Inhalational Anaesthetics
| Home | | Pharmacology |Chapter: Essential pharmacology : General Anaesthetics
Nitrous oxide (N2O) : It is a colourless, odourless, heavier than air, noninflammable gas supplied under pressure in steel cylinders.
INHALATIONAL ANAESTHETICS
Nitrous oxide (N2O)
It is a colourless, odourless, heavier than air, noninflammable gas supplied under pressure in steel cylinders. It is nonirritating, but low potency anaesthetic; unconsciousness cannot be produced in all individuals without concomitant hypoxia: MAC is 105% implying that even pure N2O cannot produce adequate anaesthesia at 1 atmosphere pressure. Patients maintained on 70% N2O + 30% O2 along with muscle relaxants often recall the events during anaesthesia, but some lose awareness completely.
Nitrous oxide is a good analgesic; even 20% produces analgesia equivalent to that produced by conventional doses of morphine. It is a poor muscle relaxant; neuromuscular blockers are often required. Onset of N2O action is quick and smooth (but thiopentone is often used for induction), recovery is rapid: both because of its low blood solubility. Second gas effect and diffusion hypoxia occur with N2O only. Post-anaesthetic nausea is not marked.
Nitrous oxide is generally used as a carrier and adjuvant to other anaesthetics. A mixture of 70% N2O + 25–30% O2 + 0.2–2% another potent anaesthetic is employed for most surgical procedures. In this way concentration of the other anaesthetic can be reduced to 1/3 for the same level of anaesthesia. Because N2O has little effect on respiration, heart and BP: breathing and circulation are better maintained with the mixture than with the potent anaesthetic given alone in full doses. However, N2O can expand pneumothorax and other abnormal air pockets in the body.
As the sole agent, N2O (50%) has been used with O2 for dental and obstetric analgesia. It is nontoxic to liver, kidney and brain. Metabolism of N2O does not occur; it is quickly removed from body by lungs. It is cheap and very commonly used.
Ether (Diethyl ether)
It is a highly volatile liquid, produces irritating vapours which are inflammable and explosive.
(C2H5 — O — C2H5)
Ether is a potent anaesthetic, produces good analgesia and marked muscle relaxation by reducing ACh output from motor nerve endings —dose of competitive neuromuscular blockers should be reduced to about 1/3.
It is highly soluble in blood—induction is prolonged and unpleasant with struggling, breath-holding, salivation and marked respiratory secretions (atropine must be given as premedication to prevent the patient from drowning in his own secretions). Recovery is slow; post-anaesthetic nausea, vomiting and retching are marked.
BP and respiration are generally well maintained because of reflex stimulation and high sympathetic tone. It does not sensitize the heart to Adr, and is not hepatotoxic.
Ether is not used now in developed countries because of its unpleasant and inflammable properties. However, it is still used in developing countries, particularly in peripheral areas because it is—cheap, can be given by open drop method (though congestion of eye, soreness of trachea and ether burns on face can occur) without the need for any equipment, and is relatively safe even in inexperienced hands.
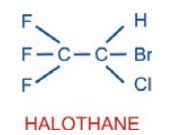
Halothane (FLUOTHANE)
It is a volatile liquid with sweet odour, nonirritant and noninflammable. Solubility in blood is intermediate— induction is reasonably quick and pleasant.
It is a potent anaesthetic—precise control of administered concentration is essential. For induction 24% and for maintenance 0.5–1% is delivered by the use of a special vaporizer. It is not a good analgesic or muscle relaxant; however, it potentiates competitive neuromuscular blockers.
Halothane causes direct depression of myocardial contractility by reducing intracellular Ca2+ concentration. Moreover, sympathetic activity fails to increase (as occurs with ether). Cardiac output is reduced with deepening anaesthesia. BP starts falling early and parallels the depth. Many vascular beds dilate but total peripheral resistance is not significantly reduced. Heart rate is reduced by vagal stimulation, direct depression of SA nodal automaticity and lack of baroreceptor activation even when BP falls. It tends to sensitize the heart to the arrhythmogenic action of Adr. The electrophysiological effects are conducive to reentry—tachyarrhythmias occur occasionally.
Halothane causes relatively greater depression of respiration; breathing is shallow and rapid—PP of CO2 in blood rises if respiration is not assisted. Ventilatory support with added oxygen is frequently required. It tends to accentuate perfusionventilation mismatch in the lungs by causing vasodilatation in hypoxic alveoli.
Pharyngeal and laryngeal reflexes are abolished early and coughing is suppressed while bronchi dilate—preferred for asthmatics. It inhibits intestinal and uterine contractions. This property is utilized for assisting external or internal version during late pregnancy. However, its use during labour can prolong delivery and increase postpartal blood loss.
Urine formation is decreased during halothane anaesthesia—primarily due to low g.f.r. as a result of fall in BP.
Hepatitis occurs in susceptible individuals (approximately 1 in 10,000) especially after repeated use. A metabolite of halothane is probably involved—causes chemical or immunological injury.
A genetically determined reaction malignant hyperthermia occurs rarely. Many susceptible subjects have an abnormal RyR (Ryanodine receptor) calcium channel at the sarcoplasmic reticulum of the skeletal muscles, which is triggered by halothane to release massive amounts of Ca2+ intracellularly causing persistent muscle contraction and increased heat production. Succinylcholine accentuates the condition (see Ch. No. 25). Rapid external cooling, bicarbonate infusion, 100% O2 inhalation and i.v. dantrolene are used to treat malignant hyperthermia.
About 20% of halothane that enters blood is metabolized in the liver, the rest is exhaled out. Elimination may continue for 24–48 hours after prolonged administration. Recovery from halothane anaesthesia is smooth and reasonably quick; shivering may occur but nausea and vomiting are rare. Psychomotor performance and mental ability remain depressed for several hours after regaining consciousness.
It is currently one of the most popular anaesthetics because of nonirritant, noninflammable, pleasant and rapid action, particularly suitable for induction and maintenance in children and as maintenance anaesthetic in adults. However, in affluent countries it has been largely replaced by the newer agents which are costly. Its deficiencies in terms of poor analgesia and muscle relaxation are compensated by concomitant use of N2O or opioids and neuromuscular blockers.
Enflurane
This faster acting substitute of halothane has similar actions, but is less soluble in blood and fat; accumulates in the body to a lesser extent. Because of its propensity to provoke seizures at deeper levels of anaesthesia, it has been superseded by isoflurane which has other desirable properties as well.
Isoflurane (SOFANE)
It is a later introduced (1981) isomer of enflurane; has similar properties, but about 1½ times more potent, more volatile and less soluble in blood. It produces relatively rapid induction and recovery, and is administered through a special vaporizer; 1.5–3% induces anaesthesia in 7–10 min, and 1–2% is used for maintenance.
Magnitude of fall in BP is similar to halothane, but is primarily due to vasodilatation while cardiac output is well maintained. Heart rate is increased. These cardiovascular effects probably result from stimulation of β adrenergic receptors, but it does not sensitize the heart to adrenergic arrhythmias. Coronary circulation is maintained: safer in patients with myocardial ischaemia.
Respiratory depression is prominent and assistance is usually needed to avoid hypercarbia. Secretions are slightly increased.
Uterine and skeletal muscle relaxation is similar to halothane.
Metabolism of isoflurane is negligible. Renal and hepatic toxicity has not been encountered. Postanaesthetic nausea and vomiting is low.
Pupils do not dilate and light reflex is not lost even at deeper levels.
Though slightly irritant, isoflurane has many advantages, i.e. better adjustment of depth of anaesthesia and low toxicity. It is a good maintenance anaesthetic, but not preferred for induction. It does not provoke seizures and is preferred for neurosurgery. Isoflurane has become the routine anaesthetic, but use may be restricted due to cost.
Desflurane
It is a newer all fluorinated congener of isoflurane which has gained popularity as an anaesthetic for out patient surgery in western countries. Though it is highly volatile, a thermostatically heated special vaporizer is used to deliver a precise concentration of pure desflurane vapour in the carrier gas (N2O + O2) mixture. Its distinctive properties are lower oil: gas partition coefficient and very low solubility in blood as well as in tissues, because of which induction and recovery are very fast. Depth of anaesthesia changes rapidly with change in inhaled concentration. Post-anaesthetic cognitive and motor impairment is shortlived— patient can be discharged a few hours after surgery.
Desflurane is less potent than isoflurane; higher concentration has to be used for induction—irritates air passage—may induce coughing, breath-holding and laryngospasm because of somewhat pungent odour making it unsuitable for induction. Rapid induction sometimes causes brief sympathetic stimulation and tachycardia. Degree of respiratory depression, muscle relaxation, vasodilatation and fall in BP, as well as maintained cardiac contractility and coronary circulation are like isoflurane. Lack of seizure provoking potential or arrhythmogenicity and absence of liver as well as kidney toxicity are also similar to isoflurane. It is exhaled unchanged, but more rapidly. As such, desflurane can serve as a good alternative to isoflurane for routine surgery as well, especially prolonged operations.
Sevoflurane
This new polyfluorinated anaesthetic has properties intermediate between isoflurane and desflurane. Solubility in blood and tissues as well as potency are less than isoflurane but more than desflurane.
Induction and emergence from anaesthesia are fast and rapid changes in depth can be achieved. Absence of pungency makes it pleasant and administrable through face mask. Unlike desflurane, it poses no problem in induction; acceptability is good even by pediatric patients. Recovery is smooth; orientation, cognitive and motor functions are regained almost as quickly as with desflurane. Sevoflurane is suitable both for outpatient as well as inpatient surgery, but its high cost and need for highflow open system makes it very expensive to use. In India, only highend hospitals are using it.
Sevoflurane does not cause sympathetic stimulation and airway irritation even during rapid induction. Fall in BP is due to vasodilatation as well as modest cardiac depression. Respiratory depression, absence of seizure and arrhythmia precipitating propensity are similar to isoflurane. About 3% of absorbed sevoflurane is metabolized, but the amount of fluoride liberated is safe for kidney and liver. However, it is degraded by sodalime—not recommended for use in closed circuit.
Related Topics
