Parenteral Controlled Release Systems
| Home | | Biopharmaceutics and Pharmacokinetics |Chapter: Biopharmaceutics and Pharmacokinetics : Controlled Release Medication
One of the major advantages of parenteral controlled drug delivery systems is that the duration of action can be extended for days or months and sometimes upto a year.
PARENTERAL CONTROLLED RELEASE SYSTEMS
One of the major advantages of parenteral controlled drug delivery systems is that
the duration of action can be extended for days or months and sometimes upto a
year. The prime drawback is that,
once administered, the drug cannot be easily removed if an undesirable action
is precipitated or if the drug is no longer needed. Most of such systems are
administered by subcutaneous and intramuscular routes and few by intravenous
and intraperitoneal routes. Subcutaneous route is limited to well absorbed
water-soluble drugs like insulin and dose volume is limited to 0.5 to 1.5 ml.
Deep intramuscular route is suitable for polymeric systems or slightly soluble
drugs, the volume size restricted to 2 ml. Intravenous route is useful for
administration of liposomes, nanoparticles, erythrocytes and polypeptides. An
important criteria for this route is drug particle size. A disadvantage of i.v.
route is that the system may be taken up by the reticuloendothelial system but
the same can be put to use in targeting drugs to such a system. Intraperitoneal
route is important in targeting of antineoplastics into the lymphatic system.
The vehicle, polymers and other substances used in
the formulation of parenteral controlled-release dosage forms should be
sterile, pyrogen free, nonirritating, biocompatible and biodegradable into
nontoxic compounds within an appropriate time, preferably close to the duration
of drug action.
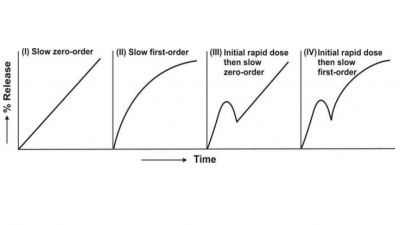
There are several approaches to achieve controlled
drug delivery via parenteral route, the release being controlled by
dissolution, diffusion, dissociation, partitioning or bioerosion. The systems
can be broadly classified as:
A. Injectables:
1. Solutions
2. Dispersions
3. Microspheres and Microcapsules
4. Nanoparticles and Niosomes
5. Liposomes
6. Resealed Erythrocytes
B. Implants
C. Infusion Devices:
1. Osmotic Pumps
2. Vapor Pressure Powered Pumps
3. Battery Powered Pumps
A. Injectables
1. Solutions
Both aqueous as well as oil solutions may be used
for controlled drug release. With aqueous
solutions (given intramuscularly), the drug release may be controlled in
three ways:
i. By increasing the viscosity of
vehicle by use of MC, CMC or PVP and thus, decreasing molecular diffusion and
localizing the injected drug.
ii. By forming a complex with macromolecules like
MC, CMC or PVP from which the drug dissociates at a controlled rate (only free
drug will get absorbed).
iii. By forming complexes that
control drug release not by dissociation but by reducing the solubility of
parent drug e.g. protamine zinc insulin and cyanocobalamin zinc tannate.
Oil solutions control the release by
partitioning the drug out of the oil in the
surrounding aqueous biofluids. Vegetable oils like arachis oil, cottonseed
oil, etc. are used for such a purpose. The method is applicable only to those
drugs which are oil soluble and have optimum partition coefficient.
2. Dispersions
Dispersed systems like emulsions and suspensions can
be administered by i.m., s.c. or i.v. routes. Among emulsions, the o/w systems have not been used successfully since
absorption of drug incorporated in the oil phase is rapid due to large
interfacial area and rapid partitioning. Similarly, few w/o emulsions of
water-soluble drugs have been tried for controlled-release. Multiple emulsions of w/o/w and o/w/o
types (more correctly, double emulsions)
are becoming popular since an additional reservoir is presented to the drug for partitioning which can effectively
retard its release rate (Fig. 14.13).
Control of drug release from suspensions is easier and predictable. Drug dissolution and
subsequent diffusion are the main rate controlling steps. Release of
water-soluble drugs can be retarded by presenting it as oil suspension and vice versa for oil soluble drugs.
Factors to be considered in the formulation of such a system include -
i. Solid content : should be
ideally in the range 0.5 to 5.0%
ii. Particle size : this factor is very important
since larger the particle size, slower the dissolution; however, larger
particles have their own disadvantages like causing irritation at the injection
site (size should therefore be below 10 microns), poor syringeability and
injectability and rapid sedimentation. The latter problem can be overcome by
use of viscosity builders which also retard drug diffusion.
Fig. 14.13 Multiple emulsions for parenteral controlled-release systems
Aqueous suspensions can be given by i.m. or s.c.
routes. Generally crystalline and stable
polymorphic forms of the drug are chosen rather than amorphous forms to delay
release. Solubility can be further reduced by salt or complex formation e.g.
crystalline zinc insulin shows more prolonged action than amorphous zinc insulin
complex. Oil suspensions, generally given i.m., prolong drug action much more in
comparison to oil solution and
aqueous suspension since drug release involves two rate- limiting steps viz.
dissolution of drug particles, and partitioning of the dissolved drug from oil
to the aqueous biofluids.
3. Microspheres and Microcapsules
Microspheres are free flowing powders
consisting of spherical particles of size ideally less than 125 microns that can be suspended in a suitable aqueous
vehicle and injected by an 18 or 20 number needle. Each particle is basically a
matrix of drug dispersed in a polymer from which release occurs by a
first-order process. The polymers used are biocompatible and biodegradable e.g.
polylactic acid, polylactide coglycolide, etc. Drug release is controlled by
dissolution/degradation of matrix. Small matrices release drug at a faster rate
and thus, by using particles of different sizes, various degrees of
controlled-release can be achieved. The system is ideally suited for controlled-release
of peptide/protein drugs such as LHRH which have short half-lives and otherwise
need to be injected once or more, daily, as conventional parenteral
formulations. In comparison to peptides, proteins are difficult to formulate
because of their higher molecular weight, lower solubility and the need to
preserve their conformational structure during manufacture.
In order to overcome uptake of intravenously
administered microspheres by the reticuloendothelial system and promote drug
targeting to tumors with good perfusion, magnetic
microspheres were developed. They are prepared from albumin and magnetite (Fe2O3)
and have a size of 1.0 micron to permit intravascular injection. The system is
infused into an artery that perfuses the target site and a magnet is placed
over the area to localize it in that region. A 100 times higher concentration
of doxorubicin was attained at the target site by such an approach with just
half the i.v. dose.
Microcapsules differ from microspheres in that
the drug is centrally located within the
polymeric shell of finite thickness and release may be controlled by
dissolution, diffusion or both. Quality microcapsules with thick walls
generally release their medicaments at a zero-order rate. Steroids, peptides
and antineoplastics have been successfully administered parenterally by use of
controlled-release microcapsules.
4. Nanoparticles and Niosomes
Nanoparticles are also called as nanospheres or nanocapsules depending upon whether the drug is in a polymer matrix or encapsulated in a shell. They
differ from microspheres in having submicron particles in the nanometer size
range—10 to 1000 nm. The polymers used are the usual biodegradable ones. The
main advantage of this system is that it can be stored for upto 1 year and can
be used for selective targeting via reticuloendothelial system to liver and to
cells that are active phagocytically.
Like nanoparticles, niosomes are inexpensive alternatives to liposomes. They are closed
vesicles formed in aqueous media from nonionic surfactants with or without the
presence of cholesterol or other lipids.
5. Liposomes
The term liposomes
(meaning lipid body) was derived on
the basis of names of subcellular particles like lysosome and ribosome. It is
defined as a spherule/vesicle of lipid bilayers enclosing an aqueous
compartment. The lipid most commonly used is phospholipid. Sphingolipids,
glycolipids and sterols have also been used to prepare liposomes. Their size
ranges from 25 to 5000 nm. Depending upon their structure, liposomes are
classified as:
i. MLV (multilamellar
vesicles) : These liposomes are made of series of concentric bilayers of
lipids enclosing a small internal volume.
ii. OLV (oligolamellar vesicles) : These are made of 2 to 10 bilayers of
lipids surrounding a large internal volume.
iii. ULV (unilamellar vesicles) : These are made of single bilayer of lipids.
They may be SUV (small unilamellar
vesicles) of size 20 to 40 nm, MUV (medium
unilamellar vesicles) of size 40 to
80 nm, LUV (large unilamellar vesicles)
of size 100 to 1000 nm or GUV (giant unilamellar vesicles) of size
greater than 1000 nm.
A large variety of drugs (antineoplastics,
antibiotics), peptides/proteins (including antibodies) and viruses and bacteria
can be incorporated into liposomes. Water-soluble drugs are trapped in the
aqueous compartment while lipophilic ones are incorporated in the lipid phase
of liposomes. Because of their availability in various sizes, ability to
incorporate both water as well as oil soluble drugs, their inertness and their
ability to protect labile drugs, liposomes are versatile carriers for
parenteral drug delivery systems. Intramuscularly and subcutaneously injected
liposomes deliver drug at a controlled rate while intravenous administration
selectively targets them to reticuloendothelial system and phagocytic cells. A
simple method by which liposomes can be produced involves drying an organic
solvent solution of lipids onto the wall of a flask/beaker followed by
hydration and dispersion of lipid by addition of buffer and mixing (Fig.
14.14).
Fig. 14.14 Production procedure for liposomes.
6. Resealed Erythrocytes
Drug loading in body’s own erythrocytes when used
to serve as controlled delivery systems have several advantages. They are fully biodegradable and biocompatible,
nonimmunogenic, can circulate intravascularly for days (act as circulatory drug
depots) and allow large amounts of drug to be carried. The drug need not be
chemically modified and is protected from immunological detection and enzymatic
inactivation. Drug loading can be done by immersing the cells in buffered
hypotonic solution of drug which causes them to rupture and release hemoglobin
and trap the medicament. On restoration of isotonicity and incubation at 37o
C, the cells reseal and are ready for use (Fig. 14.15).
Fig. 14.46 Drug loading in crythrocytes
Damaged erythrocytes are removed by the liver and
spleen. These organs can thus be specifically targeted by drug loaded
erythrocytes.
B. Implants
An ideal
implantable parenteral system should possess following properties—
1. Environmentally stable : should
not breakdown under the influence of heat, light, air and moisture.
2. Biostable : should not undergo
physicochemical degradation when in contact with biofluids (or drugs).
3. Biocompatible : should neither stimulate immune
responses (otherwise the implant will
be rejected) nor thrombosis and fibrosis formation.
4. Nontoxic and noncarcinogenic : its
degradation products or leached additives must be completely safe.
5. Should have a minimum surface
area, smooth texture and structural characteristics similar to the tissue in
which it is to be implanted to avoid irritation.
6. Should be removable
when required.
7. Should release the medicament at a constant
predetermined rate for a predetermined period of time.
Some of the important advantages of implants over injectable controlled-release
formulations are—
1. More effective and more
prolonged action (for over a year).
2. A significantly small dose is
sufficient.
A major disadvantage
of such systems is that a microsurgery is required for implantation of device.
Some devices can be easily implanted by use of a specially designed implanter
syringe. The devices are generally implanted subcutaneously or intramuscularly.
Subcutaneous tissue is an ideal location because of its easy access to
implantation, poor perfusion, slow drug absorption and low reactivity towards
foreign materials.
The drug may be dissolved, dispersed or embedded in
a matrix of polymers that control release by dissolution, diffusion or both,
bioerosion, biodegradation or an activation process such as osmosis or
hydrolysis. The system is generally prepared as implantable flexible/rigid
moulded or extruded rods, spherical pellets or compressed tablets. Polymers
used are silicone elastomers, polymethacrylates, polycaprolactone,
polylactide/glycolide, etc. Drugs generally presented in such systems are
steroids like contraceptives (megestrol acetate, norgestrone, etc.), morphine
antagonists like naltrexone for opiod-dependent addicts, etc.
C. Infusion Devices
These are also implantable devices but are
versatile in the sense that they are intrinsically powered to release the
medicament at a zero-order rate and the drug reservoir can be replenished from
time to time. Depending upon the mechanism by which these implantable pumps are
powered to release the contents, they are classified into following types:
1. Osmotic pressure activated drug delivery systems
2. Vapor pressure activated drug
delivery systems
3. Battery powered drug delivery
systems
1. Osmotic Pumps (Alzet)
These pumps are capsular in shape and made in a
variety of sizes. The device is shown in Fig. 14.16.
The pump is made of three concentric layers—the
innermost drug reservoir contained in a collapsible impermeable polyester bag
(which is open to the exterior via a single portal) followed by a sleeve of dry
osmotic energy source (sodium chloride) and the outermost rigid,
rate-controlling semipermeable membrane fabricated from substituted cellulosic
polymers. A rigid polymeric plug is used to form a leakproof seal between the
drug reservoir and the semipermeable housing. An additional component, the flow
modulator, comprising of a cap and a tube made of stainless steel is inserted
into the body of osmotic pump after filling. After implantation, water from the
surrounding tissue fluids is imbibed through the semipermeable membrane at a
controlled rate that dissolves the osmogen creating an osmotic pressure
differential across the membrane. The osmotic sleeve thus expands and since the
outer wall is rigid, it squeezes the inner flexible drug reservoir and drug
solution is expelled in a constant volume per unit time fashion. The drug
delivery continues until the reservoir is completely collapsed. Ionized drugs,
macromolecules, steroids and peptides (insulin) can be delivered by such a
device.
Rate Controlling Factors :
Porosity of semipermeable membrane
Osmotic pressure difference across the
membrane
Fig. 14.16 Cross section of osmotic pump
2. Vapour Pressure Powered Pump (Infusaid)
This device is based on the principle that at a
given temperature, a liquid in equilibrium with its vapour phase exerts a
constant pressure that is independent of enclosing volume. The device is shown
in Fig. 14.17.
The disc shaped device consists of two chambers—an
infusate chamber containing the drug solution which is separated by a freely
movable flexible bellow from the vapour chamber containing inexhaustible
vaporizable fluid such as fluorocarbons. After implantation, the volatile
liquid vaporizes at the body temperature and creates a vapour pressure that
compresses the bellows and expels the infusate through a series of flow
regulators at a constant rate. Insulin for diabetics and morphine for
terminally ill cancer patients have been successfully delivered by such a
device.
Fig. 14.17 Cross section of vapor pressure driven device
3. Battery Powered Pumps
Two types of battery powered implantable programmable
pumps used successfully to deliver insulin are—peristaltic pump and solenoid
driven reciprocating pump, both with electronic controls. The systems can be
programmed to deliver drug at desired rates. Their design is such that the drug
moves towards the exit and there is no backflow of the infusate.
Related Topics