Drugs For Glaucoma
| Home | | Pharmacology |Chapter: Essential pharmacology : Antiadrenergic Drugs (Adrenergic Receptor Antagonists) And Drugs For Glaucoma
Glaucoma is a group of diseases characterized by a progressive form of optic nerve damage. This is generally associated with raised (> 21 mmHg) intraocular tension (i.o.t), but the etiology is unknown and there are many risk factors.
DRUGS FOR GLAUCOMA
Glaucoma is a group of
diseases characterized by a progressive form of optic nerve damage. This is
generally associated with raised (> 21 mmHg) intraocular tension (i.o.t),
but the etiology is unknown and there are many risk factors. The chief therapeutic
measure is to lower i.o.t. to target level, either by reducing secretion of
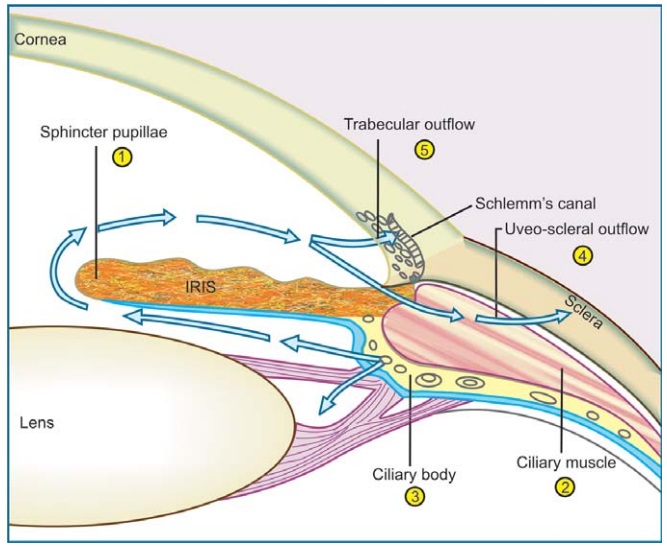
aqueous humor or by promoting its drainage. The site of formation and pathway
of drainage of aqueous humor as well as sites of action of antiglaucoma drugs
is illustrated in Fig. 10.1. Major amount of aqueous (~90%) drains through the trabecular route, while ~10% fluid
passes into the connective tissue spaces within the ciliary muscle—then via suprachoroid into episcleral vessels
(uveoscleral outflow). Glaucoma is seen in
two principal clinical forms:
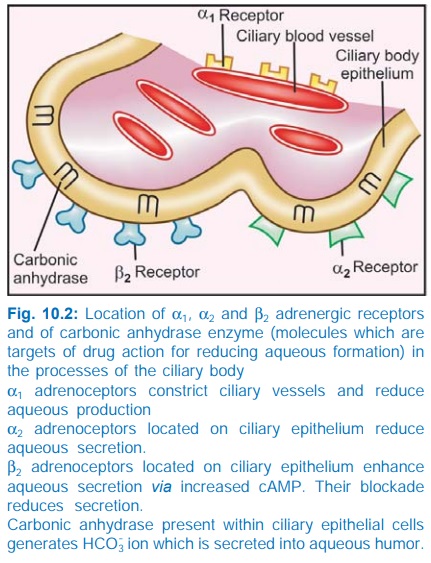
A. Open Angle (Wide Angle, Chronic Simple) Glaucoma
It
is probably a genetically predisposed degenerative disease affecting patency of
the trabecular meshwork which is gradually lost past middle age. The i.o.t.
rises insidiously and progressively. Ocular hypotensive drugs are used on a
long term basis and constitute the definitive treatment in majority of cases.
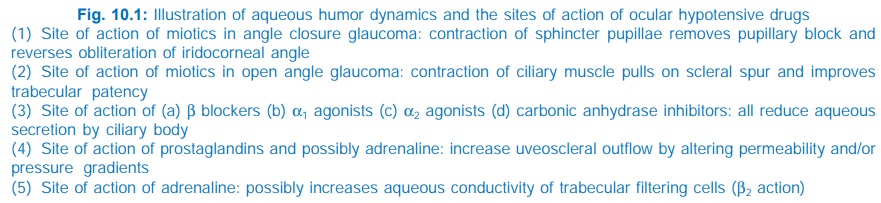
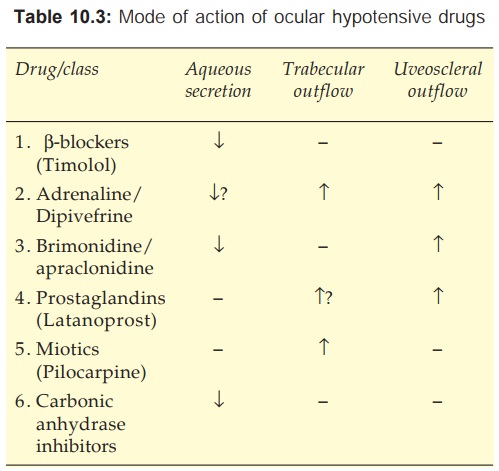
1. β Adrenergic blockers
Topical β blockers are one of
the first line drugs, but PG F2α analogues are
increasingly used now. In contrast to miotics, the β blockers do not
affect pupil size, tone of ciliary muscle or outflow facility, but lower i.o.t.
by reducing aqueous formation. This probably results from down regulation of
adenylylcyclase due to β2 receptor blockade in
the ciliary epithelium and a secondary effect due to reduction in ocular blood
flow. They are as effective as miotics and produce less ocular side effects.
Ocular β blockers are
lipophilic with high ocular capture (to reduce systemic effects) and have
no/weak local anaesthetic activity (to avoid corneal hypoesthesia and damage).
Advantages of topical
β blockers over miotics
· No induced myopia which is especially
troublesome in young patients
· · No change in pupil size: no diminution of vision in dim light and in patients with cataract
· No headache/brow pain due to persistent spasm
of iris and ciliary muscles
·
No fluctuations in i.o.t. as occur with
pilocarpine drops
·
Convenient twice/once daily application sufficient
Ocular side effects of β
blockers viz. stinging, redness and dryness of eye, corneal
hypoesthesia, allergic blepharon-conjunctivitis and blurred vision are
generally mild and infrequent. Their major limitation are the systemic adverse effects that occur due
to absorption through nasolacrimal duct. Life threatening bronchospasm has been
reported in asthmatics. Bradycardia, accentuation of heart block and CHF are
likely, especially in the elderly. In fact all adverse effects and
contraindications of systemic β blocker therapy apply to ocular β blockers as well.
Timolol It is the prototype of ocular β blockers; is nonselective (β1 + β2) and has no local
anaesthetic or intrinsic sympathomimetic activity. The ocular hypotensive
action (20–35% fall in i.o.t.) is smooth and well sustained. After chronic use,
effect on i.o.t. persists for 2–3 weeks following discontinuation. This
feature, in contrast to pilocarpine drops, gives a high level of clinical
safety, i.e. 1 or 2 missed doses will not affect i.o.t. control. However, upto
30% cases of open angle glaucoma fail to achieve the desired level of i.o.t.
with timolol alone, and may need additional medication.
GLUCOMOL, OCUPRES,
IOTIM, LOPRES 0.25%
and 0.5% eye drops; start with 0.25% drops BD, change to 0.5% drops in
case of inadequate response.
Betaxolol It is β1 selective blocker offering the advantage of less bronchopulmonary and
probably less cardiac, central and metabolic side effects. In addition, it may
exert a protective effect on retinal neurones independent of i.o.t. lowering, possibly
by reducing Na+/Ca+ influx. However, it is less
efficacious in lowering i.o.t. than timolol, because ocular β receptors are
predominantly of the β2 subtype. Transient
stinging and burning in the eye is more common with it. Most ophthalmologists prefer
to start with betaxolol and change over to timolol (or a similar drug) only if
i.o.t. control is insufficient or there is local intolerance to betaxolol.
OPTIPRESS,
IOBET 0.5% eye drops; 1 drop in each eye BD.
Levobunolol It has been introduced as a once daily alternative to timolol. The ocular and systemic
effects are very similar to timolol except for longer duration of action.
BETAGAN 0.5%
ophthalmic soln., 1 drop OD.
Carteolol and Metipranolol are the other ocular β blockers.
2. α Adrenergic
agonists
Adrenaline Applied topically 0.5–1% Adr can lower i.o.t., but response is variable due to poor
corneal penetration. The i.o.t. reduction is due to increased uveoscleral
outflow and β2 receptor mediated
increased hydraulic conductivity of trabecular filtering cells. Reduction in
aqueous formation can result from α2 and α1 receptor activation
in ciliary body.
Adrenaline frequently
produces ocular smarting and vasoconstriction followed by reactive hyperemia.
It is not used now because of ocular intolerance and possible systemic effects.
Dipivefrine It is a prodrug of Adr; penetrates cornea and is hydrolysed by the esterases
present there into Adr. Though better tolerated and longer acting than Adr,
dipivefrine still produces significant ocular side effects. It is used only as
add on therapy in poorly controlled patients.
PROPINE 0.1% eye drop;
1 drop in each eye BD.
Apraclonidine It is a polar
clonidine congener which does not cross bloodbrain
barrier, but applied topically (0.5–1%) it lowers i.o.t. by ~25%. It decreases
aqueous production by primary α2 and subsidiary α1 action in the ciliary
body. Itching, lid dermatitis, follicular conjunctivitis, mydriasis, eyelid
retraction, dryness of mouth and nose are common side effects. Its use is
restricted to control of spikes of i.o.t. after laser trabeculoplasty or
iridotomy.
Brimonidine This recently introduced clonidine congener is more α2 selective and more
lipophilic than apraclonidine. It lowers i.o.t. by 20–27% by reducing aqueous
production and by increasing uveoscleral flow. Ocular side effects are similar
to but less frequent than with apraclonidine. Because of weaker α1 action, side effects
like mydriasis, eyelid retraction, conjunctival blanching—hyperemia are less
prominent, but dry mouth, sedation and small fall in BP have been noted.
Brimonidine is
indicated both for shortterm (prophylaxis of i.o.t. spikes post laser/post surgery)
as well as longterm use in glaucoma. It is a 3rd choice/add on drug only.
ALPHAGAN, IOBRIM 0.2%
eyedrops; 1 drop in each eye TDS.
3. Prostaglandin analogues
Low concentration of
PGF2α was found to lower i.o.t without inducing
ocular inflammation. It acts by increasing uveoscleral outflow, possibly by
increasing permeability of tissues in ciliary muscle or by an action on episcleral
vessels. An effect on trabecular outflow is also possible. Ciliary body COX2 is
down regulated in wide angle glaucoma indicating a physiological role of PG in
aqueous humor dynamics.
Latanoprost Instilled in the eye, this PGF2α derivative has shown
efficacy similar to timolol (i.o.t. reduction by 25–35%) and the effect is well
sustained over longterm. It reduces i.o.t. in normal pressure glaucoma also.
Though ocular irritation and pain are frequent, no systemic side effects are
reported. Blurring of vision, increased iris pigmentation, thickening and darkening
of eyelashes have occurred in some cases.
Because
of good efficacy, once daily application and absence of systemic complications,
PG analogues have become the first choice drugs in developed countries. High
cost limits their use in resource poor countries.
LACOMA,
XALATAN 0.005% eye drops, one drop in each eye OD in the evening; LACOMAT with
timolol 0.5% eye drops. (To be stored in cold)
Unoprostone, Travoprost and Bimatoprost are other ocular PG analogues.
4. Carbonic
anhydrase inhibitors
Acetazolamide Oral treatment with acetazolamide (0.25 g 6–12 hourly) reduces
aqueous formation by limiting generation of bicarbonate ion in the ciliary
epithelium. It is used to supplement ocular hypotensive drugs for short term
indications like angle closure, before and after ocular surgery/laser therapy.
Systemic side effects—paresthesia, anorexia, hypokalaemia, acidosis, malaise
and depression restrict longterm use to few cases in which target i.o.t. is not
achieved even by concurrent use of 2–3 topical drugs.
Dorzolamide (2% eyedrops TDS) It is a topically useful carbonic anhydrase inhibitor
developed to circumvent systemic side effects of acetazolamide. It lowers i.o.t.
by ~20%; somewhat less efficacious than timolol. Ocular stinging, burning, itching
and bitter taste are the side effects.
Dorzolamide is used
only as add on drug to topical β blockers/PG analogues, or when these drugs
are contraindicated.
DORTAS, DORZOX 2% eye
drops.
Brinzolamide is another ocular
carbonic anhydrase inhibitor.
5. Miotics
Till the 1970s topical pilocarpine and/or antiChEs were the standard antiglaucoma
drugs. However, because of several drawbacks, they are now used only as the last
option. In open angle glaucoma, they lower i.o.t. by increasing ciliary muscle
tone thereby improving patency of trabeculae.
The current approach
to treatment of open angle glaucoma can be summarized as—start monotherapy with
latanoprost or a topical β blocker; if target i.o.t. is not attained
either change over to the alternative drug or use both the above concurrently.
Brimonidine/dorzolamide/dipivefrine are used only when there are contraindications
to PG analogues/β blockers, or to supplement their action. Topical miotics and
oral acetazolamide are added only as the last resort.
B. Angle Closure (Narrow Angle, Acute Congestive) Glaucoma
It occurs in
individuals with a narrow iridocorneal angle and shallow anterior chamber. The
i.o.t. remains normal until an attack is precipitated, usually by mydriasis
(Fig. 10.3A,B). The i.o.t. rises rapidly to very high values (40–60 mmHg). It
is an emergent condition; failure to lower i.o.t. quickly may result in loss of
sight.
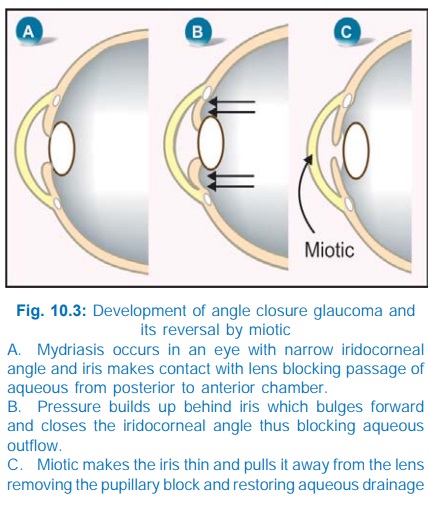
Vigorous therapy employing
various measures to reduce i.o.t. is instituted.
·
Hypertonic mannitol
(20%) 1.5–2 g/kg or glycerol (10%): infused i.v. decongest
the eye by osmotic action. A
retention enema of 50% glycerine is also some times used.
·
Acetazolamide: 0.5 g i.v. followed
by oral twice daily is started
concurrently.
·
Miotic: Once the i.o.t. starts
falling due to the above i.v.
therapy, pilocarpine 1–4% is instilled every 10 min initially and then at longer
intervals. Contraction of sphincter pupillae changes the direction of forces in
the iris to lessen its contact with the lens and spreads the iris mass
centrally → pupillary block is
removed and iridocorneal angle is freed (Fig. 10.3C). However, when i.o.t. is
very high, the iris muscle fails to respond to miotics; tension should be reduced
by other measures before miotics can act.
·
Topical β blocker: Timolol 0.5% is
instilled 12 hourly in addition.
·
Apraclonidine (1%)/latanoprost
0.005% instillation may be added.
Drugs
are used only to terminate the attack of angle closure glaucoma. Definitive
treatment is surgical or laser iridotomy. Few cases, who have chronic narrow
angle glaucoma, may be treated with a miotic/other ocular hypotensive drug for
long periods, but often surgery/laser therapy is ultimately required.
Related Topics
