Antimanic (Mood Stabilizing) Drugs
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs Used In Mental Illness: Antipsychotic And Antimanic Drugs
Lithium is a small monovalent cation. In 1949, it was found to be sedative in animals and to exert beneficial effects in manic patients.
ANTIMANIC (MOOD STABILIZING) DRUGS
Lithium Carbonate
Lithium is a small monovalent cation. In 1949, it was found to
be sedative in animals and to exert beneficial effects in manic patients.
In the 1960s and 1970s
the importance of maintaining a narrow range of serum lithium concentration was
realized and unequivocal evidence of its efficacy was obtained. Lithium is a
drug of its own kind to suppress mania and to exert a prophylactic effect in
bipolar manic depressive illness (MDI) at doses which have no overt CNS
effects. Lithium is established as the standard antimanic and mood stabilizing
drug. Over the past 2 decades, several anticonvulsants and antipsychotics have
emerged as alternatives to lithium with comparable efficacy.
Actions And Mechanism
1. CNS
Lithium has practically
no acute effects in normal individuals
as well as in MDI patients. It is neither sedative nor euphorient; but on
prolonged administration, it acts as a mood stabiliser in bipolar disorder.
Given to patients in acute mania, it gradually suppresses the episode taking
1–2 weeks; continued treatment prevents cyclic mood changes. The markedly
reduced sleep time in manic patients is normalized.
The mechanism of
antimanic and mood stabilizing action of lithium is not known. It has been
argued that:
a) Li+ partly replaces
body Na+ and is nearly equally distributed inside and outside the cells
(contrast Na+ and K+); this may affect ionic fluxes across brain cells or
modify the property of cellular membranes.
b) Lithium has been
found to decrease the release of NA and DA in the brain of treated animals
without affecting 5HT release. This may correct any imbalance in the turnover
of brain monoamines.
c) The above
hypothesis cannot explain why Li+ has no effect on people not suffering from
mania.
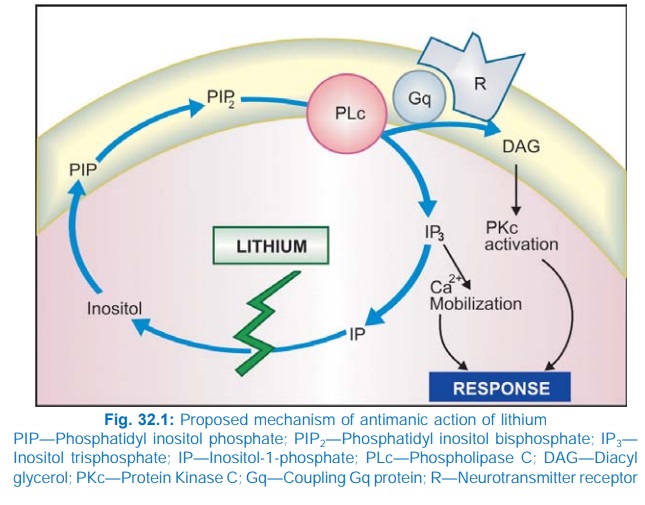
An attractive
hypothesis has been put forward based on the finding that lithium inhibits
hydrolysis of inositol1phosphate by inositol monophosphatase. As a result, the
supply of free inositol for regeneration of membrane phosphatidylinositides,
which are the source of IP3 and DAG, is reduced (Fig. 32.1). The
hyperactive neurones involved in the manic state may be preferentially
affected, because supply of inositol from extracellular sources is meagre.
Thus, lithium may ignore normally operating receptors, but ‘search out’ and
selectively, though indirectly, dampen signal transduction in the overactive
ones.
2. Other Actions
Lithium inhibits the
action of ADH on distal tubules
and causes a diabetes insipidus like state.
It has some insulin-like
action on glucose metabolism.
Leukocyte count is
increased by lithium therapy. Lithium reduces thyroxine synthesis by interfering
with iodination of tyrosine.
Pharmacokinetics And Control Of Therapy
Lithium is slowly but
well absorbed orally and is neither protein bound nor metabolized. It first
distributes in the extracellular water and then gradually enters cells and
slowly penetrates into the CNS, ultimately attaining a rather uniform distribution
in total body water; apparent volume of distribution at steady state averages
0.8 L/kg.
Lithium is handled by
the kidney in much the same way as Na+. Most of the filtered Li+ is reabsorbed
in the proximal convoluted tubule. When Na+ is restricted, a larger fraction of
filtered Na+ is reabsorbed, so is Li+. After a single dose of Li+ urinary
excretion is rapid for 10–12 hours, followed by a much slower phase lasting
several days. The t½ of the latter phase is 16–30 hours. Renal clearance of
lithium is 1/5 of creatinine clearance. On repeated medication steady state plasma
concentration is achieved in 5–7 days. Levels are higher in older patients and
in those with renal insufficiency.
There is marked
individual variation in the rate of lithium excretion. Thus, with the same
daily dose, different individuals attain widely different plasma
concentrations. However, in an individual the clearance remains fairly
constant. Since the margin of safety is narrow, monitoring of serum lithium
concentration is essential for optimal therapy. Serum lithium level is measured
12 hours after the last dose to reflect the steady state concentration; 0.5–0.8
mEq/L is considered optimum for maintenance therapy in bipolar disorder, while
0.8–1.1 mEq/L is required for episodes of mania. Toxicity symptoms occur frequently
when serum levels exceed 1.5 mEq/L.
Peaks in plasma
lithium level over and above the steadystate level occur after every dose.
Divided daily dosing in 2–4 portions is needed to avoid high peaks. Lithium is
excreted in sweat and saliva also. Lithium is secreted in breast milk. Mothers
on lithium should not breastfeed.
Adverse Effects
Side effects are
common, but are mostly tolerable.
Toxicity occurs at levels only marginally higher than therapeutic levels.
1. Nausea, vomiting
and mild diarrhoea occur initially, can be minimized by starting at lower
doses.
2. Thirst and polyuria
are experienced by most, some fluid retention may occur initially, but clears
later.
3. Fine tremors and
rarely seizures are seen even at therapeutic concentrations.
4. CNS toxicity
manifests as plasma concentration rises—coarse tremors, giddiness, ataxia,
motor incoordination, nystagmus, mental confusion, slurred speech, hyperreflexia.
Overdose symptoms are regularly seen at plasma concentration above 2 mEq/L. In
acute intoxication these symptoms progress to muscle twitchings, drowsiness,
delirium, coma and convulsions. Vomiting, severe diarrhoea, albuminuria, hypotension
and cardiac arrhythmias are the other features.
Treatment
It is symptomatic.
There is no specific antidote.
Osmotic diuretics and sod. bicarbonate infusion promote Li+ excretion.
Haemodialysis is indicated if serum levels are > 4 mEq/L.
1. On long-term use, some patients develop renal diabetes
insipidus. Goiter has been reported in about 4%. This is due to interference
with iodination of tyrosine → decreased thyroxine synthesis. However,
hypothyroidism is rare. Thyroxine administration inhibits TSH and reverses
thyroid enlargement.
2. Lithium is contraindicated during pregnancy: foetal goiter
and other congenital abnormalities, especially cardiac, can occur; the newborn
is often hypotonic.
3. Lithium is contraindicated in sick sinus syndrome.
Interactions
1.
Diuretics (thiazide, furosemide) by causing
Na+ loss promote proximal tubular reabsorption of Na+ as well as Li+ → plasma levels of
lithium rise.
2.
Tetracyclines, NSAIDs and ACE inhibitors can
also cause lithium retention.
3.
Lithium reduces pressor response to NA.
4.
Lithium tends to enhance insulin/sulfonylurea
induced hypoglycaemia.
5.
Succinylcholine and pancuronium have produced
prolonged paralysis in lithium treated patients.
6.
Neuroleptics, including haloperidol, have been
frequently used along with lithium without problem; sometimes, the combination
of haloperidol and lithium produces marked tremor and rigidity. The neuroleptic
action appears to be potentiated by lithium.
Use
Lithium is used as its carbonate salt because this is less hygroscopic
and less gastric irritant than LiCl or other salts. It is converted into
chloride in the stomach.
LICAB, LITHOSUN 300 mg
tab, 400 mg SR tab.
It is generally started at 600 mg/day and gradually increased to
yield therapeutic plasma levels; mostly 600– 1200 mg/day is required.
1. Acute Mania (inappropriate
cheerfullness or irritability, motor
restlessness, nonstop talking, flight of ideas, little need for sleep and
progressive loss of contact with reality; sometimes violent behaviour): though
lithium is effective, response is slow and control of plasma levels is
difficult during the acute phase. Most prefer to use a neuroleptic, generally
by i.m. route, with or without a potent BZD like clonazepam/ lorazepam, and
start lithium after the episode is under control. Maintenance lithium therapy
is generally given for 6–12 months to prevent recurrences.
2. Prophylaxis In Bipolar Disorder
Lithium has proven efficacy
in bipolar disorder: is gradually introduced and maintained at plasma concentration
between 0.5–0.8 mEq/L. Such treatment lengthens the interval between cycles of
mood swings: episodes of mania as well as depression are attenuated, if not
totally prevented. Bipolar disorder is the most common and definite indication
of lithium. Risks and benefits of prolonged (almost indefinite) lithium therapy
are to be weighed in individual cases. Patients have been maintained on lithium
therapy for over a decade. Most cases relapse when lithium is discontinued.
Withdrawal, when attempted should be gradual over months.
Recurrent unipolar depression also responds to
lithium therapy. Combination of antidepressant + lithium is often used initially,
and lithium alone is continued in the maintenance phase.
3. Lithium is being
sporadically used in many other recurrent
neuropsychiatric illness, cluster headache and as adjuvant to
antidepressants in resistant nonbipolar major
depression.
4. Cancer chemotherapy
induced leukopenia and agranulocytosis: Lithium may hasten the
recovery of leukocyte count.
5. Inappropriate ADH secretion syndrome: Lithium tends to
counteract water retention, but is not dependable.
Alternatives To Lithium
Approximately 50% patients
of mania and bipolar disorder (especially rapidly cycling cases) show
incomplete or poor response to lithium. Many do not tolerate it, or are at
special risk of toxicity.
Alternatives are:
1. Carbamazepine
Soon after its
introduction as antiepileptic, carbamazepine
(CBZ) was found to prolong remission in bipolar disorder. Its efficacy in mania
and bipolar disorder has now been confirmed and is rated almost equal to
lithium. Patients who relapse on lithium therapy or those prone to rapid
cycling of mood state do better on combined lithium + CBZ treatment. Since CBZ
therapy is easier to manage and better tolerated than lithium, it is being
increasingly used as firstline/adjunctive treatment for acute mania as well as
bipolar illness. The dose and effective plasma concentration range is the same
as for treatment of epilepsy. However, its efficacy in long-term prophylaxis of
bipolar illness and suicides is less well established.
2. Sodium Valproate
A reduction in manic relapses is noted when valproate is used in
bipolar disorder. It is now a first line treatment of acute mania in which high
dose valproate acts faster and is an alternative to antipsychotic ±
benzodiazepine. It can be useful in those not responding to lithium or not
tolerating it. Patients with rapid cycling pattern may particularly benefit
from valproate therapy. A combination of lithium and valproate may succeed in
cases resistant to monotherapy with either drug. Valproate has a favourable
tolerability profile. Dosage guidelines are the same as for epilepsy.
3. Lamotrigine
This newer anticonvulsant is now an approved drug
for bipolar disorder, but is not recommended for acute mania. It is especially
useful in rapidly cycling bipolar depression. Randomized trials have
demonstrated its efficacy, both as monotherapy as well as adjuvant to lithium.
It carrys minimal risk of inducing mania. The tolerability profile of
lamotrigine is favourable.
4. Topiramate
Few open studies have found it to be useful as adjunctive therapy of bipolar
disorder, but efficacy needs to be established.
Gabapentin also has shown some
prophylactic effect in bipolar
disorder.
5. Atypical antipsychotics:
Olanzapine, risperidone
and newer atypical antipsychotics aripiprazole, quetiapine, with or without a
BZD, are now the first line drugs for control of acute mania, except cases
requiring urgent parenteral therapy, for which the older neuroleptics are still
the most effective.
Olanzapine is also
approved for maintenance therapy of bipolar disorder. Because it carrys a low
risk of inducing extrapyramidal side effects or agranulocytosis, it is being
increasingly used as adjuvant/alternative to lithium for prophylaxis of cyclic
mood swings. The usefulness of other atypical antipsychotics as prophylactic in
bipolar illness is not established, but there are reports of beneficial effect.
Related Topics
