Blood Types and Transfusions
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Blood
Blood consists of different types, not all of which are compatible.
Blood
Types and Transfusions
Blood consists of different types, not all of which are compatible. Safe blood transfusions of
whole blood depend on matching the blood types of both donors and recipients.
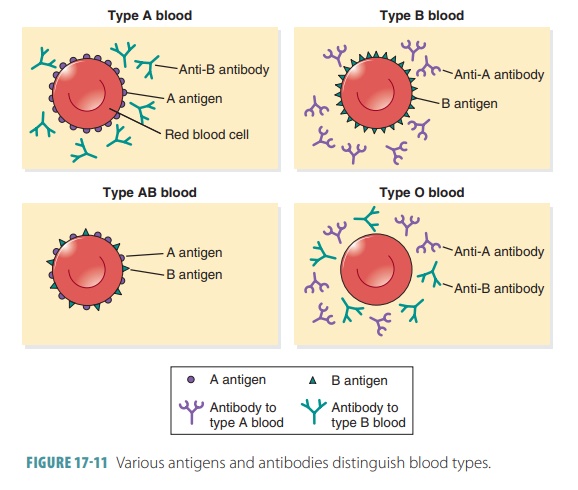
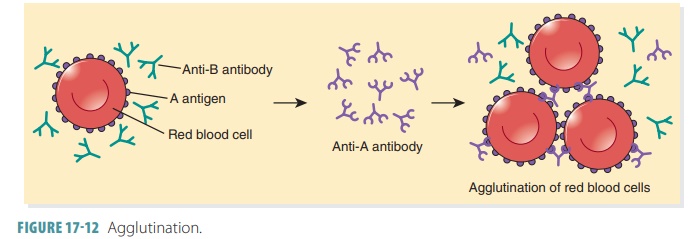
The clumping of RBCs after a transfusion reaction is called agglutination. This involves RBC surface
molecules called antigens or agglutinogens that react with antibodies or agglutinins from the plasma. There
are at least50 kinds of surface antigens
on RBC membranes.
The ABO blood groups, determined by the pres-ence or absence
of specific surface antigens in RBC cell membranes, are called blood types. The ABO blood group is
based on the presence or lack of the major protein antigens A and B on RBC
membranes.
Erythrocytes may have one of the following four antigen
combinations:
■■ Antigen
A only: type A blood
■■ Antigen
B only: type B blood
■■ Both
antigen A and B: type AB blood, the least common type
■■ Neither
antigen A or B: type O blood, the most common type
Blood types are inherited. Antibodies related to each type
of antigen are produced between two and eight months after birth. For example,
if antigen A is absent, the antibody called anti-A
is produced. There-fore, people with type A blood, meaning that antigen A is
present but antigen B is absent, have anti-B
antibody. The opposite is true for people with type B blood. Those with type AB
blood have neither of the two antibodies. People with type O blood have both
antibodies (FIGURE
17-11). The anti-A and anti-B antibodies are very large and
cannot cross the placenta. This means that a pregnant woman and her fetus may
have different blood types, and agglutination in the fetus cannot occur. TABLE 17-4 summarizes blood types, antigens,
and antibodies.
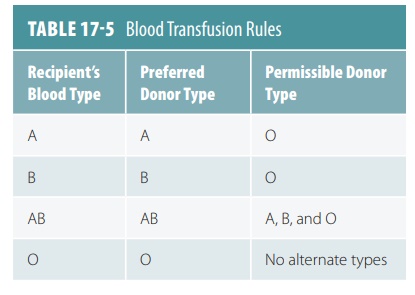
Antibodies of a certain type react with antigens of the same
type and cause clumping of RBCs, so these combinations must be avoided. For
example, a person with type A or anti-B
blood must not receive blood of either type B or type AB to avoid clumping. A
person with type B or anti-A blood
must not receive type A or type AB blood. A person with type O or anti-A andanti-B blood must not receive
type A, B, or AB blood.Because type AB blood lacks both anti-A and anti-B
antibodies, those with type AB blood can receive transfusions from any other
type. Because of this, type AB individuals are called universal recipients.
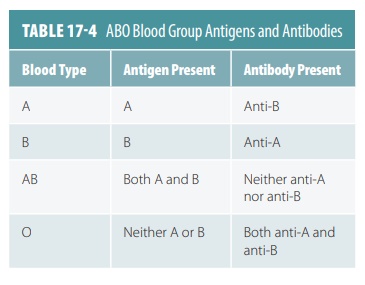
Rapid transfusion must be avoided, however, because
agglutination can still occur because of certain antibodies in the blood being
transfused. It is therefore always best to transfer blood from the same type
into the person requiring the transfusion (TABLE 17-5). Note the permissible donor types listed in Table 17-5
should be used only in extreme emergencies. Cross-matchtesting
involves exposing donor RBCs to samples ofa recipient’s plasma under
careful control to reveal significant cross-reactions involving surface
antigens other than the A, B, or Rh antigens. Lost blood can also be replaced
with synthetic blood substitutes because these do not contain surface antigens.
FIGURE
17 -12 illustrates the concepts of agglutina-tion.
Because type O blood lacks antigens A and B, it can be transfused, in extreme
emergencies, into people with any other type. Because of this, people with type
O blood are called universal donors.
Type O blood still should be given slowly to people of other blood types so it will
be diluted by the recipient’s blood volume, minimizing chances of an adverse
reaction.
For blood typing, blood is drawn from a vein, and the blood sample is mixed with antibodies against type A and B blood. It is checked to see whether the blood cells agglutinate or not. When they agglutinate, the blood has reacted with one of the antibodies. The next step is called back typing. The blood serum is mixed with blood that is known to be either type A or type B, which accurately determines the blood type. Also, Rh typing is performed with a similar method of testing.
Rh Blood Group
The Rh blood
group got its name from the rhesus monkey, because it was in this
type of monkey the blood group was first studied. There are several Rhfactors in humans, the most
prevalent of which isantigen D. If present on the RBC membranes, the blood is
called Rh-positive. If not, it is
called Rh-negative. Only 15% of the
U.S. population is Rh-negative. The presence or absence of Rh antigen is
inherited, but the antibodies that react with it, which are called anti-Rhantibodies, are not spontaneous.
They form only inRh-negative people because of specific stimulation.
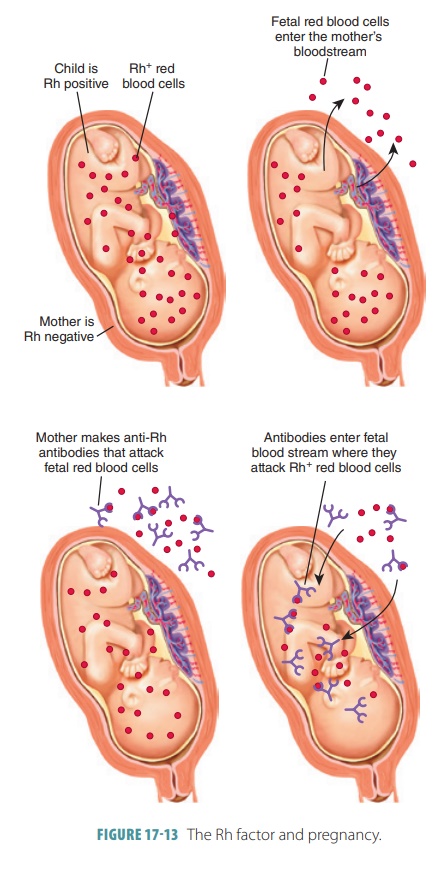
A similar condition can occur when an Rh- negative woman is pregnant with an Rh-positive fetus (FIGURE 17-13). Although the pregnancy may be normal, at birth or miscarriage the placental membranes tear, allowing some of the fetal Rh-positive RBCs to enter the mother’s circulation. This may stimulate her tissues to begin producing anti-Rh antibodies. If she becomes pregnant a second time and the fetus is Rh-positive, these antibodies or hemolysins cross the placental mem-brane to destroy the fetal RBCs. The fetus develops erythroblastosis fetalis, which is also calledhemolyticdisease of the fetus and newborn. Although extremelyrare because of the careful management of Rh status, erythroblastosis fetalis may cause the death of the fetus or infant. Signs of this condition in an infant include anemia, enlarged liver or spleen, generalized swelling, and newborn jaundice, which is yellowing of the skin and eyes due to liver or bile duct abnormalities resulting in high levels of circulating bilirubin.
Blood Transfusion
The preferred method of blood transfusion is the use of packed red blood cells (PRBCs). This involves whole blood, from which most of the
leukocytes and plasma have been removed. This restores the blood’s
oxygen-carrying capacity and is much more common than whole blood transfusions, which are indicated only when
blood loss is substantial and rapid. Blood banks usually collect donor blood
and mix it with an anticoagulant. This prevents clotting because of bind-ing of
calcium ions. Collected blood has a shelf life of about 35 days. Since blood is
very valuable, it is usually separated into component parts. Therefore, each
com-ponent can be used as it is needed.
1. Which blood type is the universal recipient, and which
blood type is the universal donor? Why?
2. Explain the Rh blood group and name the condition it may
cause in a fetus.
3. Define the terms agglutination,
antigens, and antibodies.