Pharmacokinetics of Inhalational Anaesthetics
| Home | | Pharmacology |Chapter: Essential pharmacology : General Anaesthetics
Inhalational anaesthetics are gases or vapours that diffuse rapidly across pulmonary alveoli and tissue barriers. The depth of anaesthesia depends on the potency of the agent (MAC is an index of potency) and its partial pressure (PP) in the brain, while induction and recovery depend on the rate of change of PP in the brain.
PHARMACOKINETICS OF INHALATIONAL ANAESTHETICS
Inhalational anaesthetics are gases or vapours that diffuse rapidly across pulmonary alveoli and tissue barriers. The depth of anaesthesia depends on the potency of the agent (MAC is an index of potency) and its partial pressure (PP) in the brain, while induction and recovery depend on the rate of change of PP in the brain. Transfer of the anaesthetic between lung and brain depends on a series of tension gradients which may be summarized as—
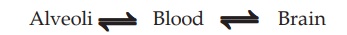
Factors affecting the PP of anaesthetic attained in the brain are—
1. PP of Anaesthetic In The Inspired Gas
This is proportional to its concentration in the inspired gas mixture. Higher the inspired tension more anaesthetic will be transferred to the blood. Thus, induction can be hastened by administering the GA at high concentration in the beginning.
2. Pulmonary Ventilation
It governs delivery of the GA to the alveoli. Hyperventilation will bring in more anaesthetic per minute and respiratory depression will have the opposite effect. Influence of minute volume on rate of induction is greatest in the case of agents which have high blood solubility because their PP in blood takes a long time to approach the PP in alveoli. However, it does not affect the terminal depth of anaesthesia attained with any concentration of a GA.
3. Alveolar Exchange
The GAs diffuse freely across alveoli, but if alveolar ventilation and perfusion are mismatched (as occurs in emphysema and other lung diseases) the attainment of equilibrium between alveoli and blood is delayed: well perfused alveoli may not be well ventilated—blood draining these alveoli carries less anaesthetic and dilutes the blood coming from well ventilated alveoli. Induction and recovery both are slowed.
4. Solubility Of Anaesthetic In Blood
This is the most important property determining induction and recovery. Large amount of an anaesthetic that is highly soluble in blood (ether) must dissolve before its PP is raised. The rise as well as fall of PP in blood and consequently induction as well as recovery are slow. Drugs with low blood solubility, e.g. N2O, sevoflurane, desflurane induce quickly.
Blood: gas partition coefficient (λ) given by the ratio of the concentration of the anaesthetic in blood to that in the gas phase at equilibrium is the index of solubility of the GA in blood.
5. Solubility Of Anaesthetic In Tissues
Relative solubility of the anaesthetic in blood and tissue determines its concentration in that tissue at equilibrium. Most of GAs are equally soluble in lean tissues as in blood, but more soluble in fatty tissue. Anaesthetics with higher lipid solubility (halothane) continue to enter adipose tissue for hours and also leave it slowly. The concentration of these agents is much higher in white matter than in grey matter.
6. Cerebral Blood Flow
Brain is a highly perfused organ; as such GAs are quickly delivered to it. This can be hastened by CO2 inhalation which causes cerebral vasodilatation—induction and recovery are accelerated. Carbon dioxide stimulates respiration and this also speeds up the transport.
Elimination
When anaesthetic administration is discontinued, gradients are reversed and the channel of absorption (pulmonary epithelium) becomes the channel of elimination. All inhaled anaesthetics are mainly eliminated through lungs. The same factors which govern induction also govern recovery. Anaesthetics, in general, continue to enter and persist for long periods in adipose tissue because of their high lipid solubility and low blood flow to fatty tissues. Muscles occupy an intermediate position between brain and adipose tissue. Most GAs are eliminated unchanged. Metabolism is significant only for halothane which is >20% metabolized in liver. Others are practically not metabolized. Recovery may be delayed after prolonged anaesthesia, especially in case of more lipidsoluble anaesthetics (halothane, isoflurane), because large quantities of the anaesthetic have entered the muscle and fat, from which it is released slowly into blood.
Second Gas Effect And Diffusion Hypoxia
In the initial part of induction, diffusion gradient from alveoli to blood is high and larger quantity of anaesthetic is entering blood. If the inhaled concentration of anaesthetic is high, substantial loss of alveolar gas volume will occur and the gas mixture will be sucked in, independent of ventilatory exchange—gas flow will be higher than tidal volume. This is significant only with N2O, since it is given at 70–80% concentration; though it has low solubility in blood, about 1 litre/min of N2O enters blood in the first few minutes—gas flow is 1 litre/min higher than minute volume. If another potent anaesthetic, e.g. halothane (1–2%) is being given at the same time, it also will be delivered to blood at a rate 1 litre/min higher than minute volume and induction will be faster—second gas effect.
The reverse occurs when N2O is discontinued after prolonged anaesthesia—N2O having low blood solubility rapidly diffuses into alveoli and dilutes the alveolar air—PP of oxygen in alveoli is reduced. The resulting hypoxia, called diffusion hypoxia, is not of much consequence if cardiopulmonary reserve is normal, but may be dangerous if it is low. This can be prevented by continuing 100% O 2 inhalation for a few minutes after discontinuing N2O, instead of straight away switching over to air. Diffusion hypoxia is not significant with other anaesthetics because they are administered at low concentrations (0.2–4%) and cannot dilute alveolar air by more than 1–2%.
Related Topics
