Cardiac Electrophysiological Considerations
| Home | | Pharmacology |Chapter: Essential pharmacology : Cardiac Electrophysiological Considerations
Drugs having their major action on heart or blood vessels, or those used primarily for cardiovascular disorders are designated cardiovascular drugs. They can act directly on the cardiovascular structures or through the autonomic/central nervous system, kidney, autacoids or hormones which regulate cardiovascular function.
CARDIAC ELECTROPHYSIOLOGICAL
CONSIDERATIONS
Drugs having their major action on heart or blood vessels, or
those used primarily for cardiovascular disorders are designated cardiovascular
drugs. They can act directly on the cardiovascular structures or through the
autonomic/central nervous system, kidney, autacoids or hormones which regulate
cardiovascular function.
Cardiac Electrophysiology
The properties which are especially important for understanding
drug action on heart are:
1. Impulse Generation
Electrophysiologically, two types of
myocardial fibres can be distinguished (Fig. VIII.1).
(a) Nonautomatic Fibres These are the ordinary working myocardial
fibres; cannot generate an impulse of their own. During diastole, the resting
membrane potential remains stable (approximately 90 mv negative inside). When
stimulated, they depolarize very rapidly (fast 0 phase) with considerable overshoot
(+ 30 mv) → rapid return to near
isoelectric level (phase1) → maintenance of membrane potential at this
level for a considerable period (phase2, plateau phase) during which Ca2+
ions flow in and bring about contraction → relatively rapid
repolarization (phase-3 during which membrane Na+K+ pump
gets activated and tends to restore ionic distribution to the resting pattern.
Resting membrane potential, once attained, does not decay (stable phase-4).
(b) Automatic
Fibres These are present in the sinoatrial (SA) and
atrioventricular (AV) nodes, and in the His-Purkinje system, i.e. especialized
conducting tissue. In addition, patches of automatic tissue are present in the
interatrial septum, AV ring and around openings of the great veins. The most
characteristic feature of these fibres is phase-4
or slow diastolic depolarization,
i.e. after repolarizing to the
maximum value, the membrane potential decays spontaneously. When it reaches a
critical threshold value—sudden depolarization occurs automatically. Thus, they
are capable of generating their own impulse. The rate of impulse generation by
a particular fibre depends on the value of maximal diastolic potential, the
slope of phase4 depolarization and the value of threshold potential.
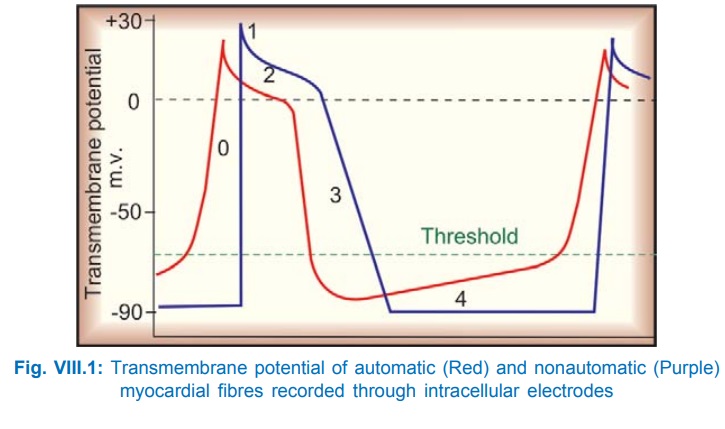
Normally, the SA node has the steepest phase4 depolarization,
undergoes self-excitation and propagates the impulse to the rest of the heart—
acts as the pacemaker. Other fibres
which are also undergoing phase4 depolarization, but at a slower rate, receive
the propagated impulse before reaching threshold value and remain as latent pacemakers.
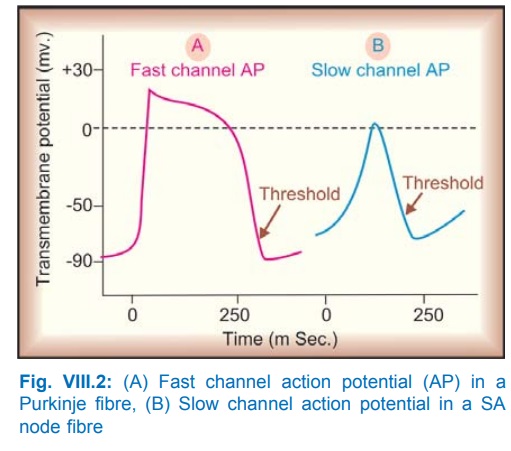
Two types of action
potential (AP) are possible. These
are depicted in Fig. VIII.2. Their characteristics are given in Table VIII. 1.
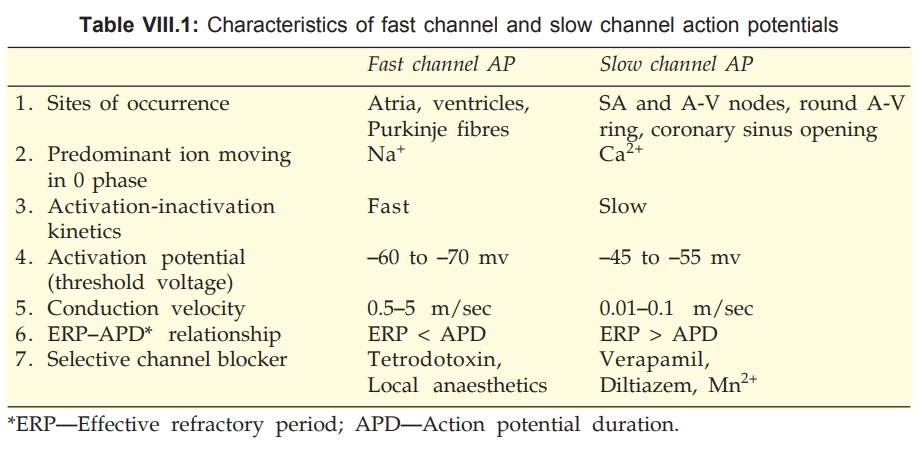
The slow channel AP is
characterised by:
·
Initiation at a higher threshold (less
negative level).
·
Slow depolarization during 0 phase.
·
Less overshoot, low amplitude.
·
Very slow propagation, decremental conduction
and a low safety factor for conduction.
·
Can arise and propagate in fibres too depolarized
to support fast channel responses.
Slow channel AP in SA
node, AV node, etc. has a shorter duration and phases 1–3 are not clearly
demarkated. Slow channel AP can occur in Purkinje fibres (PF) also, but this has
a much longer duration with a prominent plateau phase.
2. Conduction
The rate of conduction
through a fibre is a function
of its membrane responsiveness, which
is defined by rate of rise of AP (dv/dt) as a function of membrane potential at
which activation occurs (Fig. VIII.3); a more completely polarized membrane
depolarizes faster. This type of relationship is seen in atrial, ventricular
and Purkinje fibres (fast channel fibres which depolarize by Na+
current), but not in SA and AV nodal cells which remain refractory for some
time even after attainment of maximal resting potential.
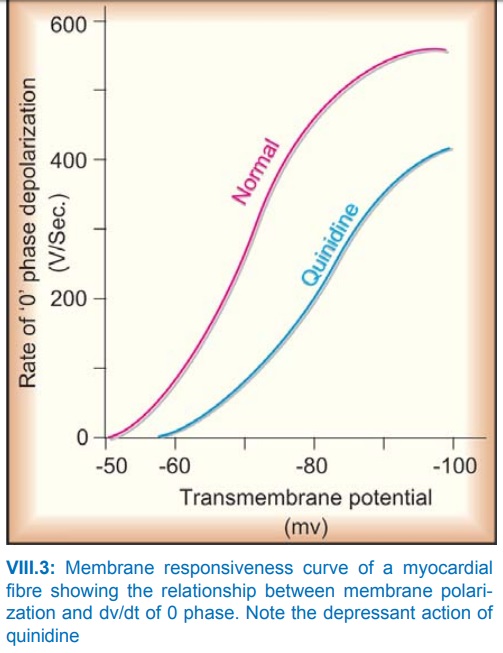
The Na+ channels get progressively inactivated as the
resting membrane potential (RMP) drops over the –80 to –60 mV range.
Consequently, less negative the RMP at which activation occurs, fewer are the
Na+ channels available for activation—slope of ‘0’ phase depolarization,
AP amplitude and conduction velocity are reduced.
A drug which reduces the slope of 0 phase (at any given resting membrane potential) will shift the membrane responsiveness curve to the right and impede conduction. The reverse occurs with a drug that shifts the curve to the left. Membrane responsiveness curve can also be altered by disease.
Small cells at the upper margin of AV node have very low conduction
velocity (20 mm/sec). Normally Purkinje fibres (PFs) have the highest
conduction velocity (4000 mm/sec) except near their junction with the
ventricular fibres ‘gate region’, or if they change over from fast channel to
slow channel response.
3. Excitability
This property of a
fibre is defined by the
strength of stimulus required to elicit a response or to produce an AP. Hyperpolarization
decreases excitability while small reductions in resting membrane potential
increase excitability by respectively increasing and decreasing the gap between
it and the threshold potential. Thus, in fast channel fibres excitability
is generally supernormal
during the end of phase3. However, when the resting membrane potential is
reduced to a value below the threshold potential, the fibre becomes
inexcitable.
4. Refractory
Period
Pharmacologically, the effective refractory period (ERP) which is the
minimum interval between two propagating APs, is the most important. It is
closely related to the AP duration (APD). An AP can be evoked in fast channel fibres
even before complete repolarization, because Na+ channels recover in
a voltage-dependent manner above the threshold potential. As such ERP/APD is
<1. By contrast, the Ca2+ channels recover in a time-dependent
manner progressively after the fibre has fully repolarized. Thus, in slow
channel fibres ERP/ APD is > 1. Most antiarrhythmic drugs increase ERP/APD
ratio.
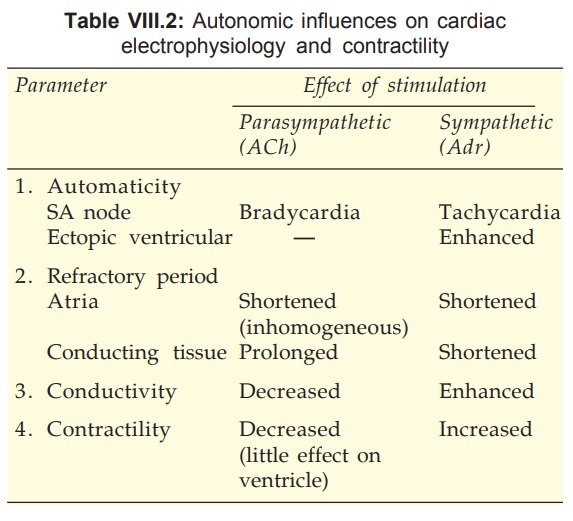
Autonomic Influences On Cardiac
Electrophysiology And Contractility
It would be profitable
to recapitulate the influence of sympathetic and parasympathetic stimulation on
variables of cardiac function, because many cardiovascular drugs have
indirect/secondary autonomic effects (Table VIII.2).
Related Topics
