Drug Therapy of Migraine
| Home | | Pharmacology |Chapter: Essential pharmacology : 5Hydroxytryptamine, Its Antagonists And Drug Therapy Of Migraine
Migraine is a mysterious disorder characterized by pulsating headache, usually restricted to one side, which comes in attacks lasting 4–48 hours and is often associated with nausea, vomiting, sensitivity to light and sound, flashes of light, vertigo, loose motions and other symptoms.
DRUG THERAPY OF MIGRAINE
Migraine is a mysterious disorder characterized by pulsating headache, usually restricted to one side, which comes in attacks lasting 4–48 hours and is often associated with nausea, vomiting, sensitivity to light and sound, flashes of light, vertigo, loose motions and other symptoms. Two major types are—migraine with aura (classical migraine) in which headache is preceded by visual or other neurological symptoms, and migraine without aura (common migraine). Pulsatile dilatation of certain large cranial vessels is the immediate cause of pain. The pathogenic mechanisms are not well understood. The Vascular theory holds that initial vasoconstriction or shunting of blood through carotid arteriovenous anastomoses produces cerebral ischaemia and starts the attack. The Neurogenic theory considers it to be a spreading depression of cortical electrical activity followed by vascular phenomena. Some triggering event appears to produce neurogenic inflammation of the affected blood vessel wall which is amplified by retrograde transmission in the afferent nerves and release of mediators like 5HT, neurokinin, substance P, calcitonin gene related peptide (CGRP), nitric oxide, etc.
Changes in blood/urinary levels of 5HT and its metabolites during migraine attack, its precipitation by 5HT releasers and efficacy of drugs having actions in the serotonergic system to prevent/abort/terminate migraine attacks suggests a pivotal role of 5HT in this disorder.
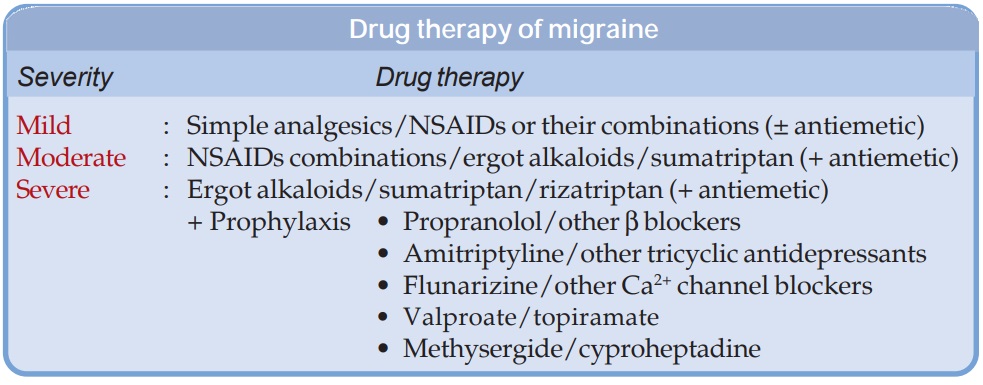
Drug therapy of migraine has to be individualized: severity and frequency of attacks and response of individual patients to drugs used earlier determine the choice. The strategy mostly adopted is summarized in the box.
Mild Migraine
Cases having fewer than one attack per month of throbbing but tolerable headache lasting upto 8 hours which does not incapacitate the individual may be classified as mild migraine.
1. Simple analgesics like paracetamol (0.5– 1 g) or aspirin (300–600 mg) taken at the first indication of an attack and repeated 4–6 hourly abort and suppress most mild attacks.
2. Nonsteroidal anti-inflammatory drugs (NSAIDs) and their combinations Drugs like ibuprofen (400–800 mg 8 hourly), naproxen (500 mg followed by 250 mg 8 hourly), diclofenac (50 mg 8 hourly), mephenamic acid (500 mg 8 hourly), indomethacin (50 mg 6–8 hourly) either alone or combined with paracetamol/codeine/diazepam or another sedative/diphenhydramine or another antihistaminic/caffeine are found more satisfactory by some patients. These drugs are more effective in migraine without aura, but certain patients of migraine with aura also prefer them over ergot alkaloids. Drugs are taken only till the attack passes off. Taken in the prodromal stage they also have a prophylactic effect, but longterm treatment on a regular schedule to ward off migraine attacks is not advised.
3. Antiemetics Gastric stasis occurs during migraine which delays absorption of oral drugs. Metoclopramide (10 mg oral/i.m.) is frequently used: relieves nausea, vomiting and gastric stasis. Domperidone (10–20 mg oral) and prochlorperazine (10–25 mg oral/i.m.) are also effective. Diphenhydramine or promethazine exert sedative as well as antiemetic action.
Moderate Migraine
Migraine may be labelled as moderate when the throbbing headache is more intense, lasts for 6–24 hours, nausea/vomiting and other features are more prominent and the patient is functionally impaired. One or more attacks occur per month.
Simple analgesics are usually not effective, but stronger NSAIDs or their combinations mentioned above are beneficial in many cases. The remaining are treated with an ergot preparation or sumatriptan. Antiemetics are almost regularly needed. Prophylactic therapy is advised only when attacks are more frequent than 2–3 per month.
Severe Migraine
These patients suffer 2–3 or more attacks per month of severe throbbing headache lasting 12–48 hours, often accompanied by vertigo, vomiting and other symptoms; the subject is grossly incapacitated during the attack.
Analgesics/NSAIDs and their combinations usually donot afford adequate relief—specific drugs like ergot alkaloids/sumatriptan have to be prescribed along with antiemetics. Prophylactic regimens lasting 6 months or more are recommended.
Ergotamine It is the most effective ergot alkaloid for migraine. Given early in attack, relief is often dramatic and lower doses suffice, but when pain has become severe—larger doses are needed and control may be achieved only after few hours. Oral/sublingual route is preferred, 1 mg is given at half hour intervals till relief is obtained or a total of 6 mg is given. Parenteral administration, though rapid in action is more hazardous.
Ergotamine acts by constricting the dilated cranial vessels and/or by specific constriction of carotid AV shunt channels. Ergotamine and DHE have also been shown to reduce neurogenic inflammation and leakage of plasma in duramater that occurs due to retrograde stimulation of perivascular afferent nerves. These actions appear to be mediated through partial agonismat 5HT1B/1D receptors in and around cranial vessels.
Dihydroergotamine (DHE) It is nearly as effective as ergotamine and preferred for parenteral administration because injected DHE is less hazardous.
Because of erratic oral absorption, frequent side effects, especially nausea and vomiting, and availability of triptans, ergot preparations are not preferred now, except for considerations of cost.
Ergot alkaloids have no prophylactic value: regular use is not justified—may itself produce a dull background headache and an attack may be precipitated on discontinuation. Caffeine 100 mg taken with ergotamine enhances its absorption from oral and rectal routes and adds to the cranial vasoconstricting action. Many combination preparations are available.
MIGRANIL: Ergotamine 1 mg, caffeine 100 mg, belladonna dry ext 10 mg, paracetamol 250 mg tab. MIGRIL: Ergotamine 2 mg, caffeine 100 mg, cyclizine 50 mg tab.
VASOGRAIN: Ergotamine 1 mg, caffeine 100 mg, paracetamol 250 mg, prochlorperazine 2.5 mg tab. ERGOPHEN: Ergotamine 0.3 mg, belladonna dry ext. 10 mg, phenobarbitone 20 mg tab.
Selective 5HT1B/1D Agonists
These are a new class of antimigraine drugs that selectively activate 5HT1B/1D receptors, and are called ‘triptans’. Currently, they are the preferred drugs for patients who fail to respond to analgesics. Ergot alkaloids are now required only in few cases. Because these drugs have been designed to act on the same subtype of 5HT receptor, pharmacodynamic differences among them are minor, but there are significant pharmacokinetic differences. All have higher oral bioavailability than sumatriptan. Fewer headache recurrences in an attack are reported with naratriptan and frovatriptan due to their longer t½, but may be slower in affording initial pain relief.
Sumatriptan It is the first selective 5HT1B/1D receptor agonist; activates other subtypes of 5HT1 receptors only at very high concentrations, and does not interact with 5HT2, 5HT3, 5HT47, or β adrenergic, dopaminergic, cholinergic or GABA receptors. Administered at the onset of an attack of migraine, sumatriptan is as effective and better tolerated than ergotamine. About 3/4 patients obtain complete/significant relief within 2–3 hours. However, recurrence of headache within 24 hr has been noted in 20–40% patients, probably due to short t½ of sumatriptan. It tends to suppress nausea and vomiting of migraine, while ergotamine accentuates these symptoms.
The antimigraine activity of sumatriptan has been ascribed to 5HT1B/1D receptor mediated constriction of dilated cranial extracerebral blood vessels, especially the arteriovenous shunts in the carotid artery, which express 5HT1B/1D receptors. Dilatation of these shunt vessels during migraine attack is believed to divert blood flow away from brain parenchyma. In addition it can reduce 5HT and inflammatory neuropeptide release around the affected vessels as well as extravasation of plasma proteins across dural vessels. Like ergotamine, the triptans have been found to suppress neurogenic inflammation of cranial vessels. Suppression of impulse transmission in the trigeminovascular system has also been implicated.
Pharmacokinetics:
Sumatriptan is absorbed rapidly and completely after s.c. injection. Oral bioavailability averages 15%. It is rapidly metabolized by MAOA isoenzyme and metabolites are excreted in urine; elimination t½ is ~2 hours.
Side Effects: to sumatriptan are usually mild. Tightness in head and chest, feeling of heat and other paresthesias in limbs, dizziness, weakness are short lasting, but dose related side effects.
These are more common after s.c. injection, which is painful. Slight rise in BP occurs, but has little clinical relevance, because sumatriptan is not a drug for regular use. Bradycardia, coronary vasospasm and risk of myocardial infarction are the serious, but infrequent adverse effects. Few cases of sudden death have been ascribed to sumatriptan. Seizures and hypersensitivity reactions are rare.
Contraindications: are in patients with ischaemic heart disease, hypertension, epilepsy, hepatic or renal impairment and during pregnancy. Patients should be cautioned not to drive.
Sumatriptan and ergotamine should not be administered within 24 hours of each other. Interaction with 5HT uptake inhibitors, MAO inhibitors and lithium has been reported.
Dose: 50–100 mg oral at the onset of migraine attack, may be repeated once within 24 hours if required. Those not responding to the first dose should not be given the second dose. It is the only triptan available for parenteral use; 6 mg s.c. may be given to patients who cannot take the drug orally or in whom the pain develops very rapidly; acts in 10–20 min and is more consistently effective.
MIGRATAN, 50, 100 mg tabs, SUMINAT 25, 50, 100 mg tab, 60 mg/5 ml inj; SUMITREX 25, 50, 100 mg tab, 6 mg/0.5 ml inj.
Rizatriptan: This congener of sumatriptan is more potent, has higher oral bioavailability with slightly faster onset of action.
Dose: 10 mg; repeat once after 2 hr (if required).
RIZACT 5, 10 mg tab.
Naratriptan, Zolmitriptan, Almotriptan, Frovatriptan and Eletriptan are other triptans used in some countries.
Features of some triptans are compared in the box.
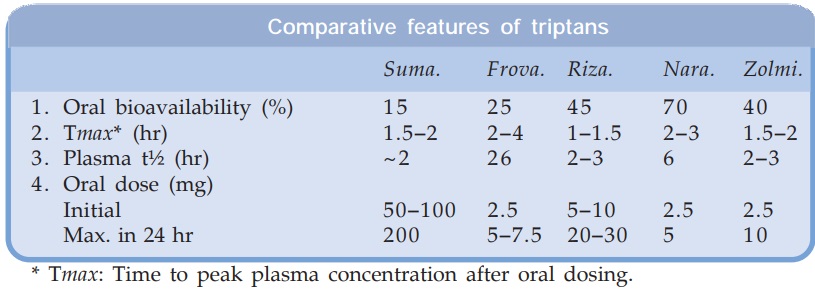
* Tmax: Time to peak plasma concentration after oral dosing.
Prophylaxis Of Migraine
Regular medication to reduce the frequency and/or severity of attacks is recommended for moderate to severe migraine when 2–3 or more attacks occur per month. Diverse classes of drugs are used but none is effective in all cases, and none abolishes the attacks totally. It may be prudent to discontinue pophylaxis every 6 months to check whether its continuation is needed or not. It is important to avoid the precipitating factor(s).
Β-Adrenergic blockers Propranolol is the most commonly used drug: reduces frequency as well as severity of attacks in upto 70% patients. Effect is generally seen in 4 weeks and is sustained during prolonged therapy. The starting dose is 40 mg BD, which may be increased upto 160 mg BD if required. The mechanism of action is not clear; that it is due to β adrenergic blockade has been questioned. Other nonselective (timolol) and β1 selective (metoprolol, atenolol) agents are also effective, but pindolol and others having intrinsic sympathomimetic action are not useful.
Tricyclic antidepressants Many tricyclic compounds of which amitriptyline has been most extensively tried (25–50 mg at bed time) reduce migraine attacks. It is effective in many patients but produces more side effects than propranolol. It is not known whether its 5HT (and other monoamine) uptake blocking property is causally related to the prophylactic effect. The antimigraine effect is independent of antidepressant property, but this class of drugs are better suited for patients who also suffer from depression.
Calcium channel blockers Verapamil was found to reduce migraine attacks, but was judged inferior to propranolol. Flunarizine is a relatively weak Ca2+ channel blocker that also inhibits Na+ channels. It is claimed to be as effective as propranolol, but convincing proof is lacking. Frequency of attacks is often reduced, but effect on intensity and duration of attacks is less well documented. It is claimed to be a cerebroselective Ca2+ channel blocker; may benefit migraine by reducing intracellular Ca2+ overload due to brain hypoxia and other causes. Side effects are sedation, constipation, dry mouth, hypotension, flushing, weight gain and rarely extrapyramidal symptoms.
Dose: 10–20 mg OD, children 5 mg OD, NOMIGRAIN, FLUNARIN 5 mg, 10 mg caps/tab.
Anticonvulsants Valproic acid (400–1200 mg/day) and gabapentin (300–1200 mg/day) have some prophylactic effect in migraine. The newer drug topiramate has recently been approved for migrain prophylaxis. A 50% reduction in the number of attacks in half of the patients was noted in 2 randomized trials. Start with 25 mg OD and gradually increase to 50 mg OD or BD. Efficacy of anticonvulsants in migraine is lower than that of β blockers. They are indicated in patients refractory to other drugs or when propranolol is contraindicated.
5HT antagonists The prophylactic effect of methysergide and cyproheptadine is less impressive than β blockers. They are seldom used now for migraine.
Related Topics
