Comments on the use of Hypolipidaemic Drugs
| Home | | Pharmacology |Chapter: Essential pharmacology : Hypolipidaemic Drugs And Plasma Expanders
Raised plasma CH is a major risk factor for coronary artery disease (CAD); higher the CH level, greater is the risk of CAD. Abundant data has confirmed that lowering the level of LDL-CH, when the same is high, results in decreased incidence of cardiovascular mortality and morbidity.
COMMENTS ON THE USE OF HYPOLIPIDAEMIC DRUGS
Raised plasma CH is a
major risk factor for coronary artery disease (CAD); higher the CH level,
greater is the risk of CAD. Abundant data has confirmed that lowering the level
of LDL-CH, when the same is high, results in decreased incidence of
cardiovascular mortality and morbidity. More recent evidence (HPS, 2002; ASCOT-LLA,
2003 studies) has indicated that prophylactic use of a statin in
CAD/hypertensive patients even with average or lower than average CH levels
lowers coronary and stroke events. With the availability of effective, well
tolerated and safe hypolipidaemic drugs, it has become a standard practice to
prescribe statin therapy after an acute coronary event irrespective of lipid
levels. Evidence that elevated plasma TG level or low plasma HDL–CH level poses
independent high risk of CAD and stroke is also now quite strong.
Whereas raised LDL-CH
is atherogenic, a higher HDLCH level is either itself protective or indicates a
low atherogenic state.
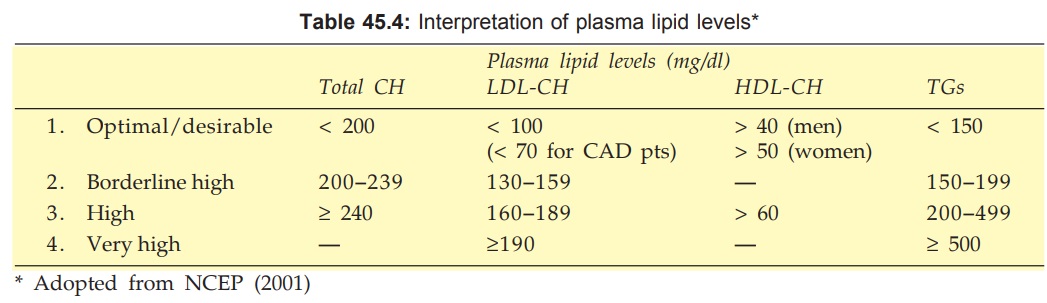
The US National Cholesterol
Education Programme (NCEP) in its third report (2001) delineated the optimal
levels of plasma lipids and various grades of hyperlipidaemias (Table 45.4) and
revised the guidelines for use of hypolipidaemic drugs (Adult Treatment Panel
III or ATP III).
Subsequently, the
results of some large randomized controlled trials like HPS (2002), ASCOTLLA
(2003), PROVEIT (2004) became available and necessitated further revision of
the treatment guidelines. A 2004 revision of the ATP III guidelines has been
published (Grundy et al, 2004). The
salient features of these guidelines are incorporated in the following summary.
Lifestyle
modification, such as low fat, low cholesterol diet, limitation of saturated
and transfats, regular exercise, body weight control, smoking cessation,
restriction of alcohol are the primary approach, whether drugs are used or not.
Risk Factors For
Coronary Artery Disease*
·
Men > 45 years, women > 55 years
·
Family history of MI/sudden cardiac death
before 55 year (men), 65 year (women) age in first degree relative
·
Smoking
·
Hypertension (BP > 140/90 or use of antihypertensive
medication)
·
Diabetes mellitus£
·
Low HDLCH (< 40 mg/dl in men, < 50 mg/dl
in women)
·
High LDL-CH (≥ 160 mg/dl) or total
CH ≥ 240 mg/dl
·
Obesity (BMI > 25 Kg/m2)† or waist > 40″ (men), >35″ (women)
The decision to
prescribe hypolipidaemic drugs depends not only on the LDL-CH level and the
type of lipid abnormality, but also on associated CAD risk factor(s) or existing
CAD or its equivalent like diabetes, peripheral/cerebral vascular disease, etc.
in an individual patient (see box).
Treatment Based on LDL-CH Level
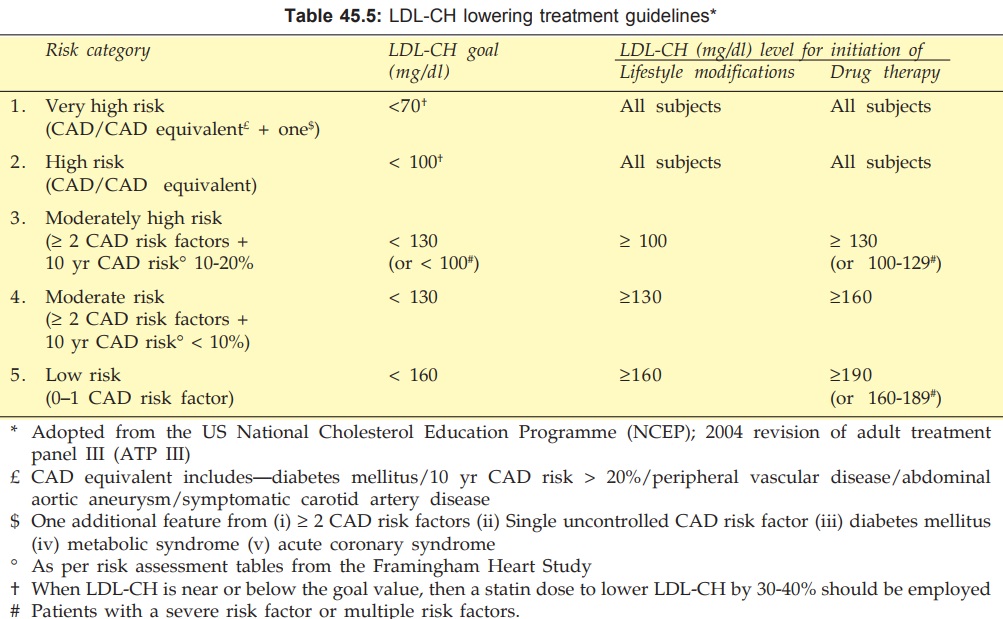
The revised NCEPATP III guidelines are summarized in Table
45.5. All subjects should receive statin (or statin-based combination) therapy
if LDL-CH is ≥ 190 mg/dl. The dose should be titrated to achieve the goal LDL-CH
level or 3040% reduction, whichever is lower (this degree of lipid lowering has
been found to yield optimum prognostic benefit). For subjects who already have
CAD or CAD equivalent, there is no lower threshold LDL-CH level; all subjects
should receive lipid lowering drug. Though, LDL-CH value upto 100 mg/dl is
considered optimal for non-CAD subjects, the goal for CAD patients has been lowered
to 70 mg/dl. These decisions have been based on the findings of recent studies
which have compared mortality as well as CAD and stroke prevention benefits of
standard vs intensive CH lowering
regimens. Also the criteria for grading the cardiovascular disease risk as
‘very high’ to ‘low’ have been defined, and threshold as well as goal LDL-CH
levels have been demarkated for each category of risk.
The primary drugs to lower LDL-CH are statins. Statin therapy should
be commenced at low dose. In case of inadequate response, dose should be
doubled at 6 week intervals (till max doses reached) and/or another drug
(fibrate/ nicotinic acid/ezetimibe) should be added to achieve the target LDL-CH
level.
Treatment Of Low HDL-CH Level
Epidemiological data has shown that most patients with
premature CAD have low HDLCH level. The total CH: HDLCH ratio has been
recognized as a more important determinant of CAD risk. While a ratio of ≤ 3.5 is considered
desirable, a ratio of > 4.5 is associated with higher risk. Recent trials have
shown that statin therapy reduces CAD endpoints in subjects with low HDLCH even
though LDL-CH may be in the normal range. Most low HDLCH subjects have metabolic
syndrome (obesity, hyper-triglyceridaemia, insulin resistance/diabetes, hypertension).
Therapy directed towards components of this syndrome often helps to normalise
HDLCH. NO. In addition to these measures, the primary approach of therapy in
subjects with low HDLCH is to reduce LDL-CH to the target level as per their LDL-CH
risk category or to achieve a total CH: HDLCH ratio of ≤ 3.5, whichever is
more intensive. None of the currently available lipid modifying drugs has a
marked effect to raise HDLCH, but nicotinic acid has the highest efficacy
followed by fibrates. These drugs may be usefully combined with the statin,
watching for signs of myositis.
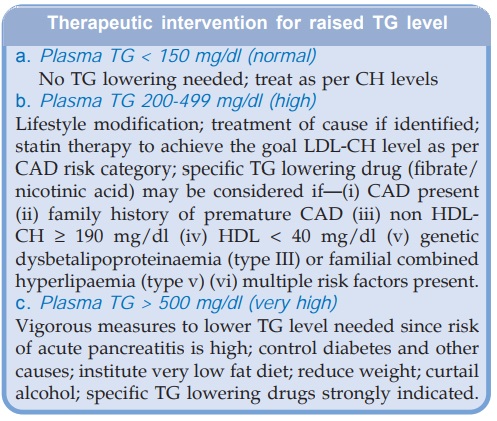
Treatment Of Raised TG Level:
On the basis of meta-analysis of
studies, the NCEP have recognized elevated TGs to be an independent CAD risk
factor. Treatment strategy for hyper-triglyceridaemia depends on its cause
(obesity, physical inactivity, smoking, alcohol, high carbohydrate diet,
diabetes, renal failure, drugs like corticosteroids, estrogens, high dose β blockers and genetic
disorders) and its severity. Initial treatment is directed to achieving the
target LDL-CH level appropriate for the patient’s CAD risk category (by using a
statin). This may itself lower the TG level. The primary TG lowering drugs are
fibrates and nicotinic acid. In case of failure to reduce serum TG to < 200
mg/dl, a fibrate (preferably fenofibrate) or nicotinic acid may be added to the
statin regimen, with extra vigilance to guard against the increased risk of
myopathy.
Related Topics
