Hemostasis
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Blood
1. What is the difference between a thrombus and an embolus? 2. List the major steps involved in blood clot formation. 3. Define the terms hemostasis, vasospasm, and prothrombin. 4. Identify the three pathways to the activation of the clotting system.
Hemostasis
The stoppage of bleeding is known as hemostasis. When blood vessels are damaged, this vital process helps to limit or prevent blood loss. It involves several steps, including blood vessel spasms, the formation of a platelet plug, and coagulation of the blood.
The process of hemostasis is quick and localized, involving
a variety of clotting factors from
the plasma, along with substances released by platelets and injured tissue
cells. The three steps of hemostasis are vaso-spasm or vascular spasm, platelet plug formation, and coagulation (blood clotting). After hemostasis, theclot retracts
and eventually dissolves to be replaced by fibrous tissue that prevents any
additional blood loss.
Step 1: Vasospasm
When a smaller blood vessel is cut or broken, smooth muscles
in its walls contract, which is known as vaso-spasm, and loss of blood slows nearly immediately.
Avasospasm has the potential to completely close the ends of a severed vessel.
The vascular spasm lasts for approximately 30 minutes and is also known as the vas-cular phase of hemostasis. The
endothelial cells contractto expose the basement membrane to the bloodstream.
Chemical factors and local hormones begin to be released by
the endothelial cells. Also released are endothelins, which are peptide hormones that stimu-late
smooth muscle contraction and promote vascular spasms. They also stimulate
endothelial cell division, smooth muscle cell division, and fibroblast division
to accelerate repair of damaged tissue.
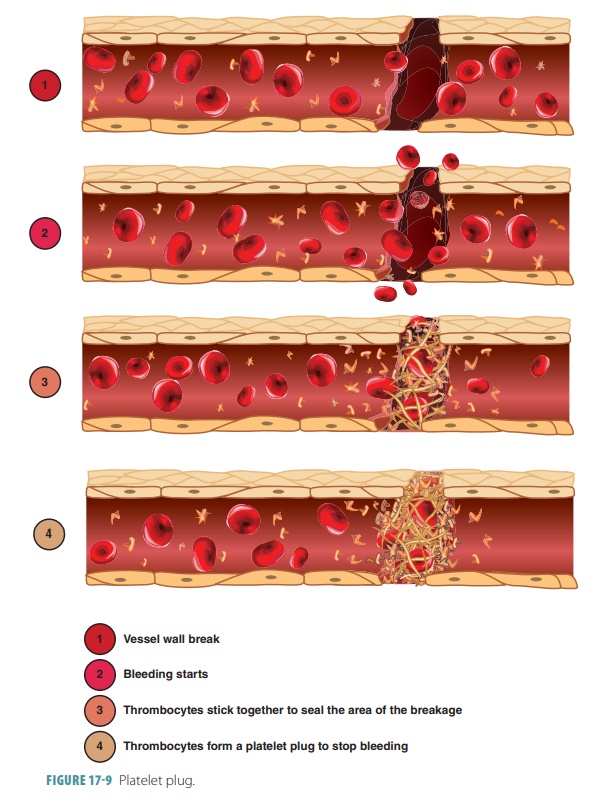
Step 2: Platelet Plug Formation
In the platelet phase, a platelet plug forms
because of platelet aggregation, and
blood begins coagulating (FIGURE
17-9). Platelets release serotonin to contract smooth muscles in blood vessels, reducing blood
loss. In platelet adhesion, the
platelets stick to rough sur-faces and connective tissue collagen under the
endo-thelial blood vessel lining. They also stick to each other to form a
platelet plug in the area of the blood vessel injury. Larger breaks may require
a blood clot to stop bleeding. The growth of the platelet plug is
limited by several following important factors:
■■
The endothelial cells release a prostaglandin known as prostacyclin,
which inhibits platelet aggregation.
■■
White blood cells entering the area release inhibitory compounds.
■■
Adenosine diphosphate near the platelet plug is broken down by
circulating plasma enzymes.
■■
Compounds such as serotonin inhibit platelet plug formation once
they are present in high quantities.
■■
The development of a blood clot strengthens the platelet plug but
isolates the platelet plug from the general circulation.
Step 3: Coagulation
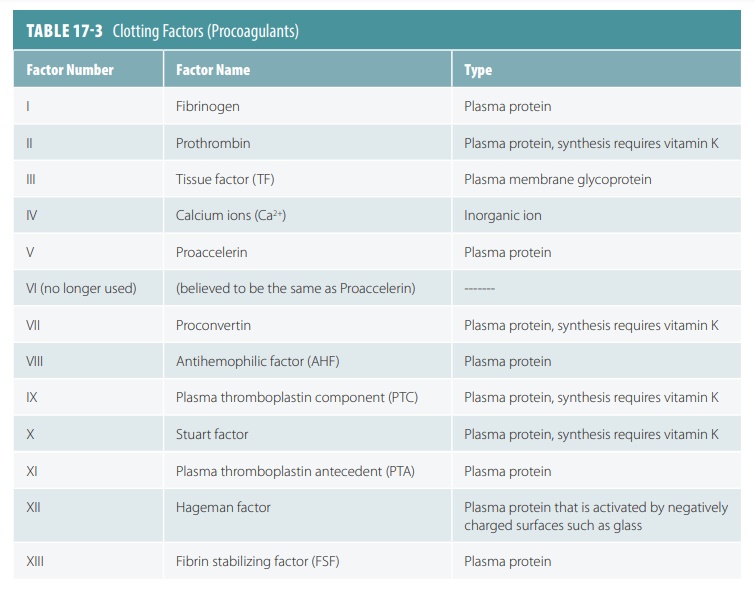
The
formation of a blood clot is known as coagulation.
The coagulation phase requires
many biochemicals known as clotting factors or
procoagulants. They are synthesized by the liver. Some
clotting factors promote coagulation, whereas others inhibit it, so a delicate
balance between these two types is achieved to address the specific injured tissue
(TABLE 17 -3). Many
present proteins or proenzymes
control vital reactions in the clotting response. Calcium ions and vitamin K are very important for nearly
all of the coagulation process. Adequate amounts of vitamin K must be present
in the liver for it to synthesize prothrombin and other clotting factors.
The most important event in coagulation is the conversion of
the plasma protein fibrinogen into
the insoluble threads of the protein called fibrin.
The first step is the release of tissue thromboplastin, which results in the
production of prothrombin activator. FIGURE 17-10 describes the
blood-clotting cascade.
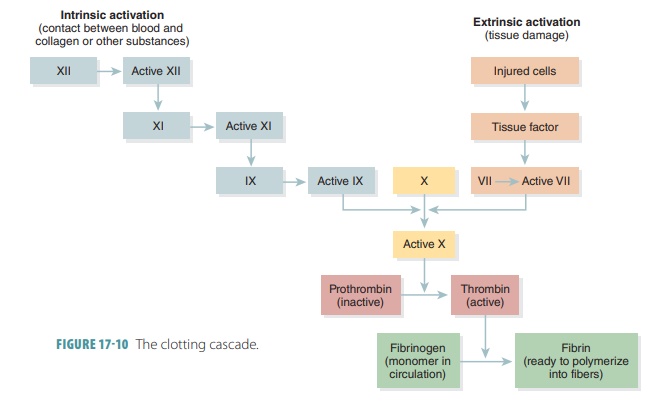
The three pathways to the activation of the clot-ting system
are the extrinsic pathway, the intrinsicpathway,and the common pathway. When dam-aged
endothelial cells or peripheral tissues release Factor III ortissue factor, the extrinsic pathwaybegins.
Tissue factor combines with calcium ions and Factor VII, forming an enzyme complex that is able to activate Factor X, which is the first stage of
the common pathway. The intrinsic
pathway starts with activation of proenzymes, primarily Factor XII, exposed to collagen fibers
at the site of injury. A plate-let factor known as PF-3 assists the process. Other factors speed up the reactions in
this pathway, and eventually, activated Factor
VIII and Factor IX com-bine,
forming an enzyme complex that can activate Factor
X. The common pathway begins as the enzyme prothrombinase is formed.
Prothrombin is an alpha globulin made in theliver on a continual basis and is always present in the blood plasma. Prothrombinase converts prothrom-bin into thrombin, which causes fibrinogen to be cut into sections of fibrin. This fibrin then joins to form long threads. The threads stick to surfaces of damaged blood vessels to create a mesh that traps blood cells and platelets. The result is a blood clot. A clear, yellowish liquid remains after formation of the clot. This liquid is called serum and is plasma minus its clotting factors.
More prothrombinase becomes present if tissue damage is more
severe. Continual clotting occurs to stop greater damage. Positive feedback is
used to stimulate more clotting action based on the original clotting action.
However, this continual process can only work for a short time because it
interrupts the stability of the body’s internal environment. Excess thrombin is
normally carried away to avoid the for-mation of a massive blood clot. As a
result, blood coagulation usually occurs in blood that is not mov-ing or only
moving slowly. Clotting stops where a clot contacts the circulating blood.
Blood clots in ruptured vessels are invaded by fibroblasts
to produce fibrous connective tissue that helps seal blood vessel breaks. Clots
that form in tissues as a result of blood leakage are called hematomas, which disappear over time. This
process requires the plasma protein plasminogen to be converted to plasmin, an enzyme that digests threads of
fibrin and other proteins involved in clotting. Although plasmin may dissolve
entire clots, those that fill large blood vessels usually are not removed
naturally. Plasmin is also called fibrinolysin.
Substances that Control Coagulation
Certain substances deactivate or remove clotting factors as
well as other stimulatory agents from the blood to control coagulation.
Examples of these substances include plasma
anticoagulants such as antithrombin
III; heparin,
which is the naturalanticoagulant released by basophils and mast cells; aspirin ; thrombomodulin, which is released by endo-thelial cells, binds to
thrombin, and converts it to an enzyme that activates proteinC , which
inacti-vates clotting factors and helps to form plasmin; prostacyclin,
which inhibits platelet aggregationand opposes thrombin and adenosine
diphosphate; alpha-2 -macroglobulin,
which inhibits thrombin;and C1
inactivator, which inhibits several intrinsic clotting factors.
Retraction of the Clot
Syneresis is also
known asclot retraction, in
whichthe torn edges of a damaged vessel are pulled closer together. This
reduces bleeding and stabilizes the site of injury. It also reduces the size of
the area of damage, so that fibrocytes, endothelial cells, and smooth mus-cle
cells can continue the repair process.
Fibrinolysis
Over time, the clot dissolves as fibrinolysis starts by activation of plasminogen by thrombin as
well as tis-sue plasminogen activator.
This activator is releasedby damaged tissues at the injury site. Plasminogen
then leads to production of plasmin,
the enzyme that begins digestion of the fibrin strands and erosion of the clot.
1. What is the difference between a thrombus and an embolus?
2. List the major steps involved in blood clot formation.
3. Define the terms hemostasis,
vasospasm, and prothrombin.
4. Identify the three pathways to the activation of the
clotting system.