responses.
Prominent
effects are seen in organs which normally receive strong parasympathetic tone.
It blocks all subtypes of muscarinic receptors.
1. CNS
Atropine has an overall CNS stimulant action. However, these effects are not
appreciable at low doses which produce only peripheral effects because of
restricted entry into the brain. Hyoscine produces central effects (depressant)
even at low doses.
o Atropine stimulates many
medullary centres —vagal, respiratory, vasomotor.
o It depresses
vestibular excitation and has antimotion sickness property. The site of this
action is not clear—probably there is a cholinergic link in the vestibular
pathway, or it is exerted at the cortical level.
o By blocking the relative
cholinergic overactivity in basal ganglia, it suppresses tremor and rigidity of
parkinsonism.
o High doses cause
cortical excitation, restlessness, disorientation, hallucinations and delirium
followed by respiratory depression and coma.
Majority
of the central actions are due to blockade of muscarinic receptors in the brain,
but some actions may have a different basis.
2. CVS
Heart The most prominent effect of atropine is to cause tachycardia. It is due to blockade of
M2 receptors on SA node through which vagal tone decreases HR.
Higher the existing vagal tone— more marked is the tachycardia (maximum in young
adults, less in children and elderly). On i.m./s.c. injection transient initial
bradycardia often occurs. Earlier believed to be due to stimulation of vagal
centre, it is now thought to be caused by blockade of muscarinic autoreceptors
(M1) on vagal nerve endings augmenting ACh release. This is
suggested by the finding that selective M1 antagonist pirenzepine is
equipotent to atropine in causing bradycardia as are atropine substitutes which
do not cross bloodbrain barrier. Atropine abbreviates refractory period of AV
node and facilitates AV conduction, especially if it has been depressed by high
vagal tone. PR interval is shortened.
BP Since cholinergic impulses are not involved in maintenance of vascular tone, atropine does
not have any consistent or marked effect on BP. Tachycardia and vasomotor centre
stimulation tend to raise BP, while histamine release and direct vasodilator
action (at high doses) tend to lower BP.
Atropine blocks
vasodepressor action of cholinergic agonists.
3. Eye
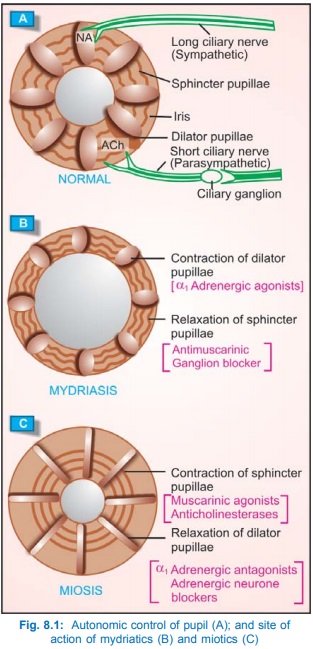
The autonomic control of iris muscles and the action of
mydriatics as well as miotics is illustrated in Fig. 8.1. Topical instillation
of atropine causes mydriasis, abolition of light reflex and cycloplegia lasting
7–10 days. This results in photophobia and blurring of near vision. The ciliary
muscles recover somewhat earlier than sphincter pupillae. The intraocular
tension tends to rise, especially in narrow angle glaucoma; conventional
systemic doses produce minor ocular effects.
4. Smooth Muscles
All visceral smooth muscles that receive parasympathetic motor
innervation are relaxed by atropine (M3 blockade). Tone and
amplitude of contractions of stomach and intestine are reduced; the passage of
chyme is slowed—constipation may occur, spasm may be relieved. However,
peristalsis is only incompletely suppressed because it is primarily regulated
by local reflexes and other neurotransmitters (5HT, enkephalin, etc.) as well
as hormones are involved. Enhanced motility due to injected cholinergic drugs
is more completely antagonised than that due to vagal stimulation.
Atropine causes bronchodilatation and reduces airway resistance, especially in COPD and asthma patients. Inflammatory mediators like histamine, PGs and kinins increase vagal activity in addition to their direct action on bronchial muscle and glands. Atropine attenuates their action by antagonizing the reflex vagal component.
Atropine has relaxant
action on ureter and urinary bladder; urinary retention can occur in older
males with prostatic hypertrophy. However, the same can be beneficial for
increasing bladder capacity and controlling detrusor hyperreflexia in neurogenic
bladder/enuresis. Relaxation of biliary tract is less marked and effect on
uterus is minimal.
5. Glands
Atropine markedly decreases sweat, salivary, tracheobronchial
and lacrimal secretion (M3 blockade). Skin and eyes become dry,
talking and swallowing may be difficult.
Atropine
decreases secretion of acid, pepsin and mucus in the stomach, but the primary
action is on volume of secretion so that pH of gastric contents may not be
elevated unless diluted by food. Since bicarbonate secretion is also reduced,
rise in pH of fasting gastric juice is only modest. Relatively higher doses are
needed and atropine is less efficacious than H2 blockers in reducing
acid secretion. Intestinal and pancreatic secretions are not significantly
reduced. Bile production is not under cholinergic control, so not affected.
6. Body Temperature
Rise in body temperature occurs at higher
doses. It is due to both inhibition of sweating as well as stimulation of temperature
regulating centre in the hypothalamus. Children are highly susceptible to
atropine fever.
7. Local Anaesthetic Atropine has a mild anaesthetic action on the cornea.
Atropine
has been found to enhance ACh (also NA) release from certain postganglionic
parasympathetic and sympathetic nerve endings, and thus produce paradoxical
responses. This is due to blockade of release inhibitory muscarinic
autoreceptors present on these nerve terminals.
The
sensitivity of different organs and tissues to atropine varies and can be
graded as—
Saliva, sweat,
bronchial secretion > eye, bronchial muscle, heart > smooth muscle of
intestine, bladder > gastric glands and smooth muscle.
The
above differences probably reflect the relative dependence of the function on
cholinergic tone vis a vis other
influences, and variation in synaptic gaps in different organs. The pattern of
relative activity is nearly the same for other atropine substitutes except pirenzepine which inhibits gastric secretion
at doses that have little effect on other secretions, heart and eye. This is
probably because atropine equally blocks M1, M2 and M3
receptors whereas pirenzepine is a selective M1 antagonist.
Atropine
more effectively blocks responses to exogenously administered cholinergic drugs
than those to parasympathetic nerve activity. This may be due to release of ACh
very close to the receptors by nerves
and involvement of cotransmitters.
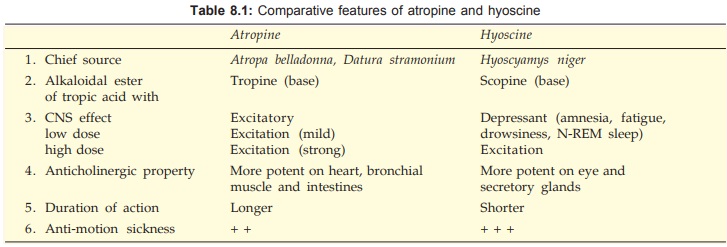
Hyoscine The other natural anticholinergic alkaloid differs from atropine in many
respects, these are tabulated in Table 8.1.
PHARMACOKINETICS
Atropine
and hyoscine are rapidly absorbed from g.i.t. Applied to eyes they freely
penetrate cornea. Passage across blood-brain barrier is somewhat restricted.
About 50% of atropine is metabolized in liver and rest is excreted unchanged in
urine. It has a t½ of 3–4 hours. Hyoscine is more completely metabolized and
has better blood-brain barrier penetration.
Atropine
sulfate: 0.6–2 mg i.m., i.v. (children 10 μg/kg), 1–2% topically
in eye. ATROPINE SULPHATE: 0.6 mg/ ml inj., 1% eye
drop/ointment; ATROSU LPH 1% eye drop, 5% eye oint.
Hyoscine
hydrobromide: 0.3–0.5 mg oral, i.m.; also as transdermal patch.
Combinations
of atropine with analgesics and antipyretics are banned in India.
Related Topics
