Chronic Gout
| Home | | Pharmacology |Chapter: Essential pharmacology : Antirheumatoid and Antigout Drugs
When pain and stiffness persist in a joint between attacks, gout has become chronic. Other cardinal features are hyperuricaemia, tophi (chalklike stones under the skin in pinna, eyelids, nose, around joints and other places) and urate stones in the kidney. Chronic gouty arthritis may cause progressive disability and permanent deformities.
CHRONIC GOUT
When pain and stiffness persist in a joint between attacks, gout has become chronic. Other cardinal features are hyperuricaemia, tophi (chalklike stones under the skin in pinna, eyelids, nose, around joints and other places) and urate stones in the kidney. Chronic gouty arthritis may cause progressive disability and permanent deformities.
A. URICOSURIC DRUGS
1. Probenecid
It is a highly lipid soluble organic acid developed in 1951 to inhibit renal tubular secretion of penicillin so that its duration of action could be prolonged. It competitively blocks active transport of organic acids by OATP at all sites; that in renal tubules being the most prominent. This transport is bidirectional: net effect depends on whether secretion or reabsorption of the particular organic acid is quantitatively more important, e.g.:
· Penicillin is predominantly secreted by the proximal tubules, its reabsorption is minimal. Net effect of probenecid is inhibition of excretion; more sustained blood levels are achieved.
· Uric acid is largely reabsorbed by active transport, while less of it is secreted; only 1/10th of filtered load is excreted in urine. Probenecid, therefore, promotes its excretion and reduces its blood level.
Probenecid does not have any other significant pharmacological action; it is neither analgesic nor anti-inflammatory.
Interactions
i. In addition to penicillins, probenecid inhibits the urinary excretion of cephalosporins, sulfonamides, Mtx and indomethacin.
ii. It inhibits biliary excretion of rifampicin. Pyrazinamide and ethambutol may interfere with uricosuric action of probenecid.
iii. Probenecid inhibits tubular secretion of nitrofurantoin which may not attain antibacterial concentration in urine.
iv. Salicylates block uricosuric action of probenecid.
Pharmacokinetics
Probenecid is completely absorbed orally; 90% plasma protein bound: partly conjugated in liver and excreted by the kidney; plasma t½ is 8–10 hours.
Adverse Effects
Probenecid is generally well tolerated.
Dispepsia is the most common side effect (upto 25% incidence with high doses). It should be used cautiously in peptic ulcer patients. Rashes and other hypersensitivity phenomena are rare. Toxic doses cause convulsions and respiratory failure.
Uses
1. Chronic gout and hyperuricaemia: Probenecid is a second line/adjuvant drug to allopurinol. Started at 0.25 g BD and increased to 0.5 g BD, it gradually lowers blood urate level; arthritis, tophi and other lesions may take months to resolve. Colchicine/NSAID cover is advised during the initial 1–2 months to avoid precipitation of acute gout.
Probenecid and other uricosurics are ineffective in the presence of renal insufficiency (serum creatinine > 2 mg/dl). Plenty of fluids should be given with probenecid to avoid urate crystallization in urinary tract.
2. Probenecid is also used to prolong penicillin or ampicillin action by enhancing and sustaining their blood levels, e.g. in gonorrhoea, SABE.
BENEMID, BENCID 0.5 g tab.
2. Sulfinpyrazone
It is a pyrazolone derivative related to phenylbutazone having consistent uricosuric action, but is neither analgesic nor anti-inflammatory. At the usual therapeutic doses, it inhibits tubular reabsorption of uric acid, but smaller doses can decrease urate excretion as do small doses of probenecid. Its uricosuric action is additive with probenecid but antagonised by salicylates. It inhibits platelet aggregation.
Pharmacokinetics
Sulfinpyrazone is well absorbed orally; 98% plasma protein bound—displacement interactions can occur. Excretion is fairly rapid, mainly by active secretion in proximal tubule. Uricosuric action of a single dose lasts for 6–10 hours.
Sulfinpyrazone inhibits metabolism of sulfonylureas and warfarin.
Adverse effects
Gastric irritation is the most common side effect—contraindicated in patients with peptic ulcer.
Rashes and other hypersensitivity reactions are uncommon.
Unlike phenylbutazone, it does not produce fluid retention or blood dyscrasias.
Uses
In chronic gout, the results are comparable to probenecid; same precautions should be exercised. Start with 100–200 mg BD, gradually
increase according to response, maximal dose 800 mg/day.
ANTURANE, ARTIRAN 200 mg cap.
Benzbromarone is another uricosuric drug marketed in Europe, but not in India.
B. URIC ACID SYNTHESIS INHIBITOR
Allopurinol
This hypoxanthine analogue was synthesized as a purine antimetabolite for cancer chemotherapy. However, it had no antineoplastic activity but was a substrate as well as inhibitor of xanthine oxidase, the enzyme responsible for uric acid synthesis (Fig. 15.1).
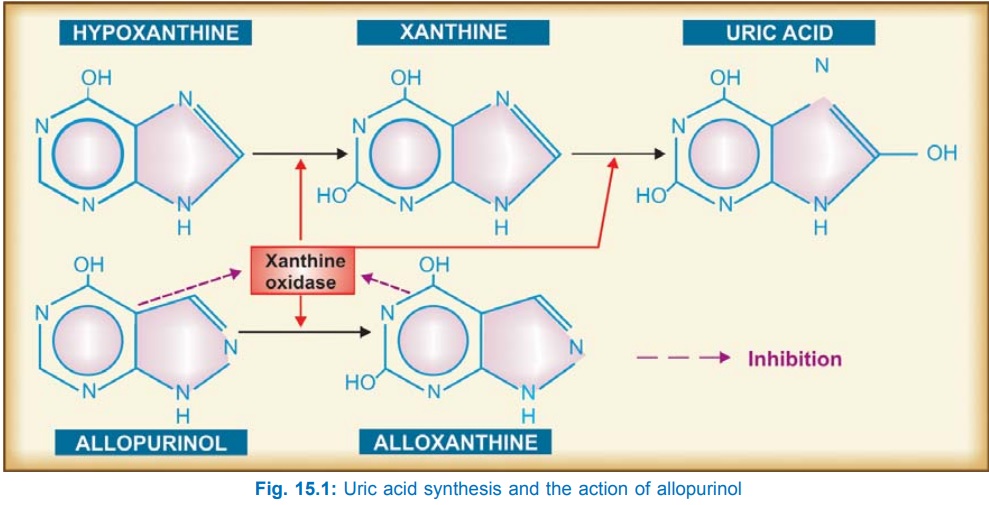
Allopurinol itself is a short acting (t½ 2 hrs) competitive inhibitor of xanthine oxidase, but its major metabolite alloxanthine (oxypurine) is a long acting (t½ 24 hrs) and noncompetitive inhibitor— primarily responsible for uric acid synthesis inhibition in vivo. During allopurinol administration, plasma concentration of uric acid is reduced and that of hypoxanthine and xanthine is somewhat increased. In place of uric acid alone, all 3 oxipurines are excreted in urine. Since xanthine and hypoxanthine are more soluble, have a higher renal clearance than that of uric acid and each has its individual solubility, precipitation and crystallization in tissues and urine does not occur.
Because of raised levels of xanthine and hypoxanthine, some feedback inhibition of de novo purine synthesis and reutilization of metabolically derived purine also occurs.
Pharmacokinetics
About 80% of orally administered allopurinol is absorbed. It is not bound to plasma proteins; metabolized largely to alloxanthine. During chronic medication, it inhibits its own metabolism and about 1/3rd is excreted unchanged, the rest as alloxanthine.
Interactions
a) Allopurinol inhibits the degradation of 6mercaptopurine and azathioprine: their doses should be reduced to 1/3rd, but not that of thioguanine, because it follows a different metabolic path (Smethylation).
b) Probenecid given with allopurinol has complex interaction; while probenecid shortens t½ of alloxanthine, allopurinol prolongs t½ of probenecid.
c) Allopurinol can potentiate warfarin and theophylline by inhibiting their metabolism.
d) A higher incidence of skin rashes has been reported when ampicillin is given to patients on allopurinol.
e) Iron therapy is not recommended during allopurinol treatment. The exact nature of interaction is not known, but interference with mobilization of hepatic iron stores is suggested.
Adverse Effects
These are uncommon. Hypersensitivity reaction consisting of rashes, fever, malaise and muscle pain is the most frequent. It subsides on stopping the drug. Renal impairment increases the incidence of rashes and other reactions to allopurinol.
Stevens-Johnson syndrome is a rare but serious risk.
Gastric irritation, headache, nausea and dizziness are infrequent; do not need withdrawal. Liver damage is rare.
Precautions And Contraindications
Liberal fluid intake is advocated during allopurinol therapy.
It is contraindicated in hypersensitive patients, during pregnancy and lactation.
It should be cautiously used in the elderly, children and in kidney or liver disease.
Uses
Allopurinol is the first choice drug in chronic gout. It can be used in both over producers and under excretors of uric acid, particularly more severe cases, with tophi or nephropathy. Uricosurics are infrequently used in India; they are less effective when g.f.r. is low and are inappropriate in stone formers. The two classes of drugs can also be used together when the body load of urate is large.
With long term allopurinol therapy, tophi gradually disappear and nephropathy is halted, even reversed.
Secondary hyperuricaemia due to cancer chemotherapy/radiation/thiazides or other drugs: can be controlled by allopurinol. It can even be used prophylactically in these situations.
To potentiate 6-mercaptopurine or azathioprine in cancer chemotherapy and immunosuppressant therapy.
Dose: Start with 100 mg OD, gradually increase to maintenance dose of 300 mg/day; maximum 600 mg/day.
ZYLORIC 100, 300 mg tabs., ZYLOPRIM, CIPLORIC 100 mg cap.
Caution
Allopurinol as well as uricosurics should not be started during acute attack of gout. During the initial 1–2 months of treatment with these drugs, attacks of acute gout are more common—probably due to fluctuating plasma urate levels favouring intermittent solubilization and recrystallization in joints; cover with NSAIDs/colchicine may be provided.
Kalaazar
Allopurinol inhibits Leishmania by altering its purine metabolism. It is used as adjuvant to sodium stibogluconate in resistant kalaazar cases (see Ch. No. 60).
Related Topics
