H1 Antagonists / Conventional Antihistaminics
| Home | | Pharmacology |Chapter: Essential pharmacology : Histamine And Antihistaminics
These drugs competitively antagonize actions of histamine at the H1 receptors. The first compounds of this type were introduced in the late 1930s and have subsequently proliferated into an unnecessary motley of drugs.
H1 ANTAGONISTS
(Conventional Antihistaminics)
These
drugs competitively antagonize actions of histamine at the H1
receptors. The first compounds of this type were introduced in the late 1930s
and have subsequently proliferated into an unnecessary motley of drugs.
Nevertheless, they are frequently used for a variety of purposes. More commonly
employed now are the less sedating second generation H1
antihistamines that have been added after 1980. Seemingly, H1
antihistaminics have diverse chemical structures, but majority have a substituted
ethylamine side chain.
Pharmacological Actions
Qualitatively
all H 1 antihistaminics have similar actions, but there are
quantitative differences, especially in the sedative property.
1. Antagonism Of Histamine
They
effectively block histamine induced
bronchoconstriction, contraction of intestinal and other smooth muscle and triple
response—especially wheal, flare and itArticle No. Fall in BP produced by low
doses of histamine is blocked, but additional H2 antagonists are
required for complete blockade of higher doses. Pretreatment with these drugs
protects animals from death caused by i.v. injection of large doses of
histamine. Release of Adr from adrenal medulla in response to histamine is
abolished. Constriction of larger blood vessel by histamine is also antagonized.
Action of histamine on gastric secretion is singularly not affected by these
drugs.
2. Antiallergic action
Many manifestations of immediate
hypersensitivity (type I reactions) are suppressed. Urticaria, itching and
angioedema are well controlled. Anaphylactic fall in BP is only partially
prevented. Asthma in man is practically unaffected though anaphylactic
bronchoconstriction in guinea pig is largely prevented. This tissue and species
dependence of response probably reflects extent of involvement of histamine in
the reaction. It is now well established that leukotrienes (C4 and D4)
and PAF are more important mediators for human asthma.
3. CNS
The older antihistamines produce variable degree of CNS depression. This appears
to depend on the compound’s ability to penetrate bloodbrain barrier and its
affinity for the central (compared to peripheral) H1 receptors.
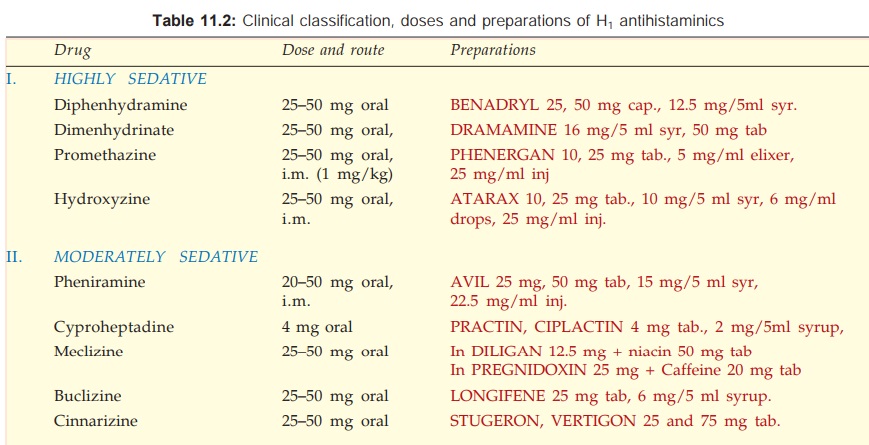
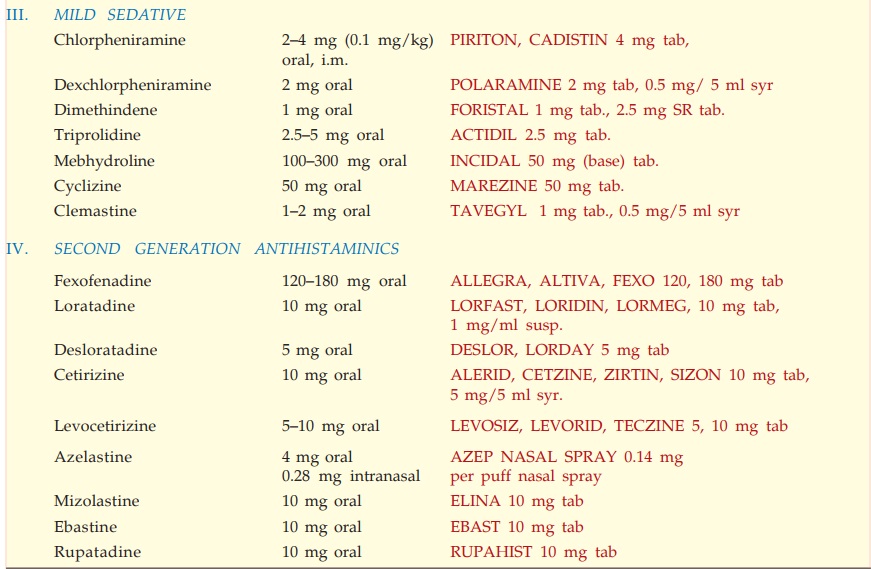
Individual susceptibility to different agents varies considerably, but an
overall grading of the sedative property is presented in Table 11.2. Some
individuals also experience stimulant effects like restlessness and insomnia.
Excitement and convulsions are frequently seen at toxic doses. The second
generation anti-histaminics are practically non-sedating.
Certain
H1 antihistamines are effective in preventing motion sickness. It is
not certain whether this is due to antagonism of histamine in the brain or
reflects antimuscarinic property of these drugs. Promethazine also controls vomiting
of pregnancy and other causes.
Promethazine
and few other antihistaminics reduce tremor, rigidity and sialorrhoea of parkinsonism.
Anticholinergic and sedative properties underlie the benefit.
Some
H1 antihistamines are also effective antitussives.
1. Anticholinergic Action
Many
H1 blockers in addition antagonize muscarinic actions of AArticle
No. The anticholinergic action can be graded as:
High Low Minimal/Absent
Promethazine Chlorpheniramine Fexofenadine
Diphenhydramine Hydroxyzine Astemizole
Dimenhydrinate Triprolidine Loratadine
Pheniramine Cyclizine Cetirizine
Cyproheptadine Mizolastine
If
used concurrently with atropine or its substitutes, phenothiazines, tricyclic
antidepressants or disopyramide, the anticholinergic action adds up.
2. Local Anaesthetic
Some drugs like pheniramine,
have strong while others have weak membrane stabilizing property. However, they
are not used clinically as local anaesthetic because they cause irritation when
injected s.c.
Membrane stabilizing
activity also confers antiarrhythmic property to these compounds.
6. BP
Most antihistaminics cause a fall in BP on i.v. injection (direct smooth muscle
relaxation). However, this is not evident on oral administration.
Pharmacokinetics
The classical H1
antihistaminics are well absorbed from oral and parenteral routes, metabolized
in the liver and excreted in urine. They are widely distributed in the body and
enter brain. The newer compounds penetrate brain poorly. Duration of action of
most agents is 4–6 hours, except meclizine, loratadine, cetirizine and
fexofenadine which act for 12–24 hours or more.
Side Effects And Toxicity
Side effects with
first generation H1 antihistaminics are frequent, but are generally
mild. Individuals show marked differences in susceptibility to side effects with
different drugs. Some tolerance to side effects develops on repeated use.
Sedation, diminished
alertness and concentration, light headedness, motor incoordination, fatigue
and tendency to fall asleep are the most common. Objective testing shows impairment
of psychomotor performance. Patients should be cautioned not to operate motor
vehicles or machinery requiring constant attention. Alcohol synergises in
producing these effects as do other CNS depressants. Few individuals become
restless, nervous and are unable to sleep. Second generation compounds are largely
free of CNS effects.
Dryness of mouth,
alteration of bowel movement, urinary hesitancy and blurring of vision can be
ascribed to anticholinergic property.
Epigastric distress
and headache are also common.
Local application can
cause contact dermatitis.
Some
like cyclizine and fexofenadine are teratogenic in animals; but not in humans;
caution is nevertheless to be exercised during pregnancy.
Acute
overdose produces central excitation, tremors, hallucinations, muscular incordination,
convulsions, flushing, hypotension, fever and some other features of belladonna
poisoning. Death is due to respiratory and cardiovascular failure.
Second Generation Antihistaminics
The second generation
antihistaminics (SGAs) may be defined as those H1 receptor blockers
marketed after 1980 which have one or more of the following properties :
·
Higher H1 selectivitiy: no
anticholinergic side effects.
·
Absence of CNS depressant property.
·
Additional antiallergic mechanisms apart from
histamine blockade: some also inhibit late phase allergic reaction by acting on
leukotrienes or by antiplatelet activating factor effect.
Some
recent compounds like fexofenadine and cetirizine that are active metabolites
of earlier drugs have also been referred as ‘third generation antihistamines’,
but this has not been accepted by an international concensus group of experts.
These
newer drugs have the advantage of not impairing psychomotor performance (driving
etc. need not be contraindicated), produce no subjective effects, no sleepiness,
do not potentiate alcohol or benzodiazepines. Some patients do complain of
sedation, but incidence is similar to placebo. However, they have a narrow
spectrum of therapeutic usefulness which is limited by the extent of
involvement of histamine (acting through H1 receptors) in the
disease state. Their principal indications are:
·
Allergic rhinitis and conjunctivitis, hay
fever, pollinosis—control sneezing, runny but not blocked nose, and red,
watering, itchy eyes.
·
Urticaria, dermographism, atopic eczema.
·
Acute allergic reactions to drugs and foods.
They have poor antipruritic, antiemetic and antitussive actions.
Fexofenadine
It is the active
metabolite of terfenadine, the first
nonsedating SGA that was withdrawn because of several deaths due to polymorphic
ventricular tachycarida (Torsades de pointes) occurring with its higher doses
or when it was coadministered with
CYP3A4 inhibitors (erythromycin, clarithromycin, ketoconazole, itraconazole,
etc.). This toxicity is based on blockade of delayed rectifier K+ channels in
the heart at higher concentrations. Astemizole is another SGA banned for the
same reason. Fexofenadine has a low propensity to block delayed rectifier K+ channels,
does not prolong QTc interval; no interaction with CYP3A4 inhibitors have been reported.
It is largely free of arrhythmogenic potential, but some cases of ventricular
arrhythmia in patients with preexisting long QT interval have been reported. Thus,
it is not entirely safe in patients with long QT, bradycardia or hypokalemia.
Fexofenadine does not cross blood-brain
barrier—does not produce sedation or impair psychomotor performance and is free
of atropinic side effects. It is rapidly absorbed, excreted unchanged in urine
and bile, has plasma t½ 11– 16 hours and duration of action 24 hours. Though
erythromycin and ketoconazole increase its blood levels, but no arrhythmias
have been observed.
Dose: For allergic rhinitis
120 mg OD; for urticaria and other
skin allergies 180 mg OD.
Loratadine
Another longacting selective peripheral H1
antagonist which lacks CNS depressant effects and is fast acting. It is partly
metabolized by CYP3A4 to an active metabolite with a longer t½ of 17 hr, but
has not produced cardiac arrhythmia in overdose, though seizures are reported.
No interaction with macrolides or antifungals has been noted. Good efficacy has
been reported in urticaria and atopic dermatitis.
Desloratadine
It is the major active metabolite of loratadine effective at half the dose. Noninterference
with psychomotor performance and cardiac safety are documented.
Cetirizine
It is a metabolite of hydroxyzine with marked affinity for peripheral H1
receptors; penetrates brain poorly, but subjective somnolence has been
experienced at higher doses. It is not metabolized; does not prolong cardiac action
potential or produce arrhythmias when given with erythromycin/ketoconazole.
Cetirizine in addition inhibits release of histamine and of
cytotoxic mediators from platelets as well as eosinophil chemotaxis during the
secondary phase of the allergic response. Thus, it may benefit allergic
disorders by other actions as well. It attains high and longer lasting
concentration in skin, which may be responsible for superior efficacy in
urticaria/atopic dermatitis, as well as for once daily dosing despite elimination
t½ of 710 hr. It is indicated in upper respiratory allergies, pollinosis,
urticaria and atopic dermatitis; also used as adjuvant in seasonal asthma.
Levocetirizine
It is the active R(–) enantiomer of cetirizine. It is effective at half the dose
and appears to produce few side effects.
Azelastine
This newer H1 blocker has good topical activity; in addition inhibits
histamine release and inflammatory reaction triggered by LTs and PAF; and has
bronchodilator property. After intranasal application it has been shown to down
regulate intracellular adhesion molecule1 (ICAM1) expression on nasal mucosa.
Its t½ is 24 hr, but action lasts longer due to active metabolite. Its
metabolism is inhibited by CYP 3A4 inhibitors. Given by nasal spray for
seasonal and perennial allergic rhinitis it provides quick symptomatic relief
lasting 12 hr. Stinging in the nose and altered taste perception are the local
side effects. Some somnolence has been reported on nasal application and a
tendency to weight gain noted after oral use.
Mizolastine
This nonsedating antihistaminic is effective in allergic rhinitis and
urticaria by single daily dosing despite a t½ of 8–10 hr and no active
metabolite.
Ebastine
Another newer SGA that rapidly gets converted to the
active metabolite carbastine having a t½ of 10–16 hr. It is non-sedating and
active in nasal and skin allergies. Animal studies have found it to prolong QTc
interval which makes it liable to arrhythmogenic potential and CYP3A4 interaction,
but actual reports are still few.
Rupatadine
This
recently introduced antihistaminic has additional PAF antagonistic property,
and is indicated in allergic rhinitis.
Uses
The
uses of H1 antihistaminics are based on their ability to block certain
effects of histamine released endogeneously, as well as on sedative and anticholinergic
properties.
1. Allergic Disorders
Antihistaminics do not suppress AG: AB
reaction, but block the effects of released histamine—are only palliative. They
effectively control certain immediate type of allergies, e.g. itching,
urticaria, seasonal hay fever, allergic conjunctivitis and angioedema of lips,
eyelids, etc. However, their action is slow—Adr alone is lifesaving in
laryngeal angioedema. Similarly, they cannot be relied upon in anaphylactic
shock and have a secondary place to Adr. Benefits are less marked in perennial
vasomotor rhinitis, atopic dermatitis and chronic urticarias; combination with
an H2 antagonist succeeds in some cases of chronic urticaria not
responding to H1 antagonist alone.
The
antihistaminics are ineffective in bronchial asthma: reasons may be—
a.
Leukotrienes (C4, D4)
and PAF are more important mediators than histamine.
b.
Concentration of antihistamines attained at
the site may not be sufficient to block high concentration of histamine
released locally in the bronchi.
Certain
newer compounds like cetirizine have adjuvant role in seasonal asthma.
Antihistaminics
are also ineffective in other types of humoral and cell mediated allergies because
histamine is not involved. They do suppress urticaria and swellings in serum
sickness, but not other components of the syndrome.
Type I hypersensitivity reactions to drugs (except asthma and
anaphylaxis) are suppressed. Some skin rashes also respond.
2. Other Conditions
Involving Histamine
Antihistaminics
block symptoms produced by histamine liberators; afford symptomatic relief in
insect bite and ivy poisoning. Abnormal dermographism is suppressed. They have
prophylactic value in blood/saline infusion induced rigor.
3. Pruritides
Many conventional antihistamines have antipruritic action independent of H1
antagonism. Though relief is often incomplete, older antihistaminics remain the
first choice drugs for idiopathic pruritus.
4. Common
Cold
Antihistaminics do not affect the course of the
illness but may afford symptomatic relief by anticholinergic (reduce
rhinorrhoea) and sedative actions. The newer nonsedating antihistamines are
less effective in this respect.
5. Motion
Sickness
Promethazine, diphenhydramine, dimenhydrinate and cyclizine have
prophylactic value in milder types of motion sickness; should be taken one hour
before starting journey. Promethazine can also be used in morning sickness,
drug induced and postoperative vomiting, radiation sickness. Cyproheptadine has
appetite stimulating effect; has been used in underweight children.
6. Vertigo
Cinnarizine is the H1 antihistamine having additional anticholinergic, anti5HT,
sedative and vasodilator properties which has been widely used in vertigo. It
modulates Ca2+ fluxes and attenuates vasoconstrictor action of many endogenous
substances.
Cinnarizine inhibits
vestibular sensory nuclei in the inner ear, suppresses postrotatory
labyrinthine reflexes, possibly by reducing stimulated influx of Ca2+ from
endolymph into the vestibular sensory cells. Beneficial effects have been
reported in Méniére’s disease and other types of vertigo. Side effects are
sedation and mild g.i. upset.
Related Topics
