Local Anaesthetics
| Home | | Pharmacology |Chapter: Essential pharmacology : Local Anaesthetics
Local anaesthetics (LAs) are drugs which upon topical application or local injection cause reversible loss of sensory perception, especially of pain, in a restricted area of the body.
LOCAL ANAESTHETICS
Local anaesthetics (LAs) are drugs which upon topical
application or local injection cause reversible loss of sensory perception,
especially of pain, in a restricted area of the body. They block generation and
conduction of nerve impulse at all parts of the neurone where they come in
contact, without causing any structural damage. Thus, not only sensory but also
motor impulses are interrupted when a LA is applied to a mixed nerve, resulting
in muscular paralysis and loss of autonomic control as well.
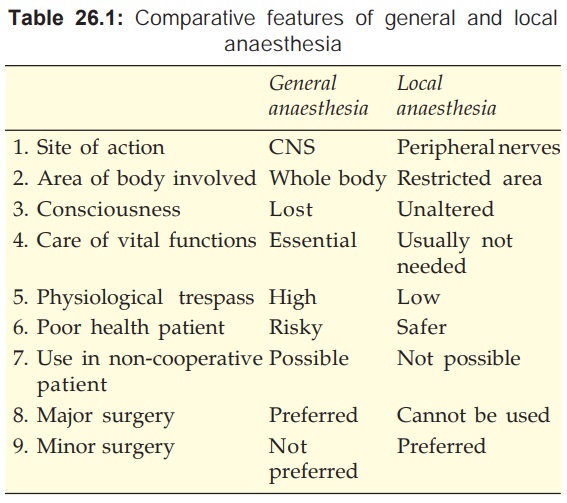
Important differences between general and local anaesthesia are
tabulated in Table 26.1.
Classification
Injectable
Anaesthetic
Low
potency, short duration
Procaine
Chloroprocaine
Intermediate
potency and duration
Lidocaine (Lignocaine)
Prilocaine
High
potency, long duration
Tetracaine (Amethocaine)
Bupivacaine
Ropivacaine
Dibucaine (Cinchocaine)
Surface
anaesthetic
Soluble Insoluble
Cocaine Benzocaine
Lidocaine Butylaminobenzoate
Tetracaine (Butamben)
Benoxinate Oxethazaine
Mepivacaine, Etidocaine,
Articaine, Dyclonine, Proparacaine are other local anaesthetics, occasionally
used in some countries.
Some other drugs, e.g.
propranolol, chlorpromazine, H1 antihistaminics, quinine have
significant LA activity, but are not used for this purpose because of local
irritancy or other prominent systemic activity. Local anaesthesia can be
produced by cooling as well, e.g. application of ice, CO2 snow,
ethylchloride spray.
Chemistry
The clinically useful LAs are weak bases with amphiphilic property.
A hydrophilic secondary or tertiary amine on one side and a lipophilic aromatic
residue on the other are joined by an alkyl chain through an ester or amide linkage.
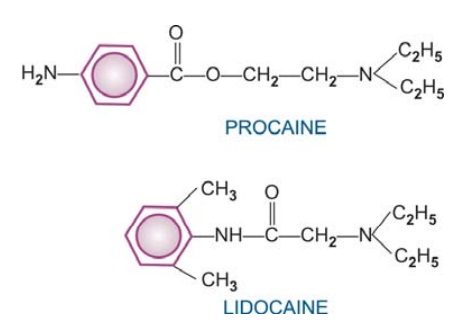
Ester-linked LAs Cocaine, procaine, chloroprocaine, tetracaine,
benzocaine.
Amide-linked LAs Lidocaine,
bupivacaine, dibucaine, prilocaine, ropivacaine.
Features of amide LAs compared to ester LAs
ü Produce more intense
and longer lasting anaesthesia
ü Bind to α1 acid glycoprotein in
plasma
ü Not hydrolysed by
plasma esterases
ü Rarely cause hypersensitivity
reactions; no cross sensitivity with ester LAs
Because of their short duration, less intense analgesia and
higher risk of hypersensitivity, the ester-linked LAs are rarely used for
infiltration or nerve block, but are still used topically on mucous membranes.
Mechanism Of Action
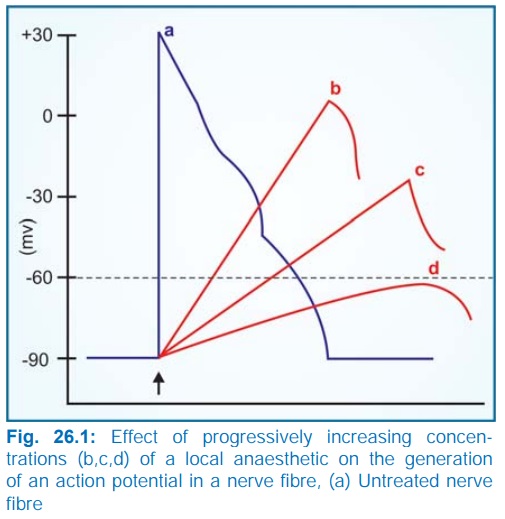
The LAs block nerve
conduction by decreasing the entry of Na+ ions during upstroke of action
potential (AP). As the concentration of the LA is increased, the rate of rise
of AP and maximum depolarization
decreases (Fig. 26.1) causing slowing of conduction. Finally, local
depolarization fails to reach the threshold potential and conduction block
ensues.
The LAs interact with
a receptor situated within the voltage sensitive Na+ channel and raise the
threshold of channel opening: Na+ permeability fails to increase in response to
an impulse or stimulus. Impulse conduction is interrupted when the Na+ channels
over a critical length of the fibre (2–3 nodes of Ranvier in case of myelinated
fibres) are blocked. The details are explained in Fig. 26.2. At physiological
pH, the LA molecule is partly ionized. The equilibrium between the unionized
base form (B) and the ionized cationic form (BH+) depends on the pKa of the LA.
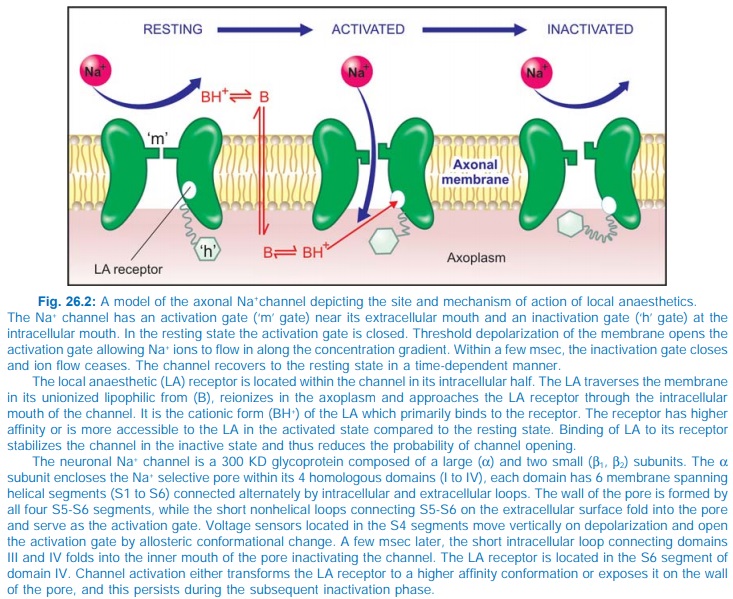
The predominant active
species (cationic form of LA) is able to approach its receptor only when the
channel is open at the inner face and it binds more avidly to the inactive
state of the channel, prolonging the inactive state. The channel takes longer
to recover → refractory period of
the fibre is increased. A resting nerve is rather resistant to blockade, and
blockade develops rapidly when the nerve is stimulated repeatedly. Degree of
blockade is frequency dependent: greater blockade at higher frequency of stimulation.
Moreover, exposure to higher concentration of Ca2+ reduces inactivation of Na+
channels and lessens the degree of block. Blockade of conduction by LA is not
due to hyperpolarization; in fact, resting membrane potential is unaltered
because K+ channels are blocked only at higher concentrations of LA.
The onset time of
blockade is related primarily to the pKa of the LA. Those with lower pKa
(7.6–7.8), e.g. lidocaine, mepivacaine are fast acting, because 30–40% LA is in
the undissociated base form at pH 7.4 and it is this form which penetrates the
axon. Procaine, tetracaine, bupivacaine have higher pKa (8.1–8.9), only 15% or
less is unionized at pH 7.4; these are slow acting. Chloroprocaine is an exception,
having rapid onset despite high pKa (9.1).
Local Actions
The clinically used LAs
have no/minimal local irritant action and block sensory nerve endings, nerve
trunks, neuromuscular junction, ganglionic synapse and receptors (nonselectively),
i.e. structures which function through increased Na+ permeability. They also
reduce release of acetylcholine from motor nerve endings. Injected around a
mixed nerve they cause anaesthesia of skin and paralysis of the voluntary
muscle supplied by that nerve.
Sensory and motor
fibres are inherently equally sensitive. The sensitivity is determined by
diameter of the fibres as well as by fibre type. Diameter remaining the same,
myelinated nerves are blocked earlier than nonmyelinated. In general, smaller
fibres are more sensitive than larger fibres. Fibres differ in the critical
length of the axon that must be exposed to the LA for effective blockade.
Smaller fibres tend to have shorter critical lengths, because in them voltage
changes propagate passively for shorter distances. Also, more slender axons
have shorter internodal distances and LAs easily enter the axon at the nodes of
Ranvier. The density of Na+ channel is much higher at these nodes. Moreover,
frequency dependence of blockade makes smaller sensory fibres more vulnerable
since they generate high frequency longer lasting action potentials than the
motor fibres.
Autonomic fibres are
generally more susceptible than somatic fibres. Among the somatic afferents
order of blockade is: pain—temperature sense—touch—deep pressure sense. Since
pain is generally carried by smaller diameter fibres than those carrying other
sensations or motor impulses, pain in the first modality to be affected.
Applied to the tongue, bitter taste is lost first followed by sweet and sour, and
salty taste last of all.
In general, fibres that
are more susceptible to LA are the first to be blocked and the last to recover.
Also, location of the fibre within a nerve trunk determines the latency,
duration and often the depth of local anaesthesia. Nerve sheaths restrict
diffusion of the LA into the nerve trunk so that fibres in the outer layers are
blocked earlier than the inner or core fibres. As a result, the more proximal
areas supplied by a nerve are affected earlier because axons supplying them are
located more peripherally in the nerve than those supplying distal areas. The differential
arrangement of various types of sensory and motor fibres in a mixed nerve may
partly account for the differential blockade. Motor fibres are usually present
circumferentially; may
be blocked earlier than the sensory fibres in the core of the nerve.
The LA often fails to
afford adequate pain control in inflamed tissues (like infected tooth). The
likely reasons are:
1. Inflammation lowers pH
of the tissue—greater fraction of the LA is in the ionized form hindering
diffusion into the axolemma.
2. Blood flow to the
inflamed area is increased— the LA is removed more rapidly from the site.
3. Effectiveness of Adr
injected with the LA is reduced at the inflamed site.
4. Inflammatory products
may oppose LA action.
Addition of a vasoconstrictor,
e.g. adrenaline (1:50,000 to 1:200,000):
·
Prolongs duration of action of LAs by
decreasing their rate of removal from the local site into the circulation.
·
Enhances the intensity of nerve block.
·
Reduces systemic toxicity of LAs: rate of absorption
is reduced and metabolism keeps the plasma concentration lower.
·
Makes the injection more painful.
·
Provides a more bloodless field for surgery.
·
Increases the chances of subsequent local
tissue edema and necrosis as well as delays wound healing by reducing oxygen
supply and enhancing oxygen consumption in the affected area.
·
May raise BP and promote arrhythmia in
susceptible individuals.
Systemic Actions
Any LA injected or
applied locally is ultimately absorbed and can produce systemic effects depending
on the concentration attained in the plasma and tissues.
C.N.S.
All LAs are capable of
producing a sequence of stimulation followed by depression. Cocaine is a powerful CNS stimulant
causing in sequence euphoria—excitement—mental confusion—restlessness—tremor
and twitching of muscles— convulsions—unconsciousness—respiratory
depression—death, in a dose-dependent manner.
Procaine and other synthetic LAs are much less potent in this regard. At safe
clinical doses, they produce little apparent CNS effects. Higher dose or
accidental i.v. injection produces CNS stimulation followed by depression.
Lidocaine, on the contrary, can initially cause drowsiness and lethargy, but higher
doses produce excitation followed by depression like others.
The basic action of all LAs is neuronal inhibition; the apparent
stimulation seen initially is due to inhibition of inhibitory neurones. At high
doses, all neurones are inhibited and flattening of waves in EEG is seen.
C.V.S.
Heart LAs are cardiac depressants, but no significant effects are observed at
conventional doses. At high doses or on inadvertent i.v. injection, they
decrease automaticity, excitability, contractility, conductivity and increase
effective refractory period (ERP). They have a quinidine like antiarrhythmic
action. Procaine is not used as
antiarrhythmic because of short duration of action and propensity to cause CNS
effects, but its amide derivative procainamide
is a classical antiarrhythmic. At high plasma concentrations
electrophysiological properties of heart may be markedly altered, QTc interval
is prolonged and LAs can themselves induce cardiac arrhythmias. Bupivacaine is relatively more
cardiotoxic and has produced
ventricular tachycardia or fibrillation. Lidocaine
has little effect on contractility and conductivity; it abbreviates ERP and is
used as an antiarrhythmic (see Ch.
No. 38).
Blood vessels LAs tend to produce
fall in BP. This is primarily due
to sympathetic blockade, but high concentrations, as obtained locally at the
site of injection, do cause direct relaxation of arteriolar smooth muscle.
Bupivacaine is more vasodilatory than lidocaine, while prilocaine is the least
vasodilatory. Toxic doses of LAs
produce cardiovascular
collapse. Cocaine has sympathomimetic
property; causes local vasoconstriction, marked rise in BP and tachycardia.
Procaine and related
drugs have weak anticholinergic, antihistaminic, ganglion blocking,
neuromuscular blocking and smooth muscle relaxant properties, but these are
clinically insignificant.
Pharmacokinetics
Soluble surface anaesthetics
(lidocaine, tetracaine) are rapidly absorbed from mucous membranes and abraded
areas, but absorption from intact skin is poor. Procaine does not significantly
penetrate mucous membranes. Rate of absorption depends on the blood flow to the
area of application or injection. The absorbed LA being lipophilic is widely
distributed; rapidly enters highly perfused brain, heart, liver, and kidney,
followed by muscle and other viscera.
Procaine is negligibly
bound to plasma proteins, but amide LAs are bound to plasma α1 acid glycoprotein.
LAs are rapidly but temporarily bound to tissues, especially nerves, at the
site of injection. Ester-linked LAs (procaine, etc.) are rapidly hydrolysed by
plasma pseudocholinesterase and the remaining by esterases in the liver. Amide-linked
LAs ( lidocaine, etc.) are degraded only in the liver microsomes by
dealkylation and hydrolysis. Metabolism of lidocaine is hepatic bloodflow
dependent. The maximal safe dose of LAs is lower in patients with hepatic disease
and in the elderly who have decreased liver function.
After oral ingestion
both procaine and lidocaine have high first pass metabolism in the liver. Thus,
they are not active orally for antiarrhythmic purposes.
Adverse Effects
a) Systemic toxicity on rapid i.v. injection is
related to the intrinsic anaesthetic potency of the LA. However, toxicity after
topical application or regional injection is influenced by relative rates of absorption
and metabolism, those rapidly absorbed but slowly metabolized are more toxic.
b) CNS effects are lightheadedness,
dizziness, auditory and visual disturbances, mental confusion, disorientation,
shivering, twitchings, involuntary movements, finally convulsions and
respiratory arrest. This can be prevented and treated by diazepam.
c)
Cardiovascular toxicity of LAs is manifested
as bradycardia, hypotension, cardiac arrhythmias and vascular collapse.
d) Injection of LAs may
be painful, but local tissue toxicity of LAs is low. However, wound healing may
be sometimes delayed. Addition of vasoconstrictors enhances the local tissue
damage; rarely necrosis results. Vasoconstrictors should not be added for ring
block of hands, feet, fingers, toes, penis and in pinna. Bupivacaine has the
highest local tissue irritancy.
e)
Hypersensitivity reactions like rashes, angioedema,
dermatitis, contact sensitization, asthma and rarely anaphylaxis occur. These
are more common with esterlinked LAs, but rare with lidocaine or its congeners.
Cross reactivity is frequent among ester compounds, but not with amidelinked
LAs.
Precautions And Interactions
a) Before injecting the
LA, aspirate lightly to avoid intravascular injection.
b) Inject the LA slowly
and take care not to exceed the maximum safe dose, especially in children.
c) Propranolol (probably
other β blockers also) may
reduce metabolism of lidocaine and other amide LAs by reducing hepatic blood
flow.
d) Vasoconstrictor
(adrenaline) containing LA should be avoided for patients with ischaemic heart
disease, cardiac arrhythmia, thyrotoxicosis, uncontrolled hypertension, and
those receiving β blockers (rise in BP due to unopposed α action) or tricyclic antidepressants
(uptake blockade of Adr).
Individual Compounds
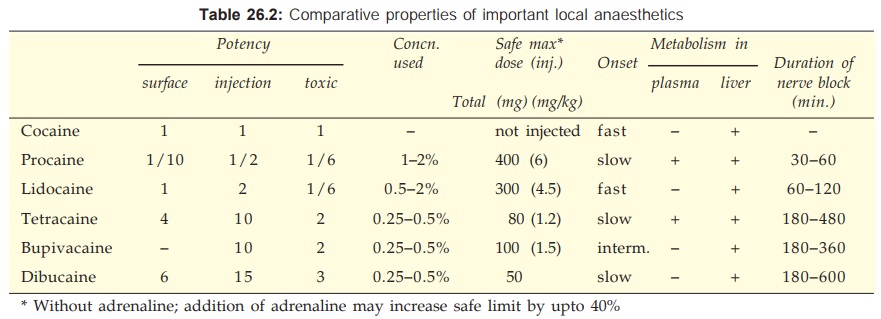
Important properties of local anaesthetics are compared in Table
26.2.
Cocaine
It is a natural alkaloid from leaves of Erythroxylon coca, a south American
plant growing on the foothills of the
Andes. The natives of Peru and Bolivia habitually chew these leaves. Cocaine is
a good surface anaesthetic and is rapidly absorbed from buccal mucous membrane.
It was first used for ocular anaesthesia in 1884. Cocaine should never be
injected; it is a protoplasmic poison and causes tissue necrosis. Cocaine
produces prominent CNS stimulation with marked effect on mood and behaviour. It
induces a sense of wellbeing, delays fatigue and increases power of endurance.
In susceptible individuals it produces a state referred to as ‘high’ leadting
to strong psychological but little physical dependence. Cocaine is unique among
drugs of abuse in not producing significant tolerance on repeated use;
sometimes reverse tolerance is seen (behavioural effects are experienced at lower
doses).
Cocaine also stimulates vagal centre→bradycardia; vasomotor
centre→rise in BP; vomiting
centre→nausea and vomiting;
temperature regulating centre→pyrexia (also due to increased heat production
as a result of enhanced muscular activity).
In the periphery, it
blocks uptake of NA and Adr into adrenergic nerve endings, resulting in higher
concentration of the transmitter around the receptors→ sympathomimetic
effect, potentiation of directly acting sympathomimetics and suppression of
indirectly acting sympathomimetics. Local vasoconstriction, tachycardia, rise
in BP and mydriasis are the reflection of its sympathomimetic action.
The only indication for cocaine is in ocular anaesthesia.
However, it causes constriction of conjunctival vessels, clouding and rarely
sloughing of cornea (due to drying and local tissue toxicity). Its use,
therefore, is not warranted.
Procaine
It is the first synthetic local anaesthetic introduced in 1905. Its popularity declined
after the introduction of lidocaine: practically not used now. It is not a surface
anaesthetic.
Procaine forms poorly
soluble salt with benzyl penicillin; procaine
penicillin injected i.m. acts for 24 hours due to slow absorption from the
site of injection.
Lidocaine (Lignocaine)
Introduced in 1948, it is currently the most widely used LA. It is a
versatile LA, good both for surface application as well as injection and is
available in a variety of forms. Injected around a nerve it blocks conduction
within 3 min, whereas procaine may take 15 min; also anaesthesia is more
intense and longer lasting. Vasodilatation occurs in the injected area. It is used
for surface application, infiltration, nerve block, epidural, spinal and
intravenous regional block anaesthesia. Cross sensitivity with ester LAs is not
seen. In contrast to other LAs, early central effects of lidocaine are
drowsiness, mental clouding, altered taste and tinnitus. Overdose causes muscle
twitching, convulsions, cardiac arrhythmias, fall in BP, coma and respiratory
arrest like other LAs. Lidocaine is a popular antiarrhythmic (see Ch. No. 38)
XYLOCAINE, GESICAIN 4%
topical solution, 2% jelly, 2% viscous, 5% ointment, 1% and 2% injection (with
or without adrenaline), 5% heavy (for spinal anaesthesia); 100 mg/ml spray (10
mg per actuation).
Prilocaine
It is similar to lidocaine
but does not cause vasodilatation at the
site of infiltration and has lower CNS toxicity due to larger volume of
distribution. One of its metabolites has potential to cause methaemoglobinaemia.
It has been used mainly for infiltration, nerve block and intravenous regional
anaesthesia.
Eutectic lidocaine/prilocaine
This is a unique preparation which can anaesthetise intact skin
after surface application. Eutectic mixture refers to lowering of melting point
of two solids when they are mixed. This happens when lidocaine and prilocaine
are mixed in equal proportion at 25°C. The resulting oil is emulsified into
water to form a cream that is applied under occlusive dressing for 1 hr before
i.v. cannulation, split skin graft harvesting and other superficial procedures.
Anaesthesia up to a depth of 5 mm lasts for 1–2 hr after removal. It has been
used as an alternative to lidocaine infiltration.
PRILOX 5% cream.
Tetracaine (Amethocaine)
A highly lipidsoluble
PABA ester, more potent and more toxic due to slow hydrolysis by plasma
pseudocholinesterase. It is both surface and conduction block anaesthetic, but
its use is restricted to topical application to the eye, nose, throat,
tracheobronchial tree and rarely for spinal or caudal anaesthesia of long
duration. Though it is slow acting, absorption from tracheobronchial spray is
very fast and blood concentrations approach those attained after i.v.
injection.
ANETHANE powder for
solution, 1% ointment.
Bupivacaine
A potent and long-acting amide-linked LA: used for infiltration,
nerve block, epidural and spinal anaesthesia of long duration. A 0.25–0.5%
solution injected epidurally produces adequate analgesia without significant
motor blockade. As a result, it has become very popular in obstetrics (mother
can actively cooperate in vaginal delivery) and for postoperative pain relief
by continuous epidural infusion. It has high lipidsolubility; distributes more
in tissues than in blood after spinal/epidural injection—less likely to reach the
foetus (when used during labour) to produce neonatal depression. Bupivacaine is
more prone to prolong QTc interval and induce ventricular tachycardia or
cardiac depression—should not be used for intravenous regional analgesia.
Epidural anaesthesia with 0.75% bupivacaine during labour has caused few fatalities
due to cardiac arrest; use of this concentration is contraindicated.
MARCAIN 0.5%, 1%
(hyperbaric for spinal anaesthesia).
SENSORCAINE 0.25%,
0.5% inj, 0.5% heavy inj.
The S(–) enantiomer Levobupivacaine is equally potent but
less cardiotoxic and less prone to cause seizures (after in-advertant
intravascular injection) than recemic bupivacaine. It has been introduced in
some countries as a single enantiomer preparation.
Ropivacaine
A newer bupivacaine
congener, equally long acting but less
cardiotoxic. It blocks Aδ and C fibres (involved in pain transmission)
more completely than Aβ fibres which control motor function. Though
equi-effective concentrations of ropivacaine are higher than those of bupivacaine,
a greater degree of separation between sensory and motor block has been
obtained with epidural ropivacaine. Continuous epidural ropivacaine is being
used for relief of postoperative and labour pain. It can also be employed for
nerve blocks.
Dibucaine (Cinchocaine)
It is the most potent,
most toxic and longest acting
LA. It is used as a surface anaesthetic on less delicate mucous membranes (anal
canal). Use for spinal anaesthesia of long duration has declined after the
availability of bupivacaine.
NUPERCAINE 0.5% inj., NUPERCAINAL 1% ointment, in OTOGESIC 1%
ear drops.
Benoxinate
It is a good surface anaesthetic for the eye; has
little irritancy. A 0.4% solution rapidly produces corneal anaesthesia
sufficient for tonometry without causing mydriasis or corneal damage.
BENDZON 0.4% eyedrops.
Benzocaine and Butylaminobenzoate
(Butamben)
Because of very low aqueous solubility, these LAs are not significantly absorbed from
mucous membranes or abraded skin. They produce long lasting anaesthesia without
systemic toxicity. They are used as lozenges for stomatitis, sore throat; as
dusting powder/ointment on wounds/ulcerated surfaces and as suppository for
anorectal lesions. Both are PABA derivative— can antagonize sulfonamides
locally.
PROCTOSEDYLM: Butylaminobenzoate 1% oint with framycetin and hydrocortisone acetate:
for piles.
PROCTOQUINOL 5%
ointment of benzocaine.
Oxethazaine
A potent topical
anaesthetic, unique in ionizing to a very
small extent even at low pH values. It is, therefore, effective in
anaesthetising gastric mucosa despite acidity of the medium. Swallowed along
with antacids it affords symptomatic relief in gastritis, drug induced gastric
irritation, gastroesophageal reflux and heartburn of pregnancy. Doses exceeding
100 mg/day may produce dizziness and drowsiness.
MUCAINE 0.2% in
alumina gel + magnesium hydroxide suspension; 5–10 ml orally.
TRICAINEMPS:
Oxethazaine 10 mg with methyl polysiloxane 125 mg, alum. hydroxide gel 300 mg,
mag. hydroxide 150 mg per 5 ml gel.
Uses And Techniques Of Local Anaesthesia
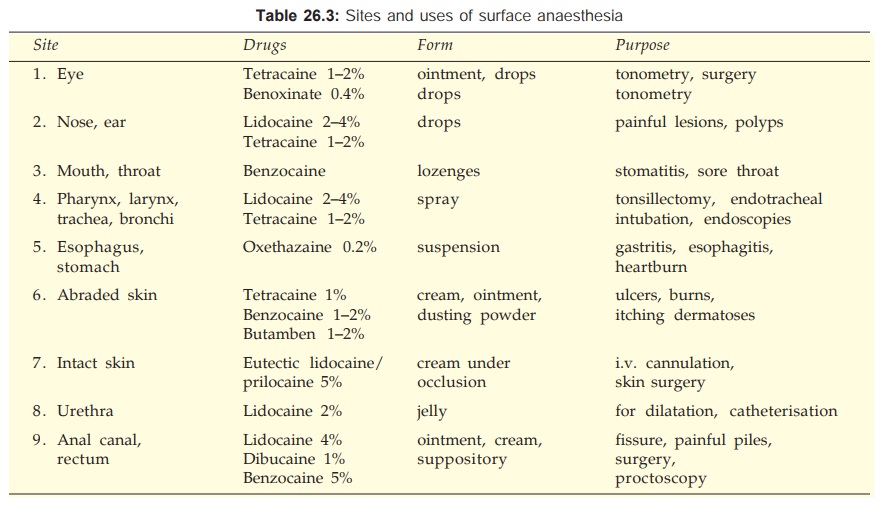
1. Surface Anaesthesia
It is produced by topical
application of a surface anaesthetics to mucous membranes and abraded skin.
Only the superficial layer is anaesthetised. Onset and duration depends on the
site, the drug, its concentration and form, e.g. lidocaine sprayed in the
throat acts in 2–5 min and produces anaesthesia for 30–45 min. Addition of Adr
does not affect duration of topical anaesthesia. Absorption of soluble LAs from
mucous membranes is rapid; blood concentrations of lidocaine and tetracaine sprayed
in throat/ tracheobronchial tree approach those attained on i.v.
injection—toxicity can occur. Except for eutectic lidocaine/prilocaine, no
other LA is capable of anaesthetizing intact skin. The sites and purposes for which
surface anaesthesia is used are given in Table 26.3.
2. Infiltration Anaesthesia
Dilute solution of LA is infiltrated under the skin in the area
of operation—blocks sensory nerve endings. Onset of action is almost immediate
and duration is shorter than that after nerve block, e.g. lidocaine 30–60 min,
bupivacaine 120–180 min. Infiltration is used for minor operations, e.g.
incisions, excisions, hydrocele, herniorrhaphy, etc. when the area to be
anaesthetized is small. Relatively larger amount of LA is required compared to
the area anaesthetised, but motor function is not affected.
3. Conduction
Block
The LA is injected around nerve trunks so that the area distal to
injection is anaesthetised and paralysed. Choice of the LA and its
concentration is mainly dictated by the required duration of action; lidocaine (1–2%) with intermediate duration of action is
most commonly used, but for longer lasting anaesthesia bupivacaine may be
selected.
a) Field Block
It is produced by injecting the LA subcutaneously in a
manner that all nerves coming to a particular field are blocked—as is done for
herniorrhaphy, appendicectomy, dental procedures, scalp stitching, operations
on forearms and legs, etc. Larger area can be anaesthetised with lesser drug
compared to infiltration. The same concentration of LA as for infiltration is
used for field block.
b) Nerve Block It is produced by
injecting the LA around the
appropriate nerve trunks or plexuses. The area of resulting anaesthesia is still
larger compared to the amount of drug used. Muscles supplied by the injected
nerve/plexus are paralysed. The latency of anaesthesia depends on the drug and
the area to be covered by diffusion, e.g. lidocaine anaesthetises intercostal
nerves within 3 min, but brachial plexus block may take 15 min. For plexus
block a ‘flooding’ technique is used and larger volumes are needed. Nerve block
lasts longer than field block or infiltration anaesthesia. Frequently performed
nerve blocks are—lingual, intercostal, ulnar, sciatic, femoral, brachial
plexus, trigeminal, facial, phrenic, etc.—used for tooth extraction, operations
on eye, limbs, abdominal wall, fracture setting, trauma to ribs, neuralgias,
persistent hiccup, etc.
The primary purpose of nerve block anaesthesia is to abolish
pain and other sensations. The accompanying motor paralysis may be advantageous
by providing muscle relaxation during surgery, as well as disadvantageous if it
interferes with breathing, ability to walk after the operation, or participation
of the patient in labour or produces postural hypotension.
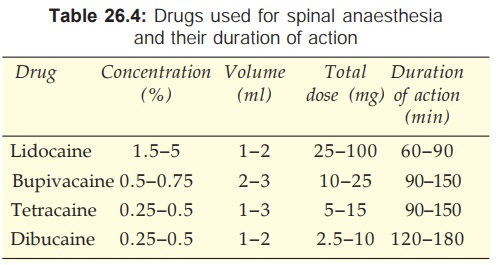
4. Spinal Anaesthesia
The LA is injected in the
subarachnoid space between L2–3 or L3–4 i.e. below the lower end of spinal
cord. The primary site of action is the nerve root in the cauda equina rather
than the spinal cord. Lower abdomen and hind limbs are anaesthetised and
paralysed. The level of anaesthesia depends on the volume and speed of
injection, specific gravity of drug solution and posture
of the patient. The drug solution could be hyperbaric (in 10% glucose) or
isobaric with CSF.
Nerve roots rapidly take up and
retain the LA, therefore, its concentration in CSF falls quickly after
injection. The level of anaesthesia does not change with change of posture
(becomes fixed) after 10 min. Also, higher segments are exposed to
progressively lower concentrations of the LA. Since autonomic preganglionic fibres
are more sensitive and somatic motor fibres less sensitive than somatic sensory
fibres, the level of sympathetic block is about 2 segments higher and the level
of motor paralysis about 2 segments lower than the level of cutaneous analgesia.
The duration of spinal anaesthesia
depends on the drug used and its concentration. Addition of 0.2–0.4 mg of
adrenaline to the LA prolongs spinal anaesthesia by about 1/3rd when measured
by the time taken for the level of sensory block to recede to L1. Adr may be
enhancing spinal anaesthesia by reducing spinal cord blood flow or by its own
analgesic effect exerted through spinal α2 adrenoceptors (intrathecal
clonidine, an α2 agonist produces spinal analgesia by itself).
Women during late pregnancy require
less drug for spinal anaesthesia, because inferior vena cava compression leads
to engorgement of the vertebral system and a decrease in the capacity of
subarachnoid space.
Spinal anaesthesia is used for
operations on the lower limbs, pelvis, lower abdomen, prostatectomy, fracture
setting, obstetric procedures, caesarean section, etc. Its advantages over
general anaesthesia are—
·
It is safer.
·
Produces good analgesia and muscle relaxation
without loss of consciousness.
·
Cardiac, pulmonary, renal disease and diabetes
pose less problem.
Complications Of Spinal Anaesthesia
1.
Respiratory Paralysis is rare; intercostal muscles may be paralysed,
but diaphragm (supplied by phrenic nerve) maintains breathing. Hypotension and
ischaemia of respiratory centre is more frequently the cause of respiratory
failure than diffusion of the anaesthetic to higher centres. Due to paralysis
of external abdominal and intercostal muscles, coughing and expectoration
becomes less effective—pulmonary complications can occur.
2.
Hypotension It is due to blockade of sympathetic vasoconstrictor outflow to
blood vessels; venous pooling and decreased return to the heart contributes more
to the fall in BP than arteriolar dilatation. Venous return is decreased due to
paralysis of skeletal muscles of lower limb. Decreased sympathetic flow to
heart and low venous return produce bradycardia. By promoting venous drainage,
raising the foot end overcomes the hypotension. Sympathomimetics, especially
those with prominent effect on veins (ephedrine, mephentermine) effectively
prevent and counteract hypotension.
3.
Headache is due to seepage of CSF; can be
minimised by using smaller bore needle.
4. Cauda Equina Syndrome is a rare neurological complication resulting
in prolonged loss of control over bladder and bowel sphincters. It may be due
to traumatic damage to nerve roots or chronic arachnoiditis caused by
inadvertent introduction of the antiseptic or particulate matter.
5.
Septic Meningitis due to infection introduced during lumbar puncture; incidence is very low.
6. Nausea and Vomiting
after abdominal operations is due to reflexes initiated by
traction on abdominal viscera. Premedication with opioid analgesics prevents
it.
Contraindications to spinal anaesthesia
·
Hypotension and hypovolemia.
·
Uncooperative or mentally ill patients.
·
Infants and children—control of level is
difficult.
·
Vertebral abnormalities e.g. kyphosis, lordosis,
etc.
·
Sepsis at injection site.
5. Epidural Anaesthesia
The spinal dural space is filled with
semiliquid fat through which nerve roots travel. The LA injected in this
space—acts primarily on nerve roots (in the epidural as well as subarachnoid
spaces to which it diffuses) and small amount permeates through intervertebral foramina
to produce multiple paravertebral blocks. Epidural anaesthesia can be divided
into 3 categories depending on the site of injection.
i) Thoracic Injection is made in
the midthoracic region. The epidural space in this region is relatively narrow,
smaller volume of drug is needed and a wide segmental band of analgesia
involving the middle and lower thoracic dermatomes is produced—used generally
for pain relief following thoracic/upper abdominal surgery.
ii) Lumbar
Relatively large volume of drug is needed because epidural
space is wide. It produces anaesthesia of lower abdomen, pelvis and hind
limbs—use is similar to spinal anaesthesia.
iii) Caudal Injection is given in
the sacral canal through the sacral
hiatus—produces anaesthesia of pelvic and perineal region—used mostly for vaginal
delivery, anorectal and genitourinary operations.
Lidocaine and
bupivacaine are popular drugs for epidural anaesthesia. Duration of anaesthesia
is longer with bupivacaine and action of both the drugs is prolonged by
addition of adrenaline. Technically epidural anaesthesia is more difficult than
spinal anaesthesia and relatively larger volumes of drug are needed— blood
concentrations of the LA are higher. Cardiovascular complications are similar
to that after spinal anaesthesia, but headache and neurological complications
are less because intrathecal space is not entered. The spread of the LA in the
epidural space is governed by the volume injected: larger volume anaesthetizes
more extensive area. Zone of differential sympathetic blockade is not evident
after epidural injection but motor paralysis is 4–5 segments caudal, especially
with lower concentrations of the drug. Greatest separation between sensory and
motor block is obtained by use of 0.25% bupivacaine—especially valuable for obstetric
purposes (mother can participate in labour without feeling pain) and for
postoperative pain relief. Continuous epidural anaesthesia can be instituted by
inserting a catheter and making repeated injections.
6. Intravenous
Regional Anaesthesia (Intravascular Infiltration Anaesthesia)
It consists of
injection of LA in a vein of a
tourniquet occluded limb such that the drug diffuses retrograde from the peripheral
vascular bed to nonvascular tissues including nerve endings. The limb is first
elevated to ensure venous drainage by gravity and then tightly wrapped in an
elastic bandage for maximal exsanguination. Tourniquet is then applied
proximally and inflated to above arterial BP. Elastic bandage is now removed and
20–40 ml of 0.5% lidocaine is injected i.v. under pressure distal to the
tourniquet. Regional analgesia is produced within 2–5 min and lasts till 5–10
min after deflating the tourniquet which is kept inflated for 15–60 min. The
safety of the procedure depends on the rapid uptake of LA by peripheral tissues;
only 1/4 of the injected drug enters systemic circulation when the tourniquet
is released. Bradycardia can occur.
It is mainly used for
the upper limb and for orthopedic procedures. It is more difficult to obstruct
the blood supply of lower limbs and larger volume of anaesthetic is needed (80
ml of 0.25% lidocaine may be required). Bupivacaine should not be employed
because of its higher cardiotoxicity.
Related Topics
