Cephalosporins
| Home | | Pharmacology |Chapter: Essential pharmacology : Betalactam Antibiotics
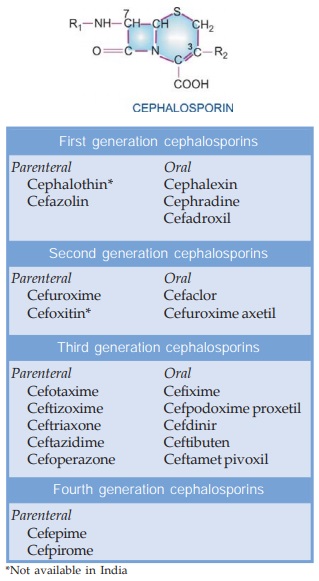
These are a group of semisynthetic antibiotics derived from ‘cephalosporin-C’ obtained from a fungus Cephalosporium. They are chemically related to penicillins; the nucleus consists of a βlactam ring fused to a dihydrothiazine ring.
CEPHALOSPORINS
These are a group of
semisynthetic antibiotics derived from ‘cephalosporin-C’ obtained from a fungus
Cephalosporium. They are chemically
related to penicillins; the nucleus consists of a βlactam ring fused to a
dihydrothiazine ring, (7-aminocephalosporanic acid). By addition of
different side chains at position 7 of βlactam ring (altering
spectrum of activity) and at position 3 of dihydrothiazine ring (affecting
pharmacokinetics), a large number of semisynthetic compounds have been
produced. These have been conventionally divided into 4 generations. This
division has a chronological sequence of development, but more importantly,
takes into consideration the overall antibacterial spectrum as well as potency.
All cephalosporins are
bactericidal and have the same mechanism of action as penicillin, i.e.
inhibition of bacterial cell wall synthesis. However, they bind to different
proteins than those which bind penicillins. This may explain differences in
spectrum, potency and lack of cross resistance.
Acquired resistance to
cephalosporins could have the same basis as for penicillins, i.e.:
a)
alteration in target proteins (PBPs) reducing
affinity for the antibiotic.
b)
impermeability to the antibiotic or its efflux
so that it does not reach its site of action.
c)
elaboration of βlactamases which
destroy specific cephalosporins (cephalosporinases).
Though the incidence
is low, resistance has been developed by some organisms, even against the third
generation compounds. Individual cephalosporins differ in their:
a)
Antibacterial spectrum and relative potency
against specific organisms.
b)
Susceptibility to βlactamases elaborated
by different organisms.
c)
Pharmacokinetic properties—many have to be
injected, some are oral; majority are not metabolized, and are excreted rapidly
by the kidney; have short t½s, probenecid inhibits their tubular secretion.
d)
Local irritancy on i.m. injection; few cannot
be injected i.m.
FIRST GENERATION CEPHALOSPORINS
These were developed
in the 1960s, have high activity against gram-positive but weaker against gram-negative
bacteria.
Cefazolin
This prototype first
generation cephalosporin is active against most PnG sensitive organisms, i.e. Streptococci (pyogenes as well as viridans), gonococci, meningococci, C. diphtheriae, H. influenzae, clostridia
and Actinomyces. Activity against Klebsiella and E. coli is
relatively high, but it is quite susceptible to staphylococcal βlactamase. It can be
given i.m. (less painful) as well as i.v. and has a longer t½ (2 hours) due to
slower tubular secretion; attains higher concentration in plasma and in bile.
It is the preferred parenteral first generation cephalosporin, especially for
surgical prophylaxis.
Dose: 0.25 g 8 hourly (mild
cases), 1 g 6 hourly (severe cases)
i.m. or i.v.
ALCIZON, ORIZOLIN 0.25
g, 0.5 g, 1 g per vial inj.
Cephalexin
It is an orally
effective first generation
cephalosporin, similar in spectrum to cefazolin, but less active against
penicillinase producing Staphylococci
and H. influenzae. It is little bound
to plasma proteins, attains high concentration in bile and is excreted unchanged
in urine; t½ ~60 min. It is one of the most commonly used cephalosporins.
Dose: 0.25–1 g 6–8 hourly
(children 25–100 mg/kg/day). CEPHACILLIN 250, 500
mg cap; SPORIDEX, ALCEPHIN, CEPHAXIN 250, 500 mg cap, 125 mg/5 ml dry syr., 100
mg/ml pediatric drops.
ALCEPHINLA: Cephalexin + probenecid (250 + 250 mg and 500 + 500
mg) tabs.
Cephradine
Another orally active
drug, almost identical to
cephalexin, but less active against some organisms. Oral administration has caused
diarrhoea as side effect. It is available for parenteral use also.
Dose: 0.25–1 g 6–12 hourly
oral/i.m/i.v.
CEFLAD 0.25, 0.5, 1 g
per vial inj.
Cefadroxil
A close congener of
cephalexin; has good tissue
penetration—exerts more sustained action at the site of infection; can be given
12 hourly despite a t½ of 1 hr. It is excreted unchanged in urine, but dose
need be reduced only if creatinine clearance is < 50 ml/min. The
antibacterial activity of cefadroxil and indications are similar to those of cephalexin.
Dose: 0.5–1 g BD. DROXYL 0.5, 1 g tab,
250 mg/5 ml syr; CEFADROX 0.5 g cap,
125 mg/5 ml syr and 250 mg kid tab; KEFLOXIN 0.5 g cap, 0.25 g Distab, 125 mg/5
ml susp.
SECOND GENERATION CEPHALOSPORINS
These were developed subsequent to the first generation
compounds and are more active against gram-negative organisms, with some
members active against anaerobes, but none inhibits P. aeruginosa. Clinically, they have been largely replaced by the
3rd generation agents that are more active.
Cefuroxime
It is resistant to gram-negative βlactamases: has high activity against
organisms
producing
these enzymes including PPNG and ampicillin-resistant H. influenzae, while retaining significant activity on gram-positive
cocci and certain anaerobes. It is well tolerated by i.m. route and attains
relatively higher CSF levels, but has been superseded by 3rd generation cephalosporins
in the treatment of meningitis. It has been employed for single dose i.m.
therapy of gonorrhoea due to PPNG.
CEFOGEN, SUPACEF, FUROXIL
250 mg and 750 mg/ vial inj; 0.75–1.5 g i.m. or i.v. 8 hourly, children
30–100 mg/kg/day.
Cefuroxime axetil
This ester of
cefuroxime is effective orally,
though absorption is incomplete. The activity depends on in vivo hydrolysis and release of cefuroxime.
Dose: 250–500 mg BD,
children half dose; CEFTUM, SPIZEF 125, 250, 500 mg captab and 125 mg/5 ml
susp.
Cefaclor
It retains significant
activity by the oral route and is more
active than the first generation compounds against H. influenzae, E. coli and Pr.
mirabilis.
Dose: 0.25–1.0 g 8 hourly
KEFLOR, VERCEF,
DISTACLOR 250 mg cap, 125 and 250 mg distab, 125 mg/5 ml dry syr, 50 mg/ml ped.
drops.
THIRD GENERATION CEPHALOSPORINS
These compounds
introduced in the 1980s have highly augmented activity against gram-negative
Enterobacteriaceae; some inhibit Pseudomonas
as well. All are highly resistant to βlactamases from gram-negative bacteria.
However, they are less active on gram-positive cocci and anaerobes.
Cefotaxime
It is the prototype of
the third generation cephalosporins;
exerts potent action on aerobic gram-negative as well as some gram-positive
bacteria, but is not active on anaerobes (particularly Bact. fragilis), Staph.
aureus and Ps. aeruginosa. Prominent indications are
meningitis caused by gram-negative
bacilli (attains relatively high CSF levels), life-threatening resistant/
hospital-acquired infections, septicaemias and infections in immunocompromised
patients. It is also utilized for single dose therapy (1 g i.m. + 1 g probenecid
oral) of PPNG urethritis, but is not dependable for Pseudomonas infections.
Cefotaxime is
deacetylated in the body; the metabolite exerts weaker but synergistic action
with the parent drug. The plasma t½ of cefotaxime is 1 hr, but is longer for
the deacetylated metabolite—permitting 12 hourly doses in many situations.
Dose: 1–2 g i.m./i.v. 8–12
hourly, children 50–100 mg/kg/day.
OMNATAX, ORITAXIM, CLAFORAN 0.25, 0.5, 1.0 g per vial inj.
Ceftizoxime
It is similar in
antibacterial activity and indications to
cefotaxime, but inhibits B. fragilis also.
It is not metabolized—excreted by the
kidney at a slower rate; t½ 1.5–2 hr.
Dose: 0.5–2.0 g i.m./i.v. 8
or 12 hourly.
CEFIZOX, EPOCELIN 0.5
and 1 g per vial inj.
Ceftriaxone
The distinguishing
feature of this cephalosporin is its
longer duration of action (t½ 8 hr), permitting once, or at the most twice
daily dosing. Penetration into CSF is good and elimination occurs equally in
urine and bile.
Ceftriaxone has shown high efficacy in a wide range of serious infections
including bacterial meningitis (especially in children), multi-resistant
typhoid fever, complicated urinary tract infections, abdominal sepsis and
septicaemias. A single dose of 250 mg i.m. has proven curative in gonorrhoea
including PPNG, and in chancroid.
Hypo-prothrombinaemia and bleeding are specific adverse effects.
Haemolysis is reported.
OFRAMAX, MONOCEF, MONOTAX 0.25, 0.5, 1.0 g per vial inj.
For skin/soft tissue/urinary infections: 1–2 g i.v. or i.m./
day.
Meningitis: 4 g followed by 2 g i.v. (children 75–100 mg/ kg)
once daily for 7–10 days.
Typhoid: 4 g i.v. daily × 2 days followed by 2 g/day (children
75 mg/kg) till 2 days after fever subsides.
Ceftazidime
The most prominent
feature of this third generation
cephalosporin is its high activity against Pseudomonas.
It has been specifically used in febrile neutropenic patients with haematological
malignancies, burn, etc. Its activity against Enterobacteriaceae is similar to
that of cefotaxime, but it is less active on Staph. aureus, other gram positive cocci and anaerobes like Bact. fragilis. Its plasma t½ is 1.5–1.8
hr.
Neutropenia, thrombocytopenia, rise in plasma transaminases and
blood urea have been reported.
Dose: 0.5–2 g i.m. or i.v.
every 8 hr, children 30 mg/kg/ day. Resistant
typhoid 30 mg/kg/day.
FORTUM, CEFAZID, ORZID
0.25, 0.5 and 1 g per vial inj.
Cefoperazone
Like ceftazidime, it
differs from other third generation
compounds in having stronger activity on Pseudomonas
and weaker activity on other organisms. It is good for S. typhi and B. fragilis also,
but more susceptible to βlactamases. The indications are—severe
urinary, biliary, respiratory, skinsoft tissue infections, meningitis and
septicaemias. It is primarily excreted in bile; t½ is 2 hr. It has hypoprothrombinaemic
action but does not affect platelet function. A disulfiramlike reaction with
alcohol has been reported.
Dose: 1–3 g i.m./i.v. 8–12
hourly.
MAGNAMYCIN 0.25 g, 1,
2 g inj; CEFOMYCIN, NEGAPLUS 1 g inj.
Cefixime
It is an orally active
third generation cephalosporin highly
active against Enterobacteriaceae, H.
influenzae and is resistant to many βlactamases. However,
it is not active on Staph. aureus, most pneumococci and Pseudomonas. It is longer acting (t½ 3 hr) and has been used in a dose of 200–400 mg
BD for respiratory, urinary and biliary infections. Stool changes and diarrhoea
are the most prominent side effects.
TOPCEF, ORFIX 100, 200
mg tab/cap, CEFSPAN 100 mg cap, 100 mg/5 ml syr.
Cefpodoxime Proxetil
It is the orally
active ester prodrug of 3rd
generation cephalosporin cefpodoxime. In addition to being highly active
against Enterobacteriaceae and streptococci, it inhibits Staph. aureus. It is used mainly for respiratory, urinary, skin and
soft tissue infections.
Dose: 200 mg BD (max 800
mg/day)
CEFOPROX 100, 200 mg
tab, 100 mg/5 ml dry syr; CEPODEM 100, 200 mg tab, 50 mg/5 ml susp.
Cefdinir
This orally active 3rd
generation cephalosporin has good
activity against many β lactamase producing organisms. Most
respiratory pathogens including gram-positive cocci are susceptible. Its
indications are pneumonia, acute exacerbations of chronic bronchitis, ENT and
skin infections.
Dose: 300 mg BD
SEFDIN, ADCEF 300 mg
cap, 125 mg/5 ml susp.
Ceftibuten
Another oral 3rd
generation cephalosporin, active
against both gram-positive
and gram-negative bacteria, but not pneumococci and Staph. aureus and stable to βlactamases. It is
indicated in respiratory, urinary and gastrointestinal infections; t½ 2–3
hours.
Dose: 200 mg BD or 400 mg
OD.
PROCADAX 400 mg cap, 90 mg/5 ml powder for oral suspension.
Ceftamet Pivoxil
This ester prodrug of
ceftamet, a 3rd generation
cephalosporin has high activity against gram-negative bacteria, especially
Enterobacteriaceae and N. gonorrhoea;
used in respiratory, skinsoft tissue infections, etc.
Dose: 500 mg BD–TDS.
ALTAMET 250 tab;
CEPIMEO 500 mg tab.
FOURTH GENERATION CEPHALOSPORINS
Cefepime
Developed in 1990s,
this 4th generation cephalosporin has antibacterial spectrum similar to that of
3rd generation compounds, but is highly resistant to βlactamases, hence
active against many bacteria resistant to the earlier drugs. Ps. aeruginosa and Staph. aureus are also inhibited. Due to high potency and extended
spectrum, it is effective in many serious infections like hospital-acquired
pneumonia, febrile neutropenia, bacteraemia, septicaemia, etc.
Dose: 1–2 g (50 mg/kg) i.v.
8–12 hourly.
KEFAGE, CEFICAD,
CEPIME 0.5, 1.0 g inj.
Cefpirome
This 4th generation
cephalosporin is indicated for the
treatment of serious and resistant hospital-acquired infections including
septicaemias, lower respiratory tract infections, etc. Its zwitterion character
permits better penetration through porin channels of gram-negative bacteria. It
is resistant to many βlactamases; inhibits type 1 β lactamase producing
Enterobacteriaceae and it is more potent against gram-positive and some gram-negative
bacteria than the 3rd generation compounds.
Dose: 1–2 g i.m./i.v. 12
hourly;
CEFROM, CEFORTH 1 g inj; BACIROM, CEFOR 0.25, 0.5, 1.0 g inj.
Adverse Effects
·
Pain after i.m. injection occurs with many. This is so severe with cephalothin as to
interdict i.m. route, but many others can be injected i.m. (see individual compounds).
Thrombophlebitis of injected vein can occur.
· Diarrhoea due to alteration of gut ecology or irritative effect is more common with
oral cephradine and parenteral cefoperazone (it is significantly excreted in
bile).
· Hypersensitivity Reactions caused by cephalosporins are similar to
penicillin, but incidence is lower. Rashes are the most frequent manifestation,
but anaphylaxis, angioedema, asthma and urticaria have also occurred. About 10%
patients allergic to penicillin show cross reactivity with cephalosporins.
Those with a history of immediate type of reactions to penicillin should better
not be given a cephalosporin. Skin tests for sensitivity to cephalosporins are
unreliable. A positive Coombs’ test occurs in many, but haemolysis is rare.
·
Nephrotoxicity is highest with
cephaloridine, which consequently has
been withdrawn. Cephalothin and a few others have lowgrade nephrotoxicity which
may be accentuated by preexisting renal disease, concurrent administration of
an aminoglycoside or loop diuretic.
· Bleeding occurs with cephalosporins having a methyl-thiotetrazole or similar
substitution at position 3 (cefoperazone, ceftriaxone). This is due to hypo-prothrombinaemia
caused by the same mechanism as warfarin and is more common in patients with
cancer, intraabdominal infection or renal failure.
·
Neutropenia and thrombocytopenia are rare
adverse effects reported with ceftazidime and some others.
·
A disulfiramlike interaction with alcohol has
been reported with cefoperazone.
Uses
Cephalosporins are now
extensively used antibiotics. Their indications are:
·
As alternatives to PnG; particularly in
allergic patients (but not who had anaphylactic reaction); one of the first
generation compounds may be used.
· Respiratory, urinary and soft tissue
infections caused by gram-negative organisms, especially Klebsiella, Proteus, Enterobacter, Serratia. Cephalosporins
preferred for these infections are cefuroxime, cefotaxime, ceftriaxone.
· Penicillinase producing staphylococcal
infections.
· Septicaemias caused by gram-negative
organisms: an aminoglycoside may be combined with a cephalosporin.
· Surgical Prophylaxis: the first generation
cephalosporins are popular drugs. Cefazolin (i.m. or i.v.) is employed for most
types of surgeries including those with surgical prosthesis such as artificial
heart valves, artificial joints, etc.
·
Meningitis: Optimal therapy of
pyogenic meningitis requires bactericidal activity in the CSF, preferably with
antibiotic concentrations several times higher than the MBC for the infecting
organism. For empirical therapy before bacterial diagnosis, i.v.
cefotaxime/ceftriaxone is generally combined with ampicillin or vancomycin. Ceftazidime
+ gentamicin is the most effective therapy for Pseudomonas meningitis.
· Gonorrhoea caused by penicillinase producing
organisms: ceftriaxone is a first choice drug for single dose therapy of
gonorrhoea if the penicillinase producing status of the organism is not known.
Cefuroxime and cefotaxime have also been used for this purpose. For chancroid
also, a single dose is as effective as erythromycin given for 7 days.
·
Typhoid: Currently, ceftriaxone
and cefoperazone injected i.v. are the fastest acting and most reliable drugs
for enteric fever. They are an alternative to fluoroquinolones (especially in
children) for empirical therapy, since many S.
typhi strains are resistant to
chloramphenicol, ampicillin and
cotrimoxazole.
· Mixed aerobicanaerobic infections in cancer
patients, those undergoing colorectal surgery, obstetric complications:
cefuroxime, cefaclor or one of the third generation compounds is used.
· Hospital acquired infections resistant to commonly
used antibiotics: cefotaxime, ceftizoxime or a fourth generation drug may work.
·
Prophylaxis and treatment of infections in
neutropenic patients: ceftazidime or another third generation compound, alone
or in combination with an aminoglycoside.
