Glucocorticoid Actions
| Home | | Pharmacology |Chapter: Essential pharmacology : Corticosteroids
Glucocorticoids promote glycogen deposition in liver (they are assayed on the basis of this action) by inducing hepatic glycogen synthase and promoting gluconeogenesis.
GLUCOCORTICOID ACTIONS
1. Carbohydrate And Protein Metabolism
Glucocorticoids
promote glycogen deposition in liver (they are assayed on the basis of this
action) by inducing hepatic glycogen synthase and promoting gluconeogenesis.
They inhibit glucose utilization by peripheral tissues. This along with
increased glucose release from liver results in hyperglycaemia, resistance to
insulin and a diabeteslike state. They also cause protein breakdown and amino
acid mobilization from peripheral tissues—responsible for side effectslike
muscle wasting, lympholysis, loss of osteoid from bone and thinning of skin.
The amino acids so mobilized funnel into liver → used up in gluconeogenesis,
excess urea is produced → negative nitrogen balance. Glucocorticoids
are thus catabolic. Their function appears to be aimed at maintaining blood
glucose levels during starvation—so that brain continues to get its nutrient.
When food is withheld from an adrenalectomized animal—liver glycogen is rapidly
depleted and hypoglycaemia occurs.
They also increase
uric acid excretion.
2. Fat Metabolism
The action is primarily permissive in nature:
promote lipolysis due to glucagon, growth hormone, Adr and thyroxine. cAMP
induced breakdown of triglycerides is enhanced. Fat depots in different areas
respond differently—redistribution of body fat occurs. Subcutaneous tissue over
extremities loses fat which is deposited over face, neck and shoulder —‘moon
face’, ‘fish mouth’, ‘buffalo hump’. Explanation offered is—because peripheral
adipocytes are less sensitive to insulin, corticosteroid enhanced lipolytic
action of GH and Adr predominates, whereas truncal adipocytes respond mainly to
enhanced insulin levels under the influence of glucocorticoids.
3. Calcium Metabolism
They
inhibit intestinal absorption and enhance renal excretion of Ca2+. There is
also loss of calcium from bone indirectly due to loss of osteoid (decreased
formation and increased resorption), negative calcium balance. Spongy bones
(vertebrae, ribs, etc.) are more sensitive.
4. Water Excretion
Effect on water excretion is independent of action on Na+ transport;
hydrocortisone and other glucocorticoids, but not aldosterone, maintain normal
g.f.r. In adrenal insufficiency, the capacity to excrete a water load is
markedly reduced—such patients are prone to water intoxication from i.v.
infusions.
Glucocorticoids
also enhance secretory activity of renal tubules.
5. CVS
Glucocorticoids restrict capillary permeability, maintain tone
of arterioles and myocardial contractility. Applied topically, they cause
cutaneous vasoconstriction. They have a permissive effect on pressor action of
Adr and angiotensin. They also play a permissive role in development of
hypertension—should be cautiously used in hypertensives.
Adrenal
insufficiency is attended by low cardiac output, arteriolar dilatation, poor
response to Adr (repeated doses of Adr cause destructive changes in blood
vessels) and increased permeability of capillaries. These changes along with
hypovolemia (due to lack of mineralocorticoid) are responsible for cardiovascular
collapse.
6. Skeletal Muscles
Optimum level of corticosteroids is needed for
normal muscular activity. Weakness occurs in both hypo and hypercorticism, but
the causes are different.
Hypocorticism: diminished work
capacity and weakness are primarily
due to hypodynamic circulation.
Hypercorticism: excess
mineralocorticoid action →
hypokalaemia → weakness;
Excess
glucocorticoid action → muscle wasting and myopathy → weakness.
7. CNS
Mild euphoria is quite
common with pharmacological doses
of glucocorticoids. This is a direct effect on brain, independent of relief of
disease
symptoms; sometimes progresses to cause increased motor activity, insomnia, and
hypomania or depression. On the other hand, patients of Addison’s disease
suffer from apathy, depression and occasionally psychosis.
Glucocorticoids
also maintain the level of sensory perception and normal level of excitability
of neurones. High doses lower seizure threshold—cautious use in epileptics.
This action is independent of electrolyte changes in the brain and is not
shared by aldosterone.
8. Stomach
Secretion of gastric acid and pepsin is increased—may aggravate
peptic ulcer.
9. Lymphoid Tissue And Blood Cells
Glucocorticoids enhance the rate of destruction of lymphoid
cells (T cells are more sensitive than B cells); but in man the effect on
normal lymphoid tissue is modest. However, a marked lytic response is shown by
malignant lymphatic cells; basis of their use in lymphomas.
Glucocorticoids
increase the number of RBCs, platelets and neutrophils in circulation. They
decrease lymphocytes, eosinophils and basophils. This is not due to destruction
of these cells but due to their sequestration in tissues. Blood counts come
back to normal after 24 hours.
10. Inflammatory Responses
Irrespective
of the type of injury or insult, the
attending inflammatory response is suppressed by glucocorticoids. This is the
basis of most of their clinical uses. The action is nonspecific and covers all
components and stages of inflammation. This includes reduction of—increased
capillary permeability, local exudation, cellular infiltration, phagocytic activity
and late responses like capillary proliferation, collagen deposition,
fibroblastic activity and ultimately scar formation. The action is direct and
local—topical use is possible. The cardinal signs of inflammation—redness,
heat, swelling and pain are suppressed.
Glucocorticoids
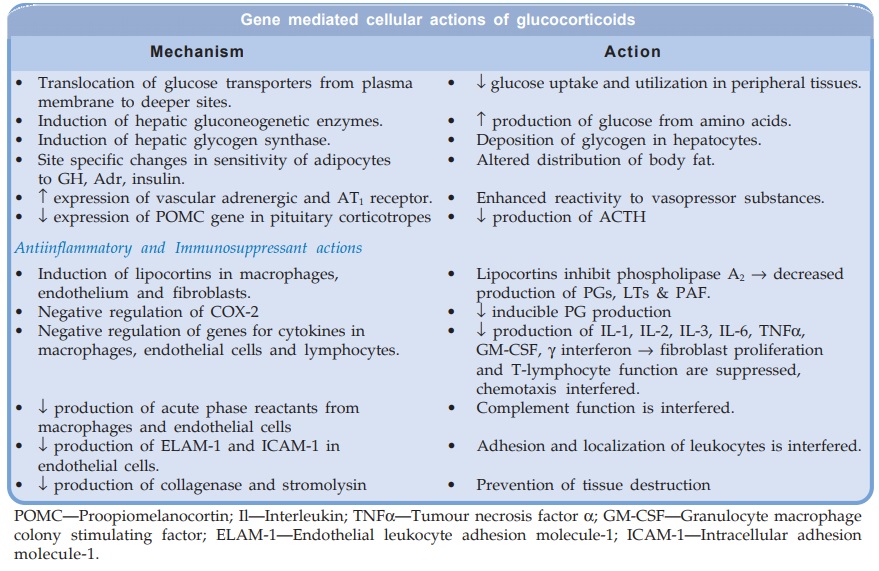
interfere at several steps in the inflammatory response (see cellular mechanism below), but the most important overall mechanism
appears to be limitation of recruitment of inflammatory cells at the local site
and production of proinflammatory mediators like PGs, LTs, PAF through
inhibition of phospholipase A2.
Corticoids
are only palliative, do not remove the cause of inflammation; the underlying
disease continues to progress while manifestations are dampened. They favour
spread of infections because capacity of defensive cells to kill microorganisms
is impaired. They also interfere with healing and scar formation: peptic ulcer
may perforate asymptomatically. Indiscriminate use of corticoids is hazardous.
11. Immunological And Allergic Responses
Glucocorticoids impair
immunological competence. They suppress all types of hypersensitization and
allergic phenomena. At high concentrations and in vitro they have been shown to interfere with practically every
step of the immunological response, but at therapeutic doses in vivo there is no impairment of
antibody production or complement
function. The clinical effect appears to be due to suppression of recruitment
of leukocytes at the site of contact with antigen and of inflammatory response
to immunological injury.
They cause greater
suppression of CMI in which T cells are primarily involved, e.g. delayed
hypersensitivity and graft rejection—basis of use in autoimmune diseases and
organ transplantation (see Ch. No. 63).
Factors involved may be inhibition of IL1 release from macrophages; inhibition
of IL2 formation and action → T cell proliferation is not stimulated;
suppression of natural killer cells, etc.
The broad action seems
to be interruption of communication between cells involved in the immune
process by interfering with production of or action of lymphokines.
Related Topics
