Drugs Used in Gout
| Home | | Pharmacology |Chapter: Essential pharmacology : Antirheumatoid and Antigout Drugs
Gout It is a metabolic disorder characterized by hyperuricaemia (normal plasma urate 1–4 mg/ dl). Uric acid, a product of purine metabolism, has low water solubility, especially at low pH. When blood levels are high, it precipitates and deposits in joints, kidney and subcutaneous tissue (tophy).
DRUGS USED IN GOUT
Gout It is a metabolic disorder characterized by hyperuricaemia (normal plasma urate 1–4 mg/
dl). Uric acid, a product of purine metabolism, has low water solubility,
especially at low pH. When blood levels are high, it precipitates and deposits
in joints, kidney and subcutaneous tissue (tophy).
Secondary Hyperuricaemia Occurs
In:
·
Leukaemias, lymphomas, polycythaemia—
especially when treated with chemotherapy or radiation: due to enhanced nucleic
acid metabolism and uric acid production.
·
Drug induced—thiazides, furosemide, pyrazinamide,
ethambutol, levodopa, clofibrate reduce uric acid excretion by kidney.
Drugs used in gout
are:
For
Acute Gout
a)
NSAIDs
b)
Colchicine
c)
Corticosteroids
For Chronic Gout / Hyperuricaemia
1. Uricosurics
Probenecid, Sulfinpyrazone
2. Synthesis inhibitor
Allopurinol
Acute Gout
Acute gout manifests
as sudden onset of severe inflammation in a small joint (commonest is metatarsophalangeal
joint of great toe) due to precipitation of urate crystals in the joint space.
The
joint becomes red, swollen and extremely painful: requires immediate treatment.
1. NSAIDs
One
of the strong anti-inflammatory drugs, e.g. indomethacin,
naproxen, piroxicam, diclofenac or
etoricoxib is given in relatively high and quickly repeated doses. They are quite effective in terminating the
attack, but may take 12–24 hours, i.e. response is somewhat slower than with
colchicine, but they are generally better tolerated; majority of patients
prefer them over colchicine. Their strong anti-inflammatory (not uricosuric)
action is responsible for the benefit. Naproxen and piroxicam specifically
inhibit chemotactic migration of leucocytes into the inflamed joint. After the
attack is over, they may be continued at lower doses for 3–4 weeks while drugs
to control hyper-uricaemia take effect. They are not recommended for long term
management due to risk of toxicity.
The
NSAIDs have also substituted colchicine for covering up the period of
initiation of therapy (6–8 weeks) with allopurinol or uricosurics in chronic
gout.
2. Colchicine
It
is an alkaloid from Colchicum autumnale
which was used in gout since 1763. The pure alkaloid was isolated in 1820.
Colchicine
is neither analgesic nor anti-inflammatory, but it especifically suppresses
gouty inflammation. It does not inhibit the synthesis or promote the excretion
of uric acid. Thus, it has no effect on blood uric acid levels.
An acute attack of
gout is started by the precipitation of urate crystals in the synovial fluid.
They start an inflammatory response, chemotactic factors are produced → granulocyte migration
into the joint; they phagocytose urate crystals and release a glycoprotein
which aggravates the inflammation by:
·
Increasing lactic acid production from
inflammatory cells → local pH is reduced → more urate crystals are precipitated in the affected joint.
·
Releasing lysosomal enzymes which cause joint
destruction.
Colchicine
does not affect phagocytosis of urate crystals but inhibits release of the
glycoprotein and the subsequent events. By binding to fibrillar protein
tubulin, it inhibits granulocyte migration into the inflamed joint and thus
interrupts the vicious cycle. Other actions of colchicine are:
·
Antimitotic: causes metaphase arrest by
binding to microtubules of mitotic spindle. It was tried for cancer
chemotherapy but abandoned due to toxicity. It is used to produce polyploidy in
plants.
·
Increases gut motility through neural mechanisms.
Pharmacokinetics
Colchicine
is rapidly absorbed orally, partly metabolized in liver and excreted in
bile—undergoes enterohepatic circulation; ultimate disposal occurs in urine and
faeces over many days.
Toxicity is high and dose
related.
Nausea,
vomiting, watery or bloody diarrhoea and abdominal cramps occur as dose
limiting adverse effects. Accumulation of the drug in intestine and inhibition
of mitosis in its rapid turnover mucosa is responsible for the toxicity. In
overdose, colchicine produces kidney damage, CNS depression, intestinal
bleeding; death is due to muscular paralysis and respiratory failure.
Chronic
therapy with colchicine is not recommended because it causes aplastic anaemia,
agranulocytosis, myopathy and loss of hair.
Use
(a) Treatment of acute gout
Colchicine
is the fastest acting drug to control an acute attack of gout; 1 mg orally
followed by 0.25 mg 1–3 hourly till control of the attack is achieved (occurs
in 4– 12 hour), or till total dose 6 mg is reached, or diarrhoea starts. The
response is dramatic, so much so that it may be considered diagnostic. However,
because of higher toxicity, most physicians prefer using a NSAID. Maintenance
doses (0.5–1 mg/day) may be given for 4–8 weeks in which time control of
hyperuricaemia is achieved with other drugs.
(b) Prophylaxis
Colchicine
0.5–1 mg/day can prevent further
attacks of acute gout, but NSAIDs are generally preferred.
Taken
at the first symptom of an attack, small doses (0.5–1.5 mg) of colchicine abort
it.
COLCHINDON, GOUTNIL
0.5 mg tab.
3. Corticosteroids
Intraarticular injection of a soluble steroid suppresses
symptoms of acute gout. Crystalline preparations should not be used. It is
indicated in refractory cases and those not tolerating NSAIDs/ colchicine.
Systemic
steroids are rarely needed. They are very effective and produce nearly as rapid a response as colchicine,
but are reserved for patients with renal failure/history of peptic ulcer bleed
in whom NSAIDs are contraindicated or for cases not responding to or not
tolerating NSAIDs. Prednisolone 40–60 mg may be given in one day, followed by
tapering doses over few weeks.
Chronic Gout
When
pain and stiffness persist in a joint between attacks, gout has become chronic.
Other cardinal features are hyperuricaemia, tophi (chalklike stones under the
skin in pinna, eyelids, nose, around joints and other places) and urate stones
in the kidney. Chronic gouty arthritis may cause progressive disability and
permanent deformities.
A. URICOSURIC DRUGS
1. Probenecid
It is a highly lipid soluble
organic acid developed in 1951 to inhibit renal tubular secretion of penicillin
so that its duration of action could be prolonged. It competitively blocks
active transport of organic acids by OATP at all sites; that in renal tubules
being the most prominent. This transport is bidirectional: net effect depends
on whether secretion or reabsorption of the particular organic acid is quantitatively
more important, e.g.:
·
Penicillin is predominantly secreted by the
proximal tubules, its reabsorption is minimal. Net effect of probenecid is
inhibition of excretion; more sustained blood levels are achieved.
·
Uric acid is largely reabsorbed by active
transport, while less of it is secreted; only 1/10th of filtered load is
excreted in urine. Probenecid, therefore, promotes its excretion and reduces
its blood level.
Probenecid does not
have any other significant pharmacological action; it is neither analgesic nor anti-inflammatory.
Interactions
i.
In addition to penicillins, probenecid
inhibits the urinary excretion of cephalosporins, sulfonamides, Mtx and
indomethacin.
ii.
It inhibits biliary excretion of rifampicin.
Pyrazinamide and ethambutol may interfere with uricosuric action of probenecid.
iii.
Probenecid inhibits tubular secretion of
nitrofurantoin which may not attain antibacterial concentration in urine.
iv.
Salicylates block uricosuric action of probenecid.
Pharmacokinetics
Probenecid is completely absorbed orally; 90% plasma protein bound:
partly conjugated in liver and excreted by the kidney; plasma t½ is 8–10 hours.
Adverse Effects
Probenecid is
generally well tolerated.
Dispepsia is the most
common side effect (upto 25% incidence with high doses). It should be used
cautiously in peptic ulcer patients. Rashes and other hypersensitivity
phenomena are rare. Toxic doses cause convulsions and respiratory failure.
Uses
1.
Chronic gout and hyperuricaemia: Probenecid is a second line/adjuvant drug to
allopurinol. Started at 0.25 g BD and increased to 0.5 g BD, it gradually lowers
blood urate level; arthritis, tophi and other lesions may take months to
resolve. Colchicine/NSAID cover is advised during the initial 1–2 months to
avoid precipitation of acute gout.
Probenecid
and other uricosurics are ineffective in the presence of renal insufficiency
(serum creatinine > 2 mg/dl). Plenty of fluids should be given with
probenecid to avoid urate crystallization in urinary tract.
2. Probenecid is also used to prolong penicillin or ampicillin
action by enhancing and sustaining their blood levels, e.g. in gonorrhoea,
SABE.
BENEMID, BENCID 0.5 g
tab.
2. Sulfinpyrazone
It
is a pyrazolone derivative related to phenylbutazone having consistent
uricosuric action, but is neither analgesic nor anti-inflammatory. At the usual
therapeutic doses, it inhibits tubular reabsorption of uric acid, but smaller
doses can decrease urate excretion as do small doses of probenecid. Its
uricosuric action is additive with probenecid but antagonised by salicylates.
It inhibits platelet aggregation.
Pharmacokinetics
Sulfinpyrazone
is well absorbed orally; 98% plasma protein bound—displacement interactions can
occur. Excretion is fairly rapid, mainly by active secretion in proximal
tubule. Uricosuric action of a single dose lasts for 6–10 hours.
Sulfinpyrazone
inhibits metabolism of sulfonylureas and warfarin.
Adverse effects
Gastric irritation is
the most common side
effect—contraindicated in patients with peptic ulcer.
Rashes
and other hypersensitivity reactions are uncommon.
Unlike
phenylbutazone, it does not produce fluid retention or blood dyscrasias.
Uses
In chronic gout, the
results are comparable to probenecid; same precautions should be exercised.
Start with 100–200 mg BD, gradually
increase
according to response, maximal dose 800 mg/day.
ANTURANE,
ARTIRAN 200 mg cap.
Benzbromarone is another uricosuric
drug marketed in Europe, but not in
India.
B. URIC ACID SYNTHESIS INHIBITOR
Allopurinol
This
hypoxanthine analogue was synthesized as a purine antimetabolite for cancer
chemotherapy. However, it had no antineoplastic activity but was a substrate as
well as inhibitor of xanthine oxidase, the enzyme responsible for uric
acid synthesis (Fig. 15.1).
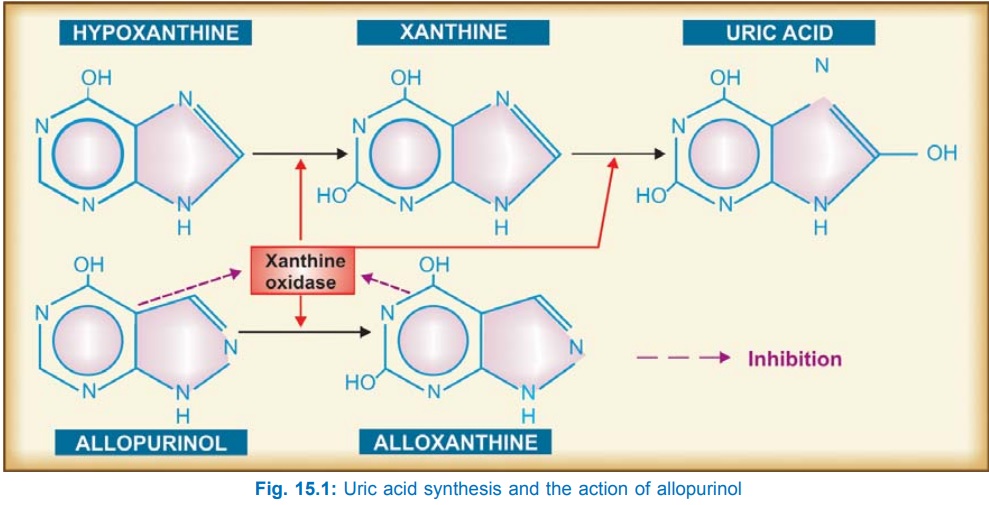
Allopurinol
itself is a short acting (t½ 2 hrs) competitive inhibitor of xanthine oxidase,
but its major metabolite alloxanthine
(oxypurine) is a long acting (t½ 24 hrs) and noncompetitive inhibitor—
primarily responsible for uric acid synthesis inhibition in vivo. During allopurinol administration, plasma concentration of
uric acid is reduced and that of hypoxanthine and xanthine is somewhat
increased. In place of uric acid alone, all 3 oxipurines are excreted in urine.
Since xanthine and hypoxanthine are more soluble, have a higher renal clearance
than that of uric acid and each has its individual solubility, precipitation
and crystallization in tissues and urine does not occur.
Because
of raised levels of xanthine and hypoxanthine, some feedback inhibition of de novo purine synthesis and reutilization
of metabolically derived purine also occurs.
Pharmacokinetics
About
80% of orally administered allopurinol is absorbed. It is not bound to plasma
proteins; metabolized largely to alloxanthine. During chronic medication, it
inhibits its own metabolism and about 1/3rd is excreted unchanged, the rest as
alloxanthine.
Interactions
a)
Allopurinol inhibits the degradation of 6mercaptopurine
and azathioprine: their doses should be reduced to 1/3rd, but not that of
thioguanine, because it follows a different metabolic path (Smethylation).
b) Probenecid given with
allopurinol has complex interaction; while probenecid shortens t½ of
alloxanthine, allopurinol prolongs t½ of probenecid.
c)
Allopurinol can potentiate warfarin and
theophylline by inhibiting their metabolism.
d) A higher incidence of
skin rashes has been reported when ampicillin is given to patients on
allopurinol.
e)
Iron therapy is not recommended during
allopurinol treatment. The exact nature of interaction is not known, but
interference with mobilization of hepatic iron stores is suggested.
Adverse Effects
These
are uncommon. Hypersensitivity
reaction consisting of rashes, fever, malaise and muscle pain is the most
frequent. It subsides on stopping the drug. Renal impairment increases the
incidence of rashes and other reactions to allopurinol.
Stevens-Johnson
syndrome is a rare but serious risk.
Gastric
irritation, headache, nausea and dizziness are infrequent; do not need withdrawal.
Liver damage is rare.
Precautions And Contraindications
Liberal fluid intake is advocated during allopurinol
therapy.
It is contraindicated
in hypersensitive patients, during pregnancy and lactation.
It should be
cautiously used in the elderly, children and in kidney or liver disease.
Uses
Allopurinol is the
first choice drug in chronic
gout. It can be used in both
over producers and under excretors
of uric acid, particularly more severe cases, with tophi or nephropathy.
Uricosurics are infrequently used in India; they are less effective when g.f.r.
is low and are inappropriate in stone formers. The two classes of drugs can
also be used together when the body load of urate is large.
With long term
allopurinol therapy, tophi gradually disappear and nephropathy is halted, even
reversed.
Secondary hyperuricaemia due to cancer chemotherapy/radiation/thiazides
or other drugs: can be controlled by allopurinol. It can even be used
prophylactically in these situations.
To potentiate 6-mercaptopurine or azathioprine in cancer
chemotherapy and immunosuppressant therapy.
Dose: Start with 100 mg OD,
gradually increase to maintenance dose of 300 mg/day; maximum 600 mg/day.
ZYLORIC 100, 300 mg
tabs., ZYLOPRIM, CIPLORIC 100 mg cap.
Caution
Allopurinol as well as
uricosurics should not be started
during acute attack of gout. During the initial 1–2 months of treatment with
these drugs, attacks of acute gout are more common—probably due to fluctuating
plasma urate levels favouring intermittent solubilization and recrystallization
in joints; cover with NSAIDs/colchicine may be provided.
Kalaazar
Allopurinol inhibits Leishmania by altering its purine
metabolism. It is used as adjuvant to sodium stibogluconate in resistant kalaazar
cases (see Ch. No. 60).
