Benzodiazepines (BZDS)
| Home | | Pharmacology |Chapter: Essential pharmacology : Sedative -Hypnotics
Chlordiazepoxide and diazepam were introduced around 1960 as antianxiety drugs. Since then this class has proliferated and has gained popularity over barbiturates as hypnotic and sedative as well, because—
BENZODIAZEPINES (BZDS)
Chlordiazepoxide and diazepam
were introduced around 1960 as antianxiety drugs. Since then this class has
proliferated and has gained popularity over barbiturates as hypnotic and
sedative as well, because—
1.
BZDs have a high therapeutic index. Ingestion
of even 20 hypnotic doses does not usually endanger life—there is no loss of
consciousness (though amnesia occurs) and patient can be aroused; respiration
is not so depressed as to need assistance.
2.
Hypnotic doses do not affect respiration or
cardiovascular functions. Higher doses produce mild respiratory depression and
hypotension which is problematic only in patients with respiratory
insufficiency and cardiac/haemodynamic abnormality.
3.
BZDs have practically no action on other body
systems. Only on i.v. injection the BP falls (may be marked in an occasional
patient) and cardiac contractility decreases. Fall in BP in case of diazepam
and lorazepam is due to reduction in cardiac output while that due to midazolam
is due to decrease in peripheral resistance. The coronary arteries dilate on
i.v. injection of diazepam.
4.
BZDs cause less distortion of sleep architecture;
rebound phenomena on discontinuation of regular use are less marked.
5.
BZDs do not alter disposition of other drugs
by microsomal enzyme induction.
6.
They have lower abuse liability: tolerance is
mild, psychological and physical dependence and withdrawal syndrome are less
marked.
7.
A specific BZD antagonist flumazenil is available which can be used in case of poisoning.
CNS actions The overall action of all BZDs is qualitatively similar, but there are prominent
differences in selectivity and timecourse of action: different members are used
for different purposes. In contrast to barbiturates, they are not general depressants,
but exert relatively selective anxiolytic, hypnotic, muscle relaxant and anticonvulsant
effects in different measures. Even when apparently anaesthetic dose of
diazepam is administered i.v., some degree of awareness is maintained, though
because of anterograde amnesia (interference with establishment of memory trace)
the patient does not clearly recollect the events on recovery. The antianxiety action of BZDs is
probably not dependent on their sedative property; with chronic administration
relief of anxiety is maintained, but drowsiness wanes off due to development of
tolerance.
While there are
significant differences among different BZDs, in general, they hasten onset of sleep, reduce intermittent awakening and increase total sleep time (specially in
those who have a short sleep span). Time spent in stage 2 is increased while
that in stage 3 and 4 is decreased. They tend to shorten REM phase, but more
REM cycles may occur so that overall effect on REM sleep is less marked than
with barbiturates. Nitrazepam has been shown to actually increase REM sleep.
Night terrors and body movements during sleep are reduced and stage shifts to
stage 1 and 0 are lessened. Most subjects wake up with a feeling of refreshing
sleep. Some degree of tolerance develops to the action of BZDs on sleep after repeated
nightly use.
BZDs produce centrally mediated skeletal muscle relaxation without impairing
voluntary activity. Clonazepam and
diazepam have more marked muscle relaxant property. Very high doses depress
neuromuscular transmission.
Clonazepam, diazepam,
nitrazepam and flurazepam have more prominent anticonvulsant activity than other BZDs. However, their utility in
epilepsy is limited by development of tolerance to the anticonvulsant action.
Given i.v., diazepam (but not others) causes analgesia. In contrast
to barbiturates, BZDs do not produce hyperalgesia.
Other actions Diazepam decreases
nocturnal gastric secretion and
prevents stress ulcers. BZDs do not significantly affect bowel movement.
Shortlasting coronary dilatation is produced by i.v. diazepam.
Site And Mechanism Of Action
Benzodiazepines act preferentially on midbrain ascending
reticular formation (which maintains wakefulness) and on limbic system (thought
and mental functions). Muscle relaxation is produced by a primary medullary
site of action and ataxia is due to action on cerebellum.
BZDs act by enhancing
presynaptic/postsynaptic inhibition through a specific BZD receptor which is an
integral part of the GABAA receptor–Cl¯ channel complex. The subunits
of this complex form a pentameric transmembrane anion channel (Fig. 29.3) gated
by the primary ligand (GABA), and modulated by secondary ligands which include
BZDs. Only the α and β subunits are required for GABA action, and most likely the
binding site for GABA is located on the subunit, while the α/γ subunit interface
carrys the BZD binding site. The modulatory BZD receptor increases the
frequency of Cl¯ channel opening induced by submaximal concentrations of GABA.
The BZDs also enhance binding of GABA to GABAA receptor. The GABAA
antagonist bicuculline antagonizes BZD action in a noncompetitive manner. It is
noteworthy that the BZDs do not themselves increase Cl¯ conductance; have only
GABA facilitatory but no GABA mimetic action. This probably explains the lower
ceiling CNS depressant effect of BZDs.
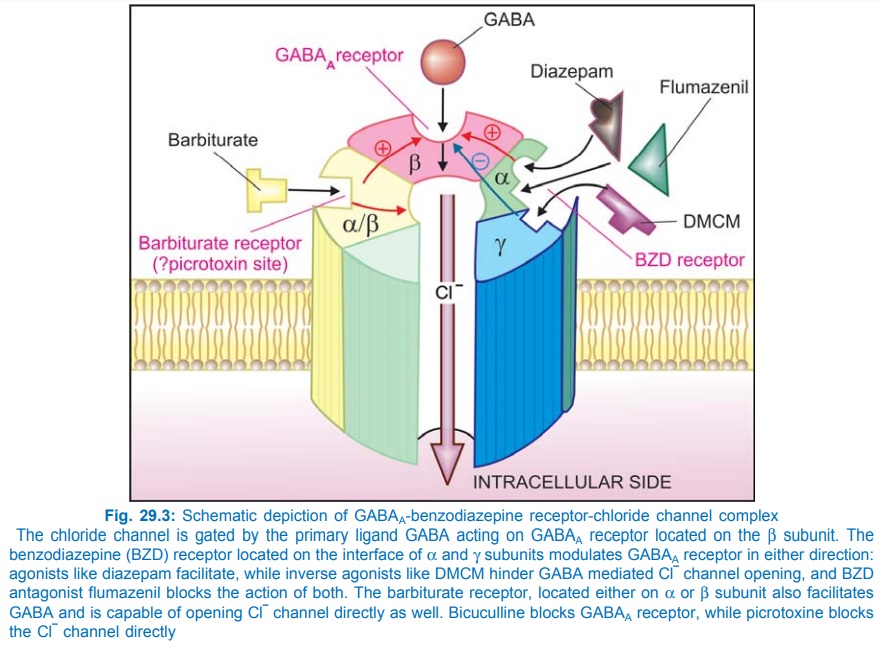
The BZD receptor exhibits a considerable degree of constitutive
activation. As such, it is capable of fine tuning GABA action in either
direction. While the BZD-agonists enhance GABA induced hyperpolarization (due
to influx of Cl¯ ions), and decrease firing rate of neurones, other compounds
called BZD-inverse agonists like
dimethoxy ethyl-carbomethoxyβcarboline (DMCM) inhibit GABA action and are
convulsants. The competitive BZD-antagonist flumazenil blocks the sedative
action of BZDs as well as the convulsant action of DMCM.
The GABAA-BZD
receptor-Cl– channel complex is composed of five α, β, γ, and in some cases δ, ε, θ or π subunits. Several
isoforms of α,
β
and γ subunits have been
cloned. The subunit composition of the complex differs at different sites, i.e.
there are multiple subtypes of BZD receptor. The ( α12 β2 2 γ2 ) pentamer appears to
be the most commonly occurring BZD receptor isoform. Based on studies conducted
in genetically mutated mice, it has been suggested that BZD receptor isoforms
containing the α1 subunit are involved
in mediating sedative, hypnotic, amnesic and possibly anticonvulsant actions of
BZDs, while those containing α2 subunits mediate
anxiolytic and muscle relaxant actions. Diazepam has similar affinity for BZD
receptor containing different (α1, α2, α3 or α5) subunits, and has
broad spectrum action. Receptor inhomogeneity may provide an explanation
for the pharmacological diversity of other BZDs. The newer non BZD hypnotics
zaleplon, Zolpidem, etc. have high affinity for α1 subunit isoform of
BZD receptor and exert selective hypnotic-amnesic effect, but have little
antiseizure or muscle relaxant property.
At high concentrations
BZDs also potentiate the depressant action of adenosine by blocking its uptake.
Certain actions of BZDs are countered by the adenosine antagonist theophylline.
Thus, BZDs could be acting through other mechanisms as well.
Pharmacokinetics
There are marked
pharmacokinetic differences among BZDs because they differ in lipid-solubility
by > 50 fold. Oral absorption of some is rapid while that of others is slow.
Absorption from i.m. sites is irregular except for lorazepam. Plasma protein binding
also varies markedly (flurazepam 10% to diazepam 99%). BZDs are widely
distributed in the body. The more lipid soluble members enter brain rapidly and
have a two phase plasma concentration decay curve; first due to distribution
and later due to elimination. A relatively short duration of action is obtained
with single dose of a drug that is rapidly redistributed, even though it may
have a long elimination t½. Using the elimination t½ alone to predict duration
of action may be misleading. However, elimination t½ determines duration of
action in case of drugs whose elimination is by far the dominant feature or
when the drug is given repeatedly.
Benzodiazepines are
metabolized in liver by dealkylation and hydroxylation to many metabolites,
some of which may be active. The biological effect half-life of these drugs may
be much longer than the plasma t½ of the administered compound. Some BZDs (e.g.
diazepam) undergo enterohepatic circulation. BZDs and their phase I metabolites
are excreted in urine as glucuronide conjugates. BZDs cross placenta and are
secreted in milk.
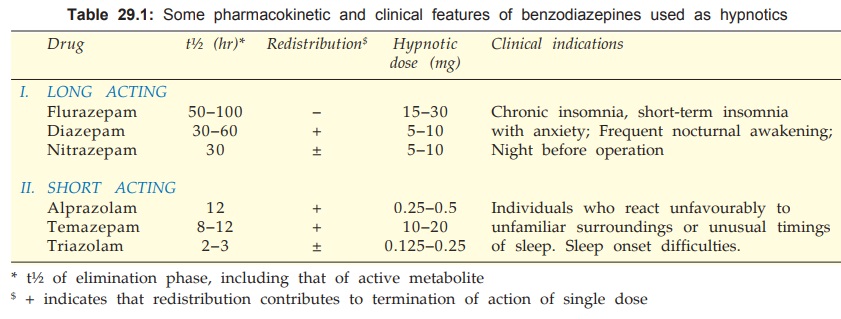
Drugs with a long t½
or those which generate active metabolites cumulate on nightly use; their
action may then extend into the next day. Some features of BZDs used as
hypnotic are given in Table 29.1.
BZDs may be
categorized according to their pharmacokinetic profile into:
1. Slow Elimination Of Parent Drug
Or Active Metabolite
Flurazepam Produces an active metabolite which has a long t½, residual effects are
likely next morning; cumulation occurs on daily ingestion peaking after 3–5
days; suitable for patients who have frequent nocturnal awakenings and in whom
some day time sedation is acceptable.
NINDRAL, FLURAZ 15 mg
cap.
2. Relatively Slow Elimination But
Marked Redistribution
Diazepam Generates active metabolites (des-methyl-diazepam,
oxazepam). On occasional use it is free of residual effects. With regular use
accumulation occurs and prolonged anxiolytic effect may be obtained. It is less
likely to cause rebound insomnia on discontinuation of chronic use. Withdrawal
phenomena are mild.
VALIUM 2, 5, 10 mg
tab., 10 mg/2 ml inj., CALMPOSE 5, 10 mg tab, 2 mg/5 ml syr, 10 mg/2 ml inj.
Nitrazepam Accumulation and residual effects can be avoided only if ingestion is
occasional. Good for patients with frequent nocturnal awakenings, when some day
time sedation is acceptable.
SEDAMON, HYPNOTEX,
NITRAVET 5 mg tab., 5, 10 mg cap.
3. Relatively Rapid Elimination And
Marked Redistribution
Alprazolam The primary indication of this intermediate acting BZD is anxiety disorder (see Ch. No. 33), but is also being
employed as nighttime hypnotic with few residual effects the next day.
Discontinuation after regular use has produced relatively marked withdrawal phenomena.
Temazepam It is an intermediate
acting BZD. Absorption is slow in
case of tablet but fast when used in soft gelatin capsule. Good for sleep onset
difficulty, free of residual effects. Accumulation can occur on daily
ingestion. Does not produce active metabolites.
4. Ultrarapid Elimination
Triazolam Very potent, peak
effect occurs in < 1 hour; good for sleep induction
but poor for maintaining it. Patient may wake up early in the morning and feel
anxious. This may be a withdrawal phenomenon. Rebound insomnia may occur when
it is discontinued after a few nights of use. It does not accumulate on
repeated nightly use and no residual effects are noted in the morning. However,
higher doses can alter sleep architecture, produce anterograde amnesia and anxiety
the following day. Some cases of paranoia and other psychiatric disturbances
have been noted—withdrawn from U.K., but is employed in other countries for
elderly patients, shift workers, travellers, etc.
Midazolam Extremely rapid absorption—peak in 20 min. It can cause problems in the elderly
(ataxia, blackouts); more liable for abuse. Therefore, it is not available now
for oral use as a hypnotic. Mainly used as an i.m. premedicant or an i.v.
anaesthetic.
Adverse Effects
Benzodiazepines are relatively safe drugs. Side effects of
hypnotic doses are dizziness, vertigo, ataxia, disorientation, amnesia,
prolongation of reaction time—impairment of psychomotor skills (should not
drive). Hangover is less common, but may be noted if larger doses are used,
especially of longer acting drugs. Weakness, blurring of vision, dry mouth and
urinary incontinence are sometimes complained. Older individuals are more
susceptible to psychomotor side effects. Like any hypnotic, BZDs can aggravate
sleep apnoea.
Paradoxical stimulation, irritability and sweating may occur in
an occasional patient, especially with flurazepam. Some patients experience
increase in nightmares and behavioural alterations, especially with nitrazepam.
Tolerance to the
sedative effects develops gradually, but there is little tendency to increase
the dose. Cross tolerance to alcohol and other CNS depressants occurs.
The dependence
producing liability of BZDs is low. They are seldom abused alone. Drug abusers find
them rather bland (except rapidly absorbed midazolam) and prefer other CNS
depressants. Withdrawal syndrome is generally mild; may be more intense in case
of ultrarapid elimination drugs. Drugseeking behaviour is not prominent.
Anxiety, insomnia, restlessness, malaise, loss of appetite, bad dreams is all
that occurs in most cases. Agitation, panic reaction, tremors and delirium are
occasional; convulsions are rare.
An earlier report of
increased birth defects on use of diazepam during pregnancy has been disputed.
Administration during labour may cause flaccidity and respiratory depression in
the neonate.
Interactions
BZDs synergise with
alcohol and other CNS depressants leading to excessive impairment. Concurrent
use with sod. valproate has provoked psychotic symptoms.
Drug interactions due
to displacement from protein binding or microsomal enzyme induction are not
significant.
Since CYP 3A4
isoenzyme plays important role in metabolism of several BZDs, their action can
be prolonged by CYP 3A4 inhibitors like ketoconazole, erythromycin and others.
Cimetidine, isoniazid and oral contraceptives also retard BZD metabolism.
Non-Benzodiazepine Hypnotics
Zopiclone This newer cyclopyrrolone hypnotic is an
agonist at a subtype of BZD receptor involved in the hypnotic action. The effect
on sleep resemble those of BZDs, but it does not alter REM sleep and tends to
prolong stages 3 and 4. It is reported not to disturb sleep architecture or
produce hangover or withdrawal phenomena on discontinuation; but some degree of
next morning impairment can occur. Zopiclone has been used to weanoff
insomniacs taking regular BZD medication. Its t½ is 5–6 hours.
Zopiclone is indicated for short term (< 2 weeks) treatment
of insomnia. Side effects are metallic or bitter aftertaste, impaired judgement
and alertness, psychological disturbances, dry mouth and rarely dependence.
Safety in overdose is similar to BZDs.
ZOPITRAN, ZOPICON, ZOLIUM, 7.5 mg tab, one tab at bedtime for not
more than 2–4 weeks (elderly 3.75 mg).
Zolpidem An imidazopyridine which preferentially acts
on the α1 subunit containing
subtype of BZD receptors that are important in mediating the hypnotic effect.
Hypnotic effect is pronounced: sleep latency is shortened, sleep duration is
prolonged in insomniacs, but anticonvulsant, muscle relaxant and antianxiety
effects are not evident. Its advantages are: relative lack of effect on sleep
stages (REM suppression is slight); minimal residual day time sedation or
fading of hypnotic action on repeated nightly use; no/little rebound insomnia
on discontinuation; near absence of tolerance or physical dependence and low
abuse potential combined with safety in overdose like BZDs.
Zolpidem is nearly
completely metabolized in liver (t½ 2 hr), and has short duration of action. It
is indicated for short term (1–2 weeks) sleep onset insomnia. Because the
plasma t½ is short, next day sedation is minimal, but morning sedation or
prolongation of reaction time can occur if it is taken late at night. Side
effects are few. Even large doses do not markedly depress respiration.
Currently, it is one of the most commonly prescribed hypnotics.
Dose: 5–10 mg (max 20 mg) at
bedtime; ½ dose in elderly and liver
disease patients.
NITREST, ZOLDEM, DEM
5, 10 mg tabs.
Zaleplon This is the shortest acting of the newer non-BZD hypnotics that selectively act
on a subset of BZD receptors containing the α1 subunit which appear
to mediate the hypnotic action. It is rapidly absorbed; oral bioavailability is
~30% due to first pass metabolism; is rapidly cleared by hepatic metabolism with
a t½ of 1 hour. No active metabolite is produced. As such it is effective only
in sleep-onset insomnia; does not prolong total sleep time or reduce the number
of awakenings. Because of brevity of action, it can be taken late at night
(> 4 hour before waking time) without causing morning sedation.
Surprisingly, despite very short action, no daytime anxiety or rebound insomnia
has been observed. No tolerance or dependence has been reported and hypnotic
effect does not fade on nightly use. However, its use should be limited to 1–2
weeks. The hypnotic efficacy of zaleplon is rated similar to zolpidem. Like the
latter, effect on sleep stages and REM sleep are less than that of BZDs.
Dose: 5–10 mg (max 20 mg) at
bed time.
ZAPLON, ZALEP, ZASO 5,
10 mg tabs.
Uses
Currently, BZDs are
one of the most frequently prescribed drugs. They have also been combined with
many other categories of drugs with a view to improve efficacy by relieving
attendant anxiety.
1. As Hypnotic
A hypnotic should not
be casually prescribed for
every case of insomnia. Understanding the cause of insomnia and use of a
variety of other measures can avoid unnecessary hypnotic medication. When
indicated, BZDs or the newer non-BZDs like zolpidem, zaleplon, zopiclone are
the hypnotic of choice. A wide range of compounds have been developed to suit
specific requirements. Some important points are outlined below:
A hypnotic may be used
to shorten sleep latency, to reduce nocturnal awakenings, or to provide
anxiolytic effect the next day when insomnia is accompanied with marked element
of anxiety.
In the use of
hypnotics, consideration must be given to onset and duration of action of the
drug. The most suitable pharmacokinetic profile drug should be chosen for a given
case.
Impaired performance
the next day is largely related to the dose and pharmacokinetic profile of the
drug. The next day effects are either due to prolonged sedation (longer acting drugs)
or rebound anxiety (shorter acting drugs).
Any hypnotic (probably
except zolpidemlike drugs) becomes useless after regular use for a few days;
may actually be harmful.
Though effect of drugs on the EEG stages of sleep, including REM
sleep, could be physiologically relevant, most important is the subject’s own
assessment of having slept restfully and with no impairment the following day.
This probably correlates more closely with effect of the hypnotic on the cyclic alternating pattern (CAP) of sleep.
Insomnia arises under a variety of circumstances. It could be a long-term
(monthsyears), shortterm (weeks) or transient (a day or two, mostly
situational) problem.
Chronic Insomnia (> 3 weeks) Uncertainty exists about the use of
hypnotics in this situation. The patient may have a personality disorder, but
often there is no specific stress factor; may have used hypnotics for long
periods, may be alcoholic or have some somatic disease—gastroesophageal reflux,
pain, COPD, etc. Measures like aerobic exercise, training at mental relaxation,
avoiding anxiety about past/future performance at bedtime, attempting sleep
when sleepiness is maximum, avoiding napping at daytime, coffee/ alcohol
restriction, treatment of concurrent somatic illness, psychotherapy and
controlled sleep curtailment may succeed. Good nightly sleep improves the
quality of daytime wakefulness. Patients of obstructive sleep apnoea have poor
sleep and feel sleepy during the day. All hypnotics aggravate apnoea and are
contraindicated.
Intermittent use of a hypnotic, say once every 3 days, may be
tried. Risk of tolerance and abuse are maximum among chronic insomniacs. A
slowly eliminated drug is preferable because rebound insomnia and withdrawal
symptoms are least marked with these drugs.
Short-term Insomnia (3–21 days) Emotional problem (occupational
stress, bereavement) and physical illness are the usual causes. Patient may
have induction
difficulty or may be waking up early. Cautious use of low doses of an appropriate
drug for the type of sleep disturbance may be made. Generally a hypnotic, free
of residual effects should be selected, but when anxiety is a dominant feature,
a BZD whose action extends into the next day may be better. Short acting drugs
are preferable in the elderly. Intermittent hypnotic use should be limited to
2–3 weeks.
Transient Insomnia (1–3 days) Due to alterations in the circumstances
of sleep, e.g. on an overnight train, new place, unusual pattern of work, shift
workers, intercontinental travel–jetlag, etc. A rapidly eliminated hypnotic or
one with marked distribution is to be preferred to avoid residual effects the next
morning. However, night before surgery—a long acting drug is better.
2. Other uses
•
As anxiolytic and for daytime sedation (see Ch. No. 33).
• As anticonvulsant, especially emergency
control of status epilepticus, febrile convulsions, tetanus, etc. (see Ch. No. 30).
•
As centrally acting muscle relaxant (see Ch. No. 25).
•
For preanaesthetic medication, i.v. anaesthesia
and conscious sedation (see Ch. No.
27).
• Before ECT, electrical cardioversion of arrhythmias,
cardiac catheterization, endoscopies, in obstetrics and many minor procedures—
diazepam i.v. has gained popularity because of its calmingamnesicanalgesic and
muscle relaxant properties and relative safety.
•
Alcohol withdrawal in dependent subjects.
•
Along with analgesics, NSAIDs, spasmolytics, antiulcer
and many other drugs.
Fixed dose
combinations of sedative/hypnotic/anxiolytic drugs with analgesicantipyretics
has been banned in India.
