General Senses
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Peripheral Nervous System and Reflex Activity
The general senses of touch, pressure, temperature, and pain are spread throughout the body via muscle, joint, skin, and visceral receptors.
General
Senses
The general
senses of touch, pressure,
temperature, and pain are spread throughout the body via muscle, joint, skin,
and visceral receptors. They are also known as the somatic senses and involve relatively simple receptors. General
sensory receptors are nerve endings of two types: nonencapsulated (free) or encap-sulated.
The senses of touch and pressure utilize both of these types.
NonEncapsulated (Free) Nerve Endings
Nonencapsulated
(free) nerve endings of the sensory neurons are
very common in epithelia and connective tissues. They are mostly non-myelinated
with group C fibers that are small in diameter. Their distal endings called sensory terminals often have small,
knob-like swellings. They mostly respond to temperature and painful stimuli in
the skin and internal tissues, except for the brain. They may also respond to
tissue movements that are influenced by pressure. Pain receptors are stimulated
by tissue damage but adapt to improving conditions poorly. They may send pain
impulses persistently to the CNS regardless of whether tissue damage is
continuing, making pain persist. Pain is triggered by releases of certain
chemicals and deficiency of oxygen-rich blood (a
condition known as ischemia) or the
stimulation of certain mechanoreceptors.
Temperature is sensed via warm receptors and cold receptors . In the superficial dermis, nerve end-ings respond
to cold temperatures. Cold receptors are most sensitive to temperatures between
50°F (10°C) and 68°F (20°C) to produce a freezing sen-sation. These receptors
work rapidly, and sensation begins to fade away after approximately one minute
of continuous stimulation. Deeper in the dermis are nerve endings that respond
to warmer temperatures. Warm receptors are most sensitive to temperatures above
77°F (25°C), becoming unresponsive to tem-peratures above 113°F (45°C) . At
this temperature, pain receptors are stimulated to produce a burning sensation.
Any temperatures outside the
range of thermo-receptors activate the nociceptors and is perceived as painful.
The nociceptors also respond to chemi-cals that are released from damaged
tissues and to pinching of the skin.
A plasma membrane protein called the vanilloid receptor is
important in the detection of painful stimuli. This protein is actu-ally an ion
channel. It is opened by heat, low pH, and chemicals such as capsaicin, which is found in hot
peppers.
Free nerve endings may extend
between epithe-lial cells and control the sensation of itching. The itch receptor
of the dermis has an extremely thin diameter, and was not discovered until long after other types of receptors
were recognized. The nerve endings related to itching are activated by many
different chemicals, but mostly histamine,
which is present in areas of inflammation. Other types of nonencapsulated nerve
endings include:
■■ Tactile (Merkel) discs:
Within the deepest epidermal layer, they are receptors for light touch. They
are formed by certain free nerve endings associated with enlarged tactile or Merkel cells.
■■ Hair follicle receptors:
Wrapping around hair follicles, these are light touch receptors that detect the
bending of hairs, which may occur when an insect lands on the skin.
Encapsulated Nerve Endings
Encapsulated
nerve endings are those that
contain one or more fiber terminals of sensory neurons. These
neurons are enclosed in connective tissue capsules. Almost all encapsulated
receptors are mechanorecep-tors, though there are wide variations in
distribution over the body, shape, and size. Encapsulated nerve endings
include:
■■ Meissner’s (tactile) corpuscles:
Oval yet flattened connective tissue cells, with two or more fibers spiraling
into each corpuscle to end in small knobs; located in hairless skin
(fingertips, lips, palms, soles, external genitalia, and nipples), they respond
to objects that lightly touch the skin. They are small receptors surrounded by
Schwann cells, and then thin, egg-shaped connective capsules.
■■ Pacinian (lamellar) corpuscles:
Scattered deep in the dermis and subcutaneous tissue, they are mechanoreceptors
stimulated by deep pressure, but only when it is first applied. This makes them
able to monitor vibrations as on/off pressure stimuli. These corpuscles are the
longest in size, sometimes more than 3 mm long and 1.5 mm wide. They can be
seen by the naked eye as white, egg-shaped structures. They have a single
dendrite surrounded by a capsule of as many as 60 layers of collagen fibers
with flat supporting cells.
■■ Bulbous corpuscles (Ruffini
endings): They are tactile receptors found in the dermis, subcutaneous
tissue, and joint capsules, their receptor endings are enclosed by flattened
capsules. They look similar to tendon organs and function to monitor changes in
dense connective tissues, responding to deep and continuous pressure.
■■ Muscle spindles: Fusiform
(spindle-shaped) pro-prioceptors throughout the skeletal muscle per-imysium.
Each of them has a bundle of modified intrafusal
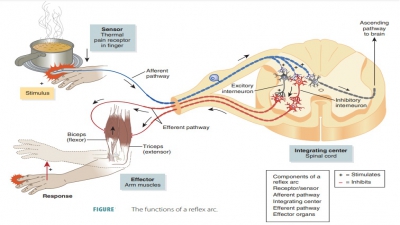
fibers within a connective tissue capsule. Muscle spindles function to detect muscle stretch-ing. They
initiate a reflex that resists this stretching.
■■ Tendon organs: Proprioceptors
inside tendons, near junctions
between the tendons and skeletal muscle. They have small bundles of collagenous
fibers inside a layered capsule. Sensory termi-nals coil between and around
their fibers. When tendon fibers stretch due to muscle contraction, compression
of nerve fibers activates the tendon organs (proprioceptors). A reflex is
initiated that causes the contracting muscle to relax.
■■ Joint kinesthetic receptors:
Proprioceptors that monitor
stretching of articular capsules enclos-ing synovial joints. They have at least
four recep-tor types, including free nerve endings, lamellar corpuscles,
bulbous corpuscles, and receptors that look like tendon organs. Together, these
receptors communicate information about joint positions and motions of which we
are aware.
Somatosensory System
Sensation is the awareness of environmental changes both externally and
internally. To survive, humans rely on sensation as well as how they interpret
these changes (perception). How we respond to sensations is determined by our
perceptions of them. The part of the sensory system that serves the limbs and
wall of the body is known as the somatosensory
system. Input is received
from exteroceptors, interoceptors, and proprioceptors. The somatosensory system
trans-mits information about various sensations. The sen-sory receptors make up
the receptor level of this system, whereas processing in the ascending
pathways makes up its circuit level. The processing in the cor-tical
sensory areas is called its perceptual level. For sensations to
occur, stimuli must excite a receptor and action potentials must reach the CNS.
Sensory neurons may be called
either tonic receptors or phasic
receptors. Tonic receptors are always active.
The rate at which action poten-tials are generated changes when stimulus
increases or decreases. Phasic receptors are normally inactive, but become
active for a short period of time when a change occurs in the conditions they
monitor. These receptors provide information about intensity and rates of
change of a stimulus.
Adaptation is a reduced sensitivity, whereas a stimulus is
consistently present. Peripheral
adaptation occurs as levels of receptor activity change. The initial strong response subsides over time, partly because the size of the
generator potential decreases gradually. This is typical of phasic receptors,
and for this reason, they are also called fast-adapting
receptors. The tonic receptors are called slow-adapting receptors because they show little peripheral
adaptation. Pain receptors or nociceptors
are examples of slow-adapting recep-tors. Central
adaptation refers to inhibition of nuclei located along a sensory pathway.
Pain Receptors in Visceral Organs
Pain receptors in the visceral
organs act differently from those located in surface tissues. When vis-ceral
tissues are stimulated on a widespread basis, strong pain sensations can
follow. This type of pain appears to be caused by mechanoreceptor stimulation,
decreased oxygenated blood flow, or accumulation of pain-stimulating chemicals.
Visceral pain may seem to be coming from a different area of the body from the
one actually being stimulated. This is known as referred
pain. Heart pain, for
example, may appear to be occurring in the shoulder or upper left arm.
Referred pain may arise from
different areas, including the skin and viscera. Heart pain impulses travel
through the same nerve pathways as do skin pain impulses such as those from the
skin of the left shoulder and upper left arm. A heart attack may, therefore,
fool the cerebral cortex into interpreting pain impulses as if they are coming
from the shoulder or arm instead.
Acute pain fibers are thin, myelinated nerve fibers that conduct nerve impulses rapidly and
mostly produce sharp pain. Acute pain is usually sensed as coming from the
skin. Chronic pain fibers are thin,
unmyelinated nerve fibers that conduct impulses more slowly and mostly produce
dull, aching pain. Chronic pain is usually sensed as coming from deeper within
the body. Pain stimulation often causes both types of sensations—a sharp pain
followed by a dull ache. The aching pain is often more intense, worsening as
time passes, and can cause prolonged suffering.
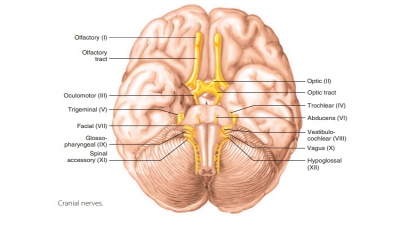
The cranial nerves sense pain
impulses origi-nating from the head. All other pain impulses travel through the
spinal nerves. The spinal cord’s neurons process pain impulses in its gray
matter to transmit them to the brain. Other neurons conduct impulses to the thalamus,
hypothalamus, and cerebral cortex. Pain awareness occurs when pain impulses
reach the thalamus; however, it is the cerebral cortex that con-trols the
body’s response to pain. The midbrain, pons, and medulla oblongata regulate how
pain impulses move from the spinal cord. Biochemicals are released to block
pain signals by inhibiting presynaptic nerve fibers in the spinal cord.
The posterior horn of the spinal
cord releases enkephalins to suppress pain impulses of various severities.
Enkephalins bind to the same receptor sites on neuronal membranes as the drug
morphine. Serotonin is also released, which helps by stimulat-ing further
enkephalin release. Endorphins also have pain suppression actions and are found in the
pituitary gland. Both enkephalins and endorphins are released in response to
extreme pain. Endorphins can inhibit impulses initiated by nociceptors.
1. Identify
which type of receptor is exemplified by thermoreceptors, mechanoreceptors, and
chemoreceptors and explain to what they respond.
2. Explain
the locations of sensory receptors of the general senses and the special
senses.
3. Differentiate
between the terms “sensation” and “perception.”
4. Explain
nonencapsulated (free) nerve endings.
5. Describe
encapsulated nerve endings.
Related Topics