High Ceiling (Loop) Diuretics
| Home | | Pharmacology |Chapter: Essential pharmacology : Diuretics
Furosemide: The development of this orally and rapidly acting highly efficacious diuretic was a breakthrough. Its maximal natriuretic effect is much greater than that of other classes.
HIGH CEILING (LOOP) DIURETICS
(Inhibitors of Na+K+2Cl¯ Cotransport)
Furosemide (Frusemide) Prototype drug
The development of this orally and rapidly acting highly efficacious diuretic was a breakthrough. Its maximal natriuretic effect is much greater than that of other classes. The diuretic response goes on increasing with increasing dose: upto 10 L of urine may be produced in a day. It is active even in patients with relatively severe renal failure. The onset of action is prompt (i.v. 2–5 min., i.m. 10–20 min., oral 20–40 min.) and duration short (3–6 hours).
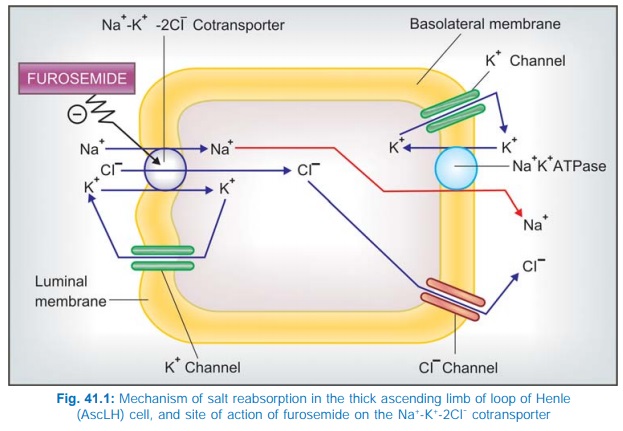
The major site of action is the thick AscLH (site II) where furosemide inhibits Na+ K+2Cl¯ cotransport (Fig. 41.1). A minor component of action on PT has also been indicated. It is secreted in PT by organic anion transport and reaches AscLH where it acts from luminal side of the membrane. It abolishes the corticomedullary osmotic gradient and blocks positive as well as negative free water clearance. K+ excretion is increased mainly due to high Na+ load reaching DT. However, at equinatriuretic doses, K+ loss is less than that with thiazides.
Furosemide has weak CAse inhibitory action and increase HCO3¯ excretion as well; urinary pH may rise but the predominant urinary anion is Cl¯; acidosis does not develop. Its action is independent of acidbase balance of the body and it causes little distortion of the same; mild alkalosis occurs at high doses.
In addition to its prominent tubular action, furosemide causes acute changes in renal and systemic haemodynamics. After 5 min of i.v. injection, renal blood flow is transiently increased and there is redistribution of blood flow from outer to midcortical zone; g.f.r. generally remains unaltered due to compensatory mechanisms despite increased renal blood flow. Pressure relationship between vascular, interstitial and tubular compartments is altered, the net result of which is decreased PT reabsorption. The intrarenal haemodynamic changes are brought about by increased local PG synthesis.
Intravenous furosemide causes prompt increase in systemic venous capacitance and decreases left ventricular filling pressure, even before the saluretic response is apparent. This action also appears to be PG mediated and is responsible for the quick relief it affords in LVF and pulmonary edema.
Furosemide increases Ca2+ excretion (contrast thiazides which reduce it) as well as Mg2+ excretion. It tends to raise blood uric acid level by competing with its proximal tubular secretion as well as by increasing reabsorption in PT which is a consequence of reduced e.c.f. volume.
The magnitude of hyperuricaemia is lower than that with thiazides. Hyperglycaemic action of furosemide is also less marked than thiazides.
Molecular Mechanism Of Action:
A glycoprotein with 12 membrane spanning domains has been found to function as the Na+K+2Cl¯ cotransporter in many epithelia performing secretory/ absorbing function, including AscLH. Recently, distinct absorptive or secretory isoforms of Na+K+2Cl¯ cotransporter have been isolated. The former is exclusively expressed at the luminal membrane of thick AscLH—furosemide attaches to the Cl¯ binding site of this protein to inhibit its transport function. The secretory form is expressed on the basolateral membrane of most glandular and epithelial cells.
Pharmacokinetics
Furosemide is rapidly absorbed orally but bioavailability is about 60%. In severe CHF oral bioavailability may be markedly reduced. Lipidsolubility is low, and it is highly bound to plasma proteins. It is partly conjugated with glucuronic acid and mainly excreted unchanged by glomerular filtration as well as tubular secretion. Some excretion in bile and directly in intestine also occurs. Plasma t½ averages 1–2 hour but is prolonged in patients with pulmonary edema, renal and hepatic insufficiency.
Dose Usually 20–80 mg once daily in the morning. In renal insufficiency, upto 200 mg 6 hourly has been given by i.m./i.v. route. In pulmonary edema 40–80 mg may be given i.v.
LASIX 40 mg tab., 20 mg/2 ml inj. LASIX HIGH DOSE 500 mg tab, 250 mg/25 ml inj; (solution degrades spontaneously on exposure to light), SALINEX 40 mg tab, FRUSENEX 40, 100 mg tab.
Bumetanide
It is similar to furosemide in all respects, but is 40 times more potent. It induces very rapid diuresis and is highly effective in pulmonary edema. However, the site of action, ceiling effect, renal haemodynamic changes and duration of action are similar to furosemide. A secondary action in PT has also been demonstrated. It may act in some cases not responding to furosemide. Hyperuricaemia, K+ loss, glucose intolerance and ototoxicity are claimed to be less than with furosemide. However, it may rarely cause myopathy.
Bumetanide is more lipidsoluble, 80–100% bioavailable orally, extensively bound to plasma proteins, partly metabolized and partly excreted unchanged in urine. Its accumulation in tubular fluid is less dependent on active secretion. Plasma t½ ~60 min, gets prolonged in renal and hepatic insufficiency.
Dose: 1–5 mg oral OD in the morning, 2–4 mg i.m./i.v., (max. 15 mg/day in renal failure).
BUMET, 1 mg tab., 0.25 mg/ml inj.
Torasemide (Torsemide)
Another high ceiling diuretic with properties similar to furosemide, but 3 times more potent. Oral absorption is more rapid and more complete. The elimination t½ (3.5 hours) and duration of action (4–8 hours) are longer. Torasemide has been used in edema and in hypertension.
Dose: 2.5–5 mg OD in hypertension; 5–20 mg/day in edema; upto 100 mg BD in renal failure.
DIURETOR 10, 20 mg tabs, DYTOR 10, 20, 100 mg tabs.
Use Of High Ceiling Diuretics
a) Edema Diuretics are used irrespective of etiology of edema—cardiac, hepatic or renal. The high ceiling diuretics are preferred in CHF for rapid mobilization of edema fluid (see Ch. No. 37). Thiazides may be used for maintenance, but often prove ineffective and high ceiling drugs are called in. For nephrotic and other forms of resistant edema, the high ceiling diuretics are the drugs of choice. In chronic renal failure massive doses have to be used, but they continue to be effective while thiazides just do not produce any action. In impending acute renal failure, loop diuretics may decrease the need for dialysis.
b) Acute Pulmonary Edema (Acute LVF, Following MI): Intravenous administration of furosemide or its congeners produces prompt relief. This is due to vasodilator action that precedes the saluretic action. Subsequently, decrease in blood volume and venous return is responsible for the improvement.
c) Cerebral Edema: Though osmotic diuretics are primarily used, furosemide may be combined to improve efficacy.
d) Hypertension: High ceiling diuretics are indicated only in presence of renal insufficiency, CHF, in resistant cases or hypertensive emergencies; otherwise thiazides are preferred.
e) Along with blood transfusion in severe anaemia, to prevent vascular overload.
f) Hypercalcaemia and renal calcium stones: because furosemide and its congeners increase calcium excretion and urine flow, they may help to reduce serum calcium level. Excess salt that is lost must be replaced.
Forced diuresis with saline and furosemide infusion is no longer recommended to treat poisonings.
Related Topics
