Metoclopramide - Prokinetic Drug
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs For Emesis, Reflux And Digestive Disorders
Metoclopramide is chemically related to procainamide, but has no pharmacological similarity with it. Introduced in early 1970s as a ‘gastric hurrying’ agent, it is now a widely used antiemetic.
METOCLOPRAMIDE
Metoclopramide is chemically related to procainamide, but has no pharmacological similarity with it. Introduced in early 1970s as a ‘gastric hurrying’ agent, it is now a widely used antiemetic.
Actions
GIT: It has more prominent effect on upper g.i.t.; increases gastric peristalsis while relaxing the pylorus and the first part of duodenum → speeds gastric emptying, especially if it was slow. This action is independent of vagal innervation, but is more prominent when vagus is intact. Lower esophageal sphincter (LES) tone is increased and gastroesophageal reflux is opposed. It also increases intestinal peristalsis to some extent, but has no significant action on colonic motility and gastric secretion.
CNS: Metoclopramide is an effective antiemetic; acting on the CTZ, blocks apomorphine induced vomiting. The gastro-kinetic action may contribute to the antiemetic effect. However, it has no chlorpromazine (CPZ) like neuroleptic action, though it does share the extrapyramidal and prolactin secretion augmenting action of CPZ.
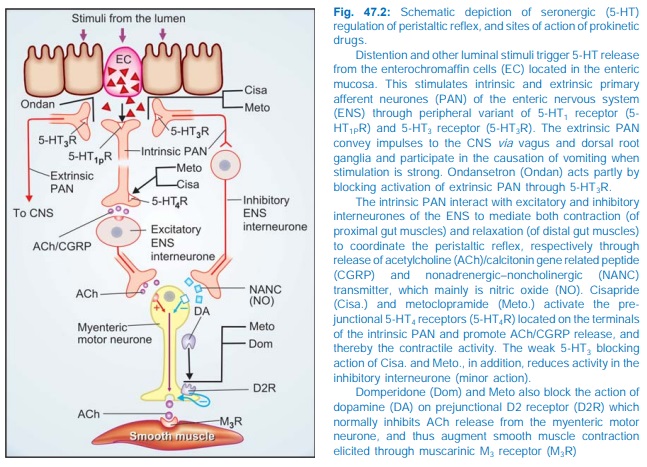
Mechanism Of Action: Metoclopramide acts through both dopaminergic and serotonergic receptors (see Fig. 47.2)
D2 Antagonism
Dopamine (acting through D2 receptors) is an inhibitory transmitter in the g.i.t.— normally acts to delay gastric emptying when food is present in stomach. It also appears to cause gastric dilatation and LES relaxation attending nausea and vomiting. Metoclopramide blocks D2 receptors and has an opposite effect— hastening gastric emptying and enhancing LES tone by augmenting ACh release. However, clinically this action is secondary to that exerted through 5HT4 receptors.
The central antidopaminergic (D2) action of metoclopramide on CTZ is clearly responsible for its antiemetic property. Other manifestations of D2 blockade are antagonism of apomorphine induced vomiting, CPZ like extrapyramidal effects and hyper-prolactinaemia.
5HT4 Agonism
Metoclopramide acts in the g.i.t. to enhance ACh release from myenteric motor neurones. This results from 5HT4 receptor activation on primary afferent neurones (PAN) of the ENS via excitatory inter-neurones (Fig. 47.2). The gastric hurrying and LES tonic effects are mainly due to this action which is synergised by bethanechol and attenuated by atropine.
5HT3 Antagonism
At high concentrations metoclopramide can block 5HT3 receptors present on inhibitory myenteric inter-neurones and in NTS/CTZ. The peripheral action can augment ACh release in the gut, but appears to be minor. The central anti 5HT3 action appears to be significant only when large doses are used to control chemotherapy induced vomiting.
Pharmacokinetics
Metoclopramide is rapidly absorbed orally, enters brain, crosses placenta and is secreted in milk. It is partly conjugated in liver and excreted in urine within 24 hours; t½ is 3–6 hours. Orally it acts in ½–1 hr, but within 10 min after i.m. and 2 min after i.v. injection. Action lasts for 4–6 hours.
Interactions
It hastens the absorption of many drugs, e.g. aspirin, diazepam, etc. by facilitating gastric emptying. It reduces the extent of absorption of digoxin by allowing less time for it. Bioavailability of cimetidine is also reduced.
By blocking DA receptors in basal ganglia, it abolishes the therapeutic effect of levodopa.
Adverse Effects
Metoclopramide is generally well tolerated.
Sedation, dizziness, loose stools, muscle dystonias (especially in children) are the main side effects.
Long-term use can cause parkinsonism, galactorrhoea and gynaecomastia.
It should not be used to augment lactation. Though the amount secreted in milk is small, but suckling infant may develop loose motions, dystonia, myoclonus.
Dose: 10 mg (children 0.2–0.5 mg/kg) TDS oral or i.m. For chemotherapy induced vomiting 0.3–1.0 mg/kg slow i.v./i.m. PERINORM, MAXERON, REGLAN, SIGMET, 10 mg tab; 5 mg/5 ml syr; 10 mg/2 ml inj.; 50 mg/ 10 ml inj.
Uses
1. Antiemetic: Metoclopramide is an effective and popular drug for many types of vomiting— postoperative, drug induced, disease associated (especially migraine), radiation sickness, etc, but is less effective in motion sickness. Though ondansetron is preferred, metoclopramide continues to be used for prophylaxis and treatment of vomiting induced by highly emetic anticancer drugs (cisplatin, etc.). A higher dose (1 mg/kg i.v.) is often needed, but is effective when phenothiazines and antihistamines do not work. Promethazine, diphenhydramine, diazepam or lorazepam injected i.v. along with metoclopramide supplement its antiemetic action and reduce the attending dystonic reactions. Dexamethasone i.v. also augments the efficacy of metoclopramide.
Though no teratogenic effects have been reported, metoclopramide should be used for morning sickness only when not controlled by other measures.
2. Gastrokinetic: to accelerate gastric emptying:
· When emergency general anaesthesia has to be given and the patient has taken food less than 4 hours before.
· To relieve post-vagotomy or diabetes associated gastric stasis.
· To facilitate duodenal intubation. Clinical efficacy is moderate.
3. Dyspepsia and other functional g.i. disorders. Metoclopramide may succede in stopping persistent hiccups.
4. Gastroesophageal Reflux Disease (GERD) Metoclopramide may afford symptomatic relief in milder cases of GERD, but is much less effective than PPIs/H2 blockers. It does not aid healing of esophagitis. It may be used as adjuvant to acid suppressive therapy, but additional benefit is uncertain.
