Connective Tissues
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Levels of Organization : Tissues
Components of Connective Tissues, Connective Tissue Cells, Connective Tissue Fibers
Types of Tissues
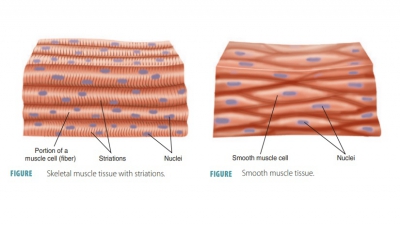
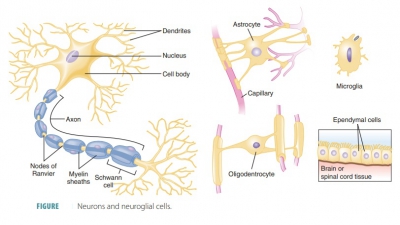
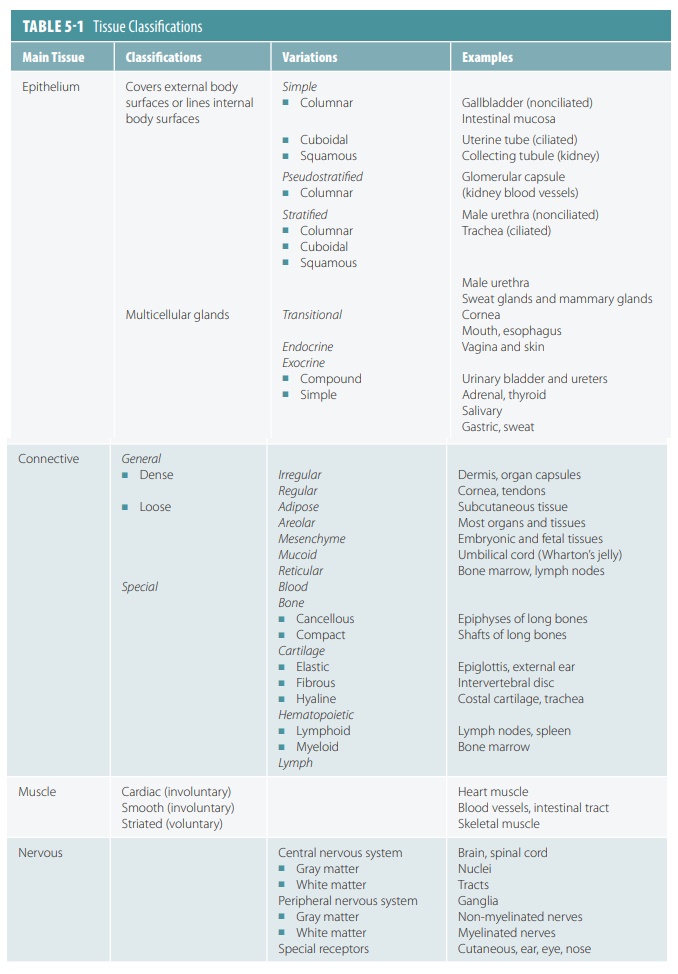
The human body is primarily made up of four major types of tissues: epithelial, connective, muscle, and nervous. Epithelial tissues cover body surfaces, cover and line internal organs, and make up the glands. Connective tissues are widely distributed throughout the body, filling internal spaces, and func-tion to bind, support, and protect body structures. Muscle tissues are specialized for contraction and include the skeletal muscles of the body, the heart, and the muscular walls of hollow organs. Skeletal muscles are attached to bones and are used for movement of the body. Nervous tissues carry information from one part of the body to another via electrical impulses. They are found in the brain, spinal cord, and nerves (TABLE 5-1).
The human body is primarily made up of four major types of tissues:
1. epithelial,
2. connective
3. muscle, and
4. nervous.
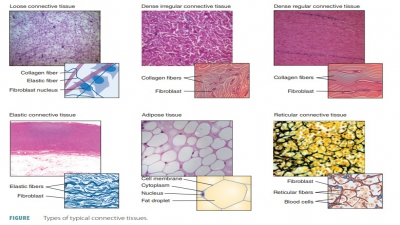
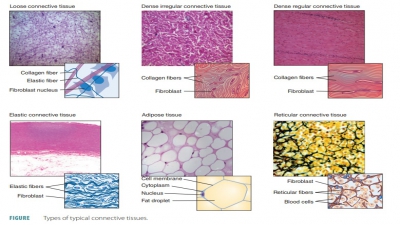
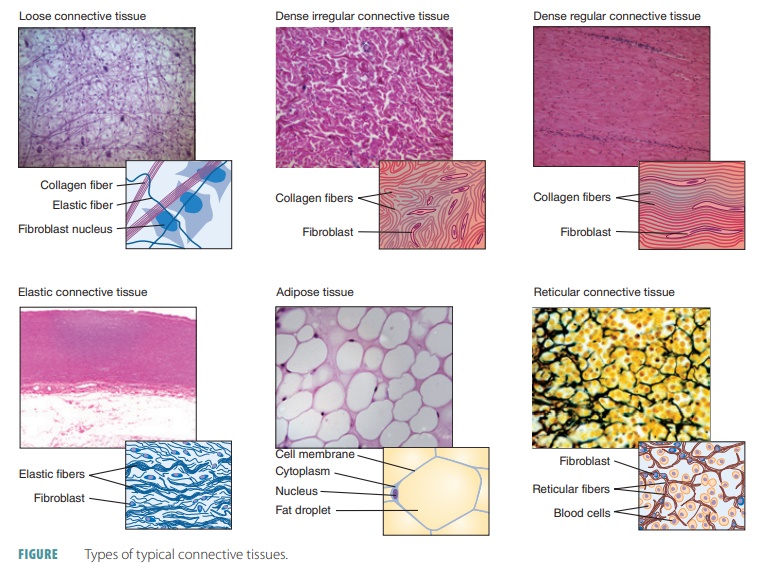
Connective Tissues
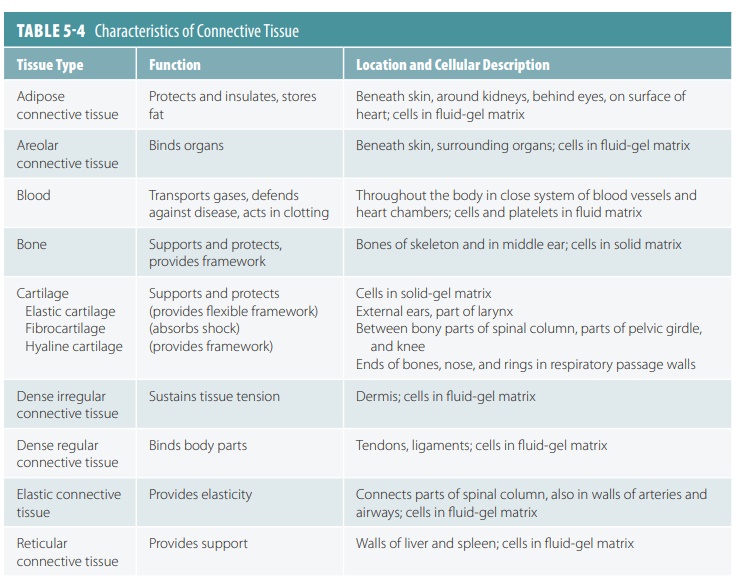
The cells that make up connective tissues are farther apart than those of epithelial tissues. These tissues bind body structures, provide support and protection, cre-ate frameworks, fill body spaces, store fat for reserve fuel, insulate the body, produce blood cells, transport fluids and dissolved materials, repair damaged tissues, and protect the body from infection. Connective tis-sues usually contain a large amount of matrix. This matrix is composed of fibers and ground substance, which is clear and colorless.
Many connective tissues are extremely vascular and contain sensory receptors able to detect tempera-ture, pain, pressure, and other stimuli. The specific functions of connective tissues include:
■■ Defense of the body from invading pathogens
■■ Establishment of a structural framework
■■ Protection of delicate organs
■■ Storing energy, primarily as triglycerides
■■ Interconnecting, supporting, and surrounding other tissue types
■■ Transporting dissolved materials and fluids
Components of Connective Tissues
Connective tissues vary greatly in appearance and function, but have three basic components:
■■ Specialized cells
■■ Extracellular protein fibers
■■ A fluid known as ground substance, which is the unstructured material filling spaces between cells and containing fibers. It is made up of cell adhesion proteins, interstitial fluid, and proteoglycans. Cell adhesion proteins include fibronectin, laminin, and others. They attach connective tissue cells to elements of the matrix. Proteoglycans have a protein core that is attached to glycosaminoglycans.
These are strand-like polysaccharides that include chondroitin sulfate and hyaluronic acid, emerging from the core like spikes.
Together, the extracellular protein fibers and ground substance constitute the matrix, which sur-rounds the cells. Although cells make up most epithe-lial tissue, the matrix usually accounts for most of the connective tissue. Connective tissues vary in amount per organ, but overall are the most widely distributed and abundant of primary body tissues.
Connective Tissue Cells
Most connective tissue cells divide, have good blood supply, and require large amounts of nourishment. Connective tissues include those of bone, cartilage, and fat. Connective tissues contain different types of cells, including those that are fixed or wander-ing. Connective tissue cells exist in both immature (undifferentiated) and mature forms. Immature cells are described using the suffix -blast, which means “forming.” These actively mitotic cells secrete the ground substance and the fibers that make up their portion of the matrix. The most common type of fixed cell is the star-shaped fibroblast, which pro-duces fibers via protein secretion into the extracellu-lar matrix. Fibroblasts also secrete a polysaccharide derivative known as hyaluronan, which helps lock epithelial cells together. This substance interacts with extracellular fluid and proteins to form proteo-glycans, which make the ground substance viscous.
Bacteria and other pathogens cannot move through the ground substance easily, making it easier for phagocytes to engulf them.
Fibroblasts also secrete protein subunits that even-tually join to form large extracellular fibers. Additional cells include chondroblasts (which produce cartilage) and osteoblasts (which produce bone). Blood cells are produced by hematopoietic stem cells, which are not located in the blood and do not make the matrix of the blood, which is known as the plasma.
Fibrocytes
Fibrocytes differentiate from fibroblasts. They are the second most common fixed cells in connective tissue proper. Fibrocytes have a spindle shape and maintain connective tissue fibers.
Mast Cells
Mast cells are distributed throughout connective tissues, usually near blood vessels, and release both heparin (to prevent blood clotting) and histamine (for the inflammatory and allergic response). Mast cells are oval shaped and cause the inflammatory response against foreign microorganisms when they are detected. The cytoplasm of mast cells contains secretory granules of heparin, histamine, proteases, and various other enzymes. Granules of histamine and heparin are also found in basophils, which are white blood cells that enter damaged tissues and enhance the inflammatory process.
Macrophages
Macrophages are responsible for phagocytosis, are large and irregularly shaped, and are able to ingest many different foreign materials, including entire bacteria, dust particles, and dead tissue cells. They are large, amoeboid cells that are not extremely abundant. Macrophages are the primary cellular components of the immune system, releasing chemicals that not only activate in this system, but also attract many more macrophages and other cells involved in the defense of tissues. They are found throughout the bone marrow, loose connective tissue, and lymphatic tissue. Fixed macrophages spend long amounts of time inside tis-sues. Free macrophages migrate quickly through tis-sues, providing a first line of defense that is assisted by more free macrophages and other specialized cells.
Lymphocytes
Lymphocytes move through the body’s tissues, increasing in number dramatically where tissue dam-age occurs. Certain lymphocytes develop into plasma cells. These cells produce antibodies, which help to defend the body against disease.
Microphages
Microphages are phagocytes that are usually found in small numbers in the connective tissues. These white blood cells include neutrophils and eosinophils. How-ever, when injury or infection occurs, many micro-phages are attracted to the site because of chemicals released by macrophages and mast cells.
Melanocytes
Melanocytes synthesize and store melanin, which is the brown pigment that causes tissues to have a dark color. Melanocytes are commonly found in the skin’s epithelium, where they are important for determining skin color. Melanocytes are also common in the der-mis, vagina, and in the connective tissues of the eyes. The number of melanocytes that are present differs between individuals and between body regions.
Connective Tissue Fibers
Connective tissue fibers provide support. Fibroblasts produce three connective tissue fibers: collagenous, elastic, and reticular fibers.
Collagenous Fibers
Collagenous fibers are important for body parts that hold structures together (ligaments and tendons). They are also called dense connective tissue or white fibers, and are long and straight. They are the strongest and most abundant type of connective tissue fibers and do not have branches. Constructed mostly of the fibrous protein collagen, these fibers are very tough and resist being pulled apart, providing tensile strength to the matrix. If steel fibers existed at the same size, the collagenous fibers would be stronger. The fibers are formed as the extracellular space receives secreted col-lagen molecules, which assemble into fibrils that have a cross-linked organization. These are then bundled into thicker collagen fibers that are wound like strands in a rope. Tendons, connecting skeletal muscles to bones, are made up almost completely of collagen fibers. Ligaments, which connect bones to each other, are also made of collagenous fibers. Tendons and lig-aments are less likely to snap when stress is applied in comparison to bones.
Elastic Fibers
Elastic fibers are common in body parts that are often stretched such as the vocal cords, large blood vessel walls (e.g., those leaving the heart), lungs, and skin. They are composed of a protein called elastin and are also called yellow fibers. Elastic fibers are long, wavy, and thin. In the extracellular matrix, they form branch-ing networks. Elastin allows these fibers to stretch and then recoil, which then causes the connective tissue to return to its normal length and shape. Elastic ligaments are mostly made up of elastic fibers. Though these liga-ments are rare in the body, they are important, such as when they interconnect the spinal vertebrae.
Reticular Fibers
Reticular fibers form delicate supporting networks in the spleen and other tissues. They are short and fine in structure, made up of collagen, but in a different form than the collagenous fibers. However, the reticular fibers are continuous with the collagenous fibers. They form thin, delicately branched networks that extensively sur-round small blood vessels, providing soft organ tissue support. They are highly abundant where connective tissue meets other types of tissue, such as the epithelial tissue basement membranes and in the areas that sur-round capillaries. Here, the reticular fibers form net-like structures that provide more “give and take” than larger collagenous fibers are able to provide. The interwoven network of reticular fibers or stroma stabilizes the posi-tions of functional cells known as parenchyma. These are found in the liver and other organs.

1. List the components of connective tissues.
2. Explain the three connective tissue fibers produced by fibroblasts.
3. What chemical substances do mast cells secrete?