Objectives and Use of Antimalarials
| Home | | Pharmacology |Chapter: Essential pharmacology : Antimalarial Drugs
The aims of using drugs in relation to malarial infection are:
OBJECTIVES AND USE OF
ANTIMALARIALS
The aims of using
drugs in relation to malarial infection are:
·
To prevent and treat clinical attack of
malaria.
·
To completely eradicate the parasite from the
patient’s body.
· To reduce the human reservoir of infection cut
down transmission to mosquito.
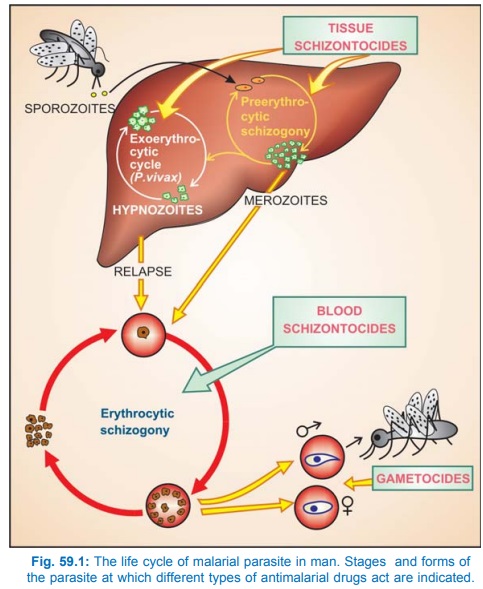
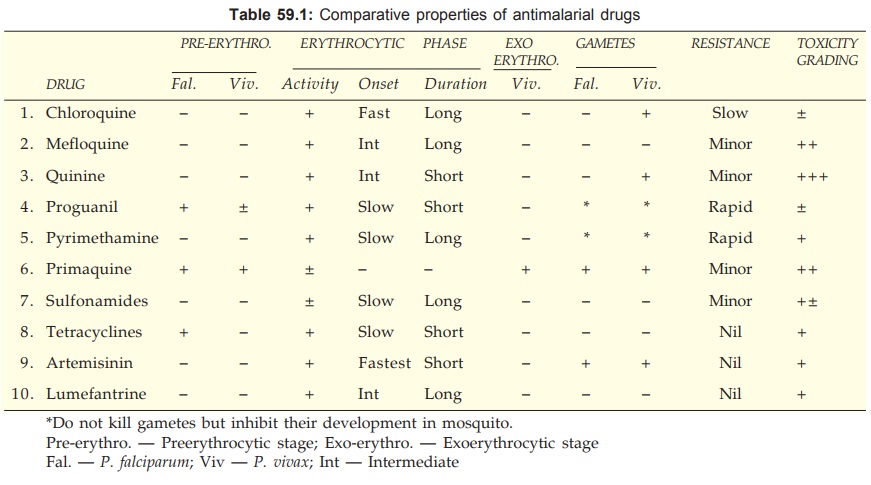
These are achieved by
attacking the parasite at its various stages of life cycle in the human host (see Fig. 59.1). Antimalarials that act
on erythrocytic schizogony are called erythrocytic
schizontocides, those that act on preerythrocytic as well as
exoerythrocytic (P. vivax) stages in
liver are called tissue schizontocides, while
those which kill gametocytes in blood
are called gametocides. Antimalarial
drugs exhibit considerable stage selectivity of action (see Table 59.1). Antimalarial therapy is given in the following
forms.
1. Causal Prophylaxis
The preerythrocytic phase (in liver), which is the cause of malarial infection and clinical
attacks, is the target for this purpose.
Proguanil is a causal
prophylactic, primarily for P.
falciparum, but is not employed routinely because it has to be given daily
and is not very effective against P.
vivax.
Primaquine is a causal prophylactic for all
species of malaria, but has not been used in mass programmes, because of its
toxic potential. Trials in Kenya and Irian Jaya have successfully used
primaquine 0.5 mg/kg daily against both P.
falciparum and P. vivax in
subjects with normal G6PD levels. The CDC (USA) recommends it only for subjects
who cannot take any other prophylactic drug.
2. Suppressive Prophylaxis
The schizontocides which suppress the
erythrocytic phase and thus attacks of malarial fever can be used as
prophylactics. Though the exoerythrocytic phase in case of vivax and other relapsing
malarias continues, clinical disease does not appear.
Chloroquine 300 mg (base*) or 5 mg/kg weekly.
In travellers, start one week before with a loading dose of 10 mg/kg and
continue till one month after return from endemic area. The last dose should be
25 mg/kg over 3 days along with primaquine 15 mg/day for 14 days. It should not
be given for > 3 yr for fear of cumulative toxicity.
Proguanil 200 mg daily
with chloroquine 300 mg weekly affords substantial protection against
moderately chloroquine-resistant P. falciparum, but less than that afforded
by mefloquine. This has been
successfully used in Africa. In India NVBDCP recommends it for visitors to
areas with chloroquine resistance.
Mefloquine 250 mg
weekly till 4 weeks after return from endemic area has been used for areas
where chloroquine-resistant P. falciparum
is prevalent. In India use of mefloquine for prophylaxis is not allowed among
residents, but may be used by travellers.
Doxycycline 100 mg
daily starting day before travel and taken till 4 weeks after return from
endemic area for chloroquine resistant P.
falciparum, is an alternative regimen
for individuals unable to take
mefloquine. It is contraindicated in pregnant women and children < 8 yr.
Chemoprophylaxis of
malaria should be limited to short-term use in special risk groups, such as —
nonimmune travellers, nonimmune persons living in endemic areas for fixed
periods (army units, labour forces) and pregnant women (falciparum malaria has
serious consequences in the pregnant). Start prophylaxis after 1st trimester
and continue till 1 month after delivery.
3. Clinical Cure
The erythrocytic schizontocides are used to
terminate an episode of malarial fever. The available drugs can be divided
into:
Fast-Acting High-Efficacy Drugs: Chloroquine, amodiaquine, quinine,
mefloquine, halofantrine, lumefantrine, atovaquone, artemisinin; they can be
used singly to treat attacks of malarial fever.
Slow-Acting Low-Efficacy Drugs: Proguanil, pyrimethamine, sulfonamides,
tetracyclines; they are used only in combination for clinical cure.
The faster acting
drugs are preferred, particularly in falciparum malaria where delay in
treatment may result in death even if the parasites are cleared from blood by
the drug. The exoerythrocytic phase of vivax and ovale persists which can cause
relapses subsequently without
reinfection. Thus, the above drugs are radical curatives for falciparum, but
not for relapsing malaria. Recrudescences
occur in falciparum infection if the blood is not totally cleared of the
parasites by the drug.
The drugs and regimens
used for uncomplicated falciparum and vivax malaria are detailed in the box.
Only oral drugs are used for uncomplicated malaria.
Treatment Of Uncomplicated Malaria
Vivax malaria
1. Chloroquine 600 mg (10 mg/kg) followed by
300 mg (5 mg/kg) after 8 hours and then for next 2 days (total 25 mg/kg over 3
days) + Primaquine 15 mg (0.25 mg/kg) daily × 14 days
In occasional case of
chloroquine resistance
2. Quinine 600 mg (10 mg/kg) 8
hourly × 7 days + Doxycycline 100 mg daily × 7 days + Primaquine (as above)
Chloroquine-sensitive Falciparum malaria
1. Chloroquine (as above) + Primaquine 45 mg (0.75
mg/kg) single dose (as gametocidal)
In case of intolerance
to chloroquine
2. Sulfadoxine 1500 mg
(25 mg/kg) + Pyrimethamine 75 mg (1.25 mg/kg) single dose + Primaquine 0.75
mg/kg single dose
Chloroquine-Resistant Falciparum malaria
1.* Artesunate 100 mg BD (4 mg/kg/day) × 3
days + Sulfadoxine# 1500 mg (25 mg/kg) + Pyrimethamine 75 mg (1.25 mg/kg)
single dose
or
2. Artesunate
100 mg BD (4 mg/kg/day) × 3 days + Mefloquine# 750 mg (15 mg/kg) on 2nd day and
500 mg (10 mg/kg) on 3rd day.
or
Artemether 80 mg + Lumefantrine 480 mg twice
daily × 3 days (child 25–35 kg BW ¾ dose; 15–25 kg BW ½ dose; 5–15 kg BW ¼ dose)
or
4.$ Quinine 600 mg (10 mg/kg) 8 hourly × 7
days + Doxycycline 100 mg daily × 7 days.
*First line ACT under NVBDCP
$Second line drug
under NVBDCP
#Sulfadoxine-pyrimethamine (S/P) alone and
mefloquine alone are also used, but should preferably be combined with
artesunate.
Relapses of vivax/ovale malaria are treated in
the same way as the primary attack because the parasite remains sensitive to
the drug. Recrudescence in falciparum malaria indicates resistant infection: should
be treated with an alternative drug as per local needs.
Severe And Complicated Falciparum malaria
This includes P.
falciparum infection attended by any one or more of—hyperparasitaemia,
hyperpyrexia, fluid and electrolyte imbalance, acidosis, hypoglycaemia,
prostration, cardiovascular collapse, jaundice, severe anaemia, spontaneous bleeding,
pulmonary edema, haemoglobinuria, black water fever, renal failure and cerebral
malaria. Parenteral (i.m./i.v.) drugs have to be used; oral drugs may be
substituted when the condition improves. Drugs and regimens employed are
detailed below.
Treatment Of Severe And Complicated Falciparum Malaria*
Artesunate: 2.4 mg/kg i.v. or
i.m., followed by 2.4 mg/kg after 12 and 24 hours, and then once daily for 7
days. Switchover to 3 day oral ACT inbetween whenever the patient can take and
tolerate oral medication.
or
Artemether: 3.2 mg/kg i.m. on the
1st day, followed by 1.6 mg/kg daily for 7 days. Switchover to 3 day oral ACT
inbetween whenever the patient is able to take oral medication.
or
Arteether: 3.2 mg/kg i.m. on the
1st day, followed by 1.6 mg/kg daily for the next 4 days. Switchover to 3 day
oral ACT inbetween whenever the patient is able to take oral medication.
or
Quinine diHCl: 20 mg/kg (loading
dose) diluted in 10 ml/kg 5% dextrose/dextrosesaline and infused i.v. over 4
hours, followed by 10 mg/kg (maintenance dose) i.v. infusion over 4 hours (in
adults) or 2 hours (in children) every 8 hours, untill patient can swallow.
Switchover to oral quinine 10 mg/kg 8 hourly to complete the 7 day course.
(Volume of fluid for i.v. infusion of quinine
should be reduced in patients with volume overload/pulmonary edema).
(If possible, oral quinine should be
substituted by 3 day oral ACT, or doxycycline 100 mg daily should be combined
with it).
(Chloroquine HCl i.v. to be used only if none
of the above is available and only in adults).
4. Radical Cure
Drugs which attack the
exoerythrocytic stage (hypnozoites) given together with a clinical curative achieve
total eradication of the parasite from the patient’s body. A radical curative
is needed in relapsing malaria, while in falciparum malaria — adequate
treatment of clinical attack leaves no parasite in the body (there is no
secondary exoerythrocytic tissue phase).
Drug of choice for
radical cure of vivax and ovale malaria is:
Primaquine 15 mg daily
for 14 days. A shorter course of 5 days used earlier by NAMP in India has been
found inadequate, and is no longer recommended. This treatment should be given
concurrently with or immediately after chloroquine/other schizontocide only to
individuals who test negative for G6PD deficiency.
There is no point in
antirelapse treatment in highly endemic areas, because chances of reinfection
would be high; a subsequent attack may be erroneously labelled as failure of
radical cure. Antirelapse treatment of vivax malaria should be restricted to:
· Areas with very low level of transmission
(where only sporadic cases occur).
·
Patients treated during an epidemic along with
effective vector control measures to cut down transmission.
5. Gametocidal
This refers to
elimination of the male and female
gametes of Plasmodia formed in the
patient’s blood. Gametocidal action is of no benefit to the patient being
treated, but will reduce the transmission to mosquito.
Primaquine and artemisinins are gametocidal to
all species of Plasmodia, while
chloroquine and quinine are active against vivax but not falciparum gametes.
Gametes exposesd to proguanil or pyrimethamine fail to carry on the life cyle
normally in the mosquito. Adequate control of clinical attacks will reduce
formation of gametes.
A single 45 mg (0.75 mg/kg) dose of primaquine
is employed immediately after clinical cure of falciparum malaria to kill the
gametes and cut down transmission to mosquito. This is not necessary when an
artemisinin is used for clinical cure.
