Antihypertensive Drugs
| Home | | Pharmacology |Chapter: Essential pharmacology : Antihypertensive Drugs
These are drugs used to lower BP in hypertension. Hypertension is a very common disorder, particularly past middle age. It is not a disease in itself, but is an important risk factor for cardiovascular mortality and morbidity.
ANTIHYPERTENSIVE DRUGS
These are drugs used
to lower BP in hypertension. Hypertension is a very common disorder, particularly
past middle age. It is not a disease in itself, but is an important risk factor
for cardiovascular mortality and morbidity. The cutoff manometric reading
between normotensives and hypertensives is arbitrary. For practical purposes
‘hypertension’ could be that level of BP at or above which long-term antihypertensive
treatment will reduce cardiovascular mortality. The JNC 7* (2003) and WHOISH@
guidelines (2003) have defined it to be 140 mm Hg systolic and 90 mm Hg
diastolic, though risk appears to increase even above 120/80 mm Hg. Epidemiological
studies have confirmed that higher the pressure (systolic or diastolic or both)
greater is the risk of cardiovascular disease.
Majority of cases are
of essential (primary) hypertension, i.e. the cause is not known. Sympathetic
and renin-angiotensin systems may or may not be overactive, but they do
contribute to the tone of blood vessels and c.o. in hypertensives, as they do
in normotensives. Many antihypertensive drugs interfere with these regulatory
systems at one level or the other. Antihypertensive drugs, by chronically
lowering BP, may reset the barostat to function at a lower level of BP.
Antihypertensive drug
therapy has been remarkably improved in the last 50 years. Different classes of
drugs have received prominence with passage of time in this period. Before 1950
hardly any effective and tolerated antihypertensive was available. Veratrum and Sod. thiocyanate could
lower BP, but were toxic and difficult to
use. The ganglion blockers developed
in the 1950s were effective, but inconvenient. Reserpine was a breakthrough, but produced mental depression. The
therapeutic potential of hydralazine
could not be tapped fully because of marked side effects when it was used
alone. Guanethidine introduced in
1961 was an improvement on ganglion blockers.
The antihypertensives of the 1960– 70s were methyldopa,
β blockers, thiazide and high ceiling diuretics and clonidine.
The status of β
blockers and diuretics
was consolidated in the 1970s and selective α1 blocker prazosin broke new grounds. The
antihypertensives of the 1980–90s are angiotensin II converting enzyme (ACE) inhibitors and calcium channel blockers. Angiotensin
receptor blockers (losartan) are the
latest antihypertensives. With the development of many types of drugs, delineation
of their long-term benefits and complications, and understanding of the
principles on which to combine them, hypertension can now be controlled in most
cases with minimum discomfort.
Classification
1. Diuretics
Thiazides: Hydrochlorothiazide, Chlorthalidone, Indapamide
High ceiling: Furosemide, etc.
K+ Sparing: Spironolactone,
Amiloride
2. ACE
inhibitors
Captopril, Enalapril, Lisinopril, Perindopril, Ramipril,
Fosinopril, etc.
3. Angiotensin
(AT1 receptor) blockers
Losartan, Candesartan, Irbesartan, Valsartan, Telmisartan
4. Calcium
channel blockers
Verapamil, Diltiazem, Nifedipine, Felodipine, Amlodipine,
Nitrendipine, Lacidipine, etc.
5. β Adrenergic blockers
Propranolol,
Metoprolol, Atenolol, etc.
6. β + α Adrenergic blockers
Labetalol, Carvedilol
7. α Adrenergic blockers
Prazosin, Terazosin, Doxazosin Phentolamine, Phenoxybenzamine
8. Central
sympatholytics
Clonidine, Methyldopa
9. Vasodilators
Arteriolar: Hydralazine,
Minoxidil, Diazoxide
Arteriolar + venous: Sodium nitroprusside
Adrenergic neurone blockers (Reserpine, Guanethidine, etc.) and
ganglion blockers (Pentolinium, etc.) are only of historical importance, though
reserpine is still marketed.
DIURETICS
Diuretics have been the standard antihypertensive drugs over the
past 4 decades, though they do not lower BP in normotensives. Their
pharmacology is described in Ch. No. 41.
Thiazides and related drugs (chlorthalidone, etc.) are the diuretic of choice in
uncomplicated hypertension. The proposed mechanism of antihypertensive action
is:
1.
Initially, the diuresis reduces plasma and
e.c.f. volume by 5–15% → decreased c.o.
2.
Subsequently, compensatory mechanisms operate
to almost regain Na+ balance and plasma volume; c.o. is restored, but the fall
in BP is maintained by a slowly developing reduction in t.p.r.
3.
The reduction in t.p.r. is most probably an
indirect consequence of a small (~5%) persisting Na+ and volume deficit.
Decrease in intracellular Na+ concentration in the vascular smooth muscle may
decrease stiffness of vessel wall, increase their compliance and dampen
responsiveness to constrictor stimuli (NA, AII). Similar effects are produced
by salt restriction; antihypertensive action of diuretics is lost when salt
intake is high. A mild slowly developing vasodilator action of thiazides due to
opening of smooth muscle K+ATP channels and
hyperpolarization has been proposed, but does not appear to be real.
The fall in BP develops
gradually over 2–4 weeks. During long-term treatment with thiazides, the heart
rate and c.o. are unaffected, while t.p.r. is reduced despite compensatory
increase in plasma renin activity, which confirms persisting Na+ deficit. They
have no effect on capacitance vessels, sympathetic reflexes are not impaired:
postural hypotension is rare. Thiazides are mild antihypertensives, average
fall in mean arterial pressure is ~10 mm Hg. They are effective by themselves
in ~ 30% cases (mostly low grade hypertension) but they potentiate all other
antihypertensives (except DHPs) and prevent development of tolerance to these
drugs by not allowing expansion of plasma volume. They are more effective in
the elderly and maximal antihypertensive efficacy is reached at doses equivalent
to 25 mg of hydrochlorothiazide/day, though higher doses produce greater
diuresis.
High Ceiling Diuretics Furosemide, the prototype
of this class, is a strong diuretic, but the antihypertensive efficacy does not
parallel diuretic potency. Furosemide is a weaker antihypertensive than thiazides:
fall in BP is entirely dependent on reduction in plasma volume and c.o. The
explanation to this paradox may lie in its brief duration of action. The
natriuretic action lasting only 4–6 hr after the conventional morning dose is
followed by compensatory increase in proximal tubular reabsorption of Na+. The
Na+ deficient state in vascular smooth muscle may not be maintained round-the-clock.
The t.p.r. and vascular responsiveness are not reduced. Moreover, the high ceiling
diuretics are more liable to cause fluid and electrolyte imbalance, weakness
and other side effects. They are indicated in hypertension only when it is
complicated by:
·
Chronic renal failure: thiazides are
ineffective, both as diuretics and antihypertensives.
·
Coexisting refractory CHF.
·
Resistance to combination regimens containing
a thiazide, or marked fluid retention due to use of potent vasodilators.
Desirable Properties Of Diuretics
As Antihypertensives Are:
ü Once a day dosing and
flat doseresponse curve permitting simple standardized regimens.
ü No fluid retention, no
tolerance.
ü Low incidence of
postural hypotension and relative freedom from side effects, especially CNS,
compared to sympatholytics.
ü Effective in isolated
systolic hypertension (ISH).
ü Lessened risk of hip
fracture in the elderly due to hypocalciuric action of thiazides.
ü Low cost.
Current Status Of Diuretics As Antihypertensives
The popularity of diuretics as antihypertensive has had ups and
downs. In the 1960–70s they were almost routinely prescribed alone or in
combination to nearly all hypertensive patients. The usual dose used was
hydrochlorothiazide 50 mg/day or equivalent. Soon a number of drawbacks were
highlighted:
·
Hypokalaemia—muscle pain, fatigue and loss of
energy.
·
Erectile dysfunction in males.
· Carbohydrate intolerance: due to inhibition of
insulin release (probably secondary to K+ depletion which interferes with
conversion of proinsulin to insulin), precipitation of diabetes. Dyslipidemia:
rise in total and LDL cholesterol and triglycerides with lowering of HDL. This
could increase atherogenic risk, but no direct evidence has been obtained.
·
Hyperuricaemia: by inhibiting urate excretion—increased
incidence of gout.
· Increased incidence of sudden cardiac death:
attributed to episodes of torsades de
pointes and ischaemic ventricular fibrillation precipitated by
hypokalaemia.
Consequently,
prescribing of diuretics fell.
Over the past 20 years
thiazides have been used at lower doses (12.5–25 mg/day hydrochlorothiazide or
equivalent) alone and in combination with a K+ sparing diuretic.
The multiple risk
factor intervention trial (1982), the Medical research council trial (1987,
1992), the systolic hypertension in the elderly programme (SHEP, 1991) and a
case control study (1994) demonstrated that increased incidence of death
associated with thiazide diuretic use in the elderly was dosedependent, and
that 25 mg/day hydrochlorothiazide (or equivalent) yielded the best benefitrisk
ratio. Favourable results obtained with ≤ 25 mg/day in the above
and subsequent studies, including ALLHAT (2002) and a metaanalysis (2003) have
reinstated thiazide diuretics as the first choice antihypertensive.
Findings with low dose thiazide therapy are:
·
Though serum K+ falls a little, significant
hypokalaemia does not occur.
· Continuous ECG recording studies have failed
to document increased incidence of arrhythmias during lowdose thiazide therapy.
· Impairment of glucose tolerance or increase in
serum cholesterol or hyperuricaemia over long-term are unlikely.
· Whereas earlier data had failed to document reduction
in the incidence of MI with thiazides, analysis of recent trials has found them
to reduce fatal and nonfatal MI by 27–44%. The incidence of stroke is reduced
by 31–49%. Overall mortality and morbidity is reduced in long-term trials.
· Though not as effective as ACE inhibitors,
some recent trials in mild to moderate hypertension have found thiazides to
reduce left ventricular mass.
The JNC 7 recommends
instituting low dose (12.5–25 mg) thiazide therapy, preferably with added K+
sparing diuretic, as a first choice treatment of essential hypertension,
especially in the elderly. Higher doses are neither more effective nor safe. If
the low dose (25 mg/day) fails to reduce BP to desired level, another antihypertensive
should be added, rather than increasing dose of the diuretic. However, in the
treatment of severe hypertension when potent vasodilators/ sympatholytics have
induced fluid retention, higher dose of thiazide or a loop diuretic may be
appropriate. Not withstanding the above, there are subsets of patients in whom
other antihypertensives are more suitable. Some patients complain impairment of
quality of life with diuretics.
Potassium Sparing Diuretics Spironolactone or amiloride themselves lower BP slightly, but
they are used only in conjunction with a thiazide diuretic to prevent K+ loss
and to augment the antihypertensive action.
Indapamide
It is a mild diuretic, chemically related to
chlorthalidone; reduces BP at doses which cause little diuresis. Electrolyte
disturbances and K+ loss are minimal at antihypertensive doses. In poststroke
patients, indapamide, with or without ACE inhibitor, reduces the risk of
further stroke. It probably has additional vasodilator action exerted through alteration
of ionic fluxes across vascular smooth muscle cell.
Indapamide is well absorbed orally, has an elimination t½ of 16
hr. Single daily dose (2.5 mg) is enough.
LORVAS, NATRILIX 2.5 mg tab, NATRILIXSR 1.5 mg SR tab
It is well tolerated: side effects are minor g.i. symptoms and
fatigue. Hypokalaemia is infrequent.
ANGIOTENSIN CONVERTING ENZYME (ACE) INHIBITORS
The ACE inhibitors are one of the first choice drugs in all
grades of essential as well as renovascular hypertension (except those with bilateral
renal artery stenosis). Most patients require relatively lower doses (enalapril
2.5–10 mg/day or equivalent) which are well tolerated.
Used alone they
control hypertension in ~50% patients, and addition of a diuretic/β blocker extends
efficacy to ~90%. Because of supra-additive synergism, only a low dose of
diuretic (12.5 mg of hydrochlorothiazide, rarely 25 mg) needs to be added. Of
particular mention are their renal blood flow improving action, their potential
to retard diabetic nephropathy and their capacity to regress left
ventricular/vascular hypertrophy. They are the most appropriate
antihypertensives in patients with diabetes, nephropathy (even nondiabetic),
left ventricular hypertrophy, CHF, angina and post MI cases. Several large
prospective studies including AIRE (1993), HOPE (2000), ALLHAT (2002) have
confirmed the antihypertensive and cardioprotective effects of ACE inhibitors.
They appear to be more effective in younger (< 55 year) hypertensives than
in the elderly. Dry persistent cough is the most common side effect requiring
discontinuation of ACE inhibitors.
ANGIOTENSIN RECEPTOR BLOCKERS
The pharmacology of losartan and other angiotensin receptor
blockers (ARBs) is described on p. 488. In a dose of 50 mg/day losartan is an
effective antihypertensive. Action manifests early and progresses to peak at
2–4 weeks. Addition of 12.5 mg/day hydrochlorothiazide further enhances the fall
in BP. The newer ARBs—valsartan, candesartan, irbesartan and telmisartan have been
shown to be as effective antihypertensives as ACE inhibitors, while losartan
may be somewhat weaker than high doses of ACE inhibitors. ARBs are remarkably
free of side effects. Because they do not increase kinin levels, the ACE
inhibitor related cough is not encountered. Angioedema, urticaria and taste
disturbance are also rare. Though effects of ACE inhibitors and ARBs are not
identical, the latter have all the metabolic and prognostic advantages of ACE
inhibitors.
Several interventional
endpoint reduction trials like LIFE (2002), VALUE (outcomes in hypertensive
patients with valsartan or amlodipine, 2004), SCOPE (study on cognition and
prognosis in the elderly; stroke prevention with candesartan in elderly with
isolated systolic hypertension, 2004), JLIGHT (Japanese losartan therapy
intended for global renal protection in hypertensive patients, 2004) have
attested to the favourable effects of ARBs on morbidity and mortality in
hypertensive patients.
The value of combining
ARBs with ACE inhibitors is discussed on p. 489.
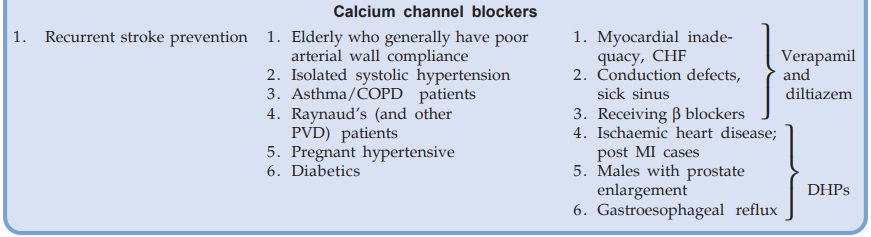
CALCIUM CHANNEL BLOCKERS
Calcium channel
blockers (CCBs) are another class of first line antihypertensive drugs. Their
pharmacology is described in Ch. No. 39. All 3 subgroups of CCBs, viz. dihydropyridines (DHPs, e.g.
amlodipine), phenylalkylamine (verapamil) and benzothiazepine (diltiazem) are
equally efficacious antihypertensives. They lower BP by decreasing peripheral
resistance without compromising c.o. Despite vasodilatation, fluid retention is
insignificant.
Ankle edema that occurs
in some patients is due to increased hydrostatic pressure across capillaries of
the dependent parts as a result of reflex constriction of post capillary vessels
in these vascular beds.
The onset of
antihypertensive action is quick. With the availability of long acting
preparations, most agents can be administered once a day. Monotherapy with CCBs
is effective in ~ 50% hypertensives; their action is independent of patient’s
renin status, and they may improve arterial compliance. Other advantages of CCBs
are:
·
Do not compromise haemodynamics: no impairment
of physical work capacity.
·
No sedation or other CNS effects; cerebral perfusion
is maintained.
· Not contraindicated in asthma, angina
(especially variant) and PVD patients: may benefit these conditions.
·
Do not impair renal perfusion.
·
Do not affect male sexual function.
·
No deleterious effect on plasma lipid profile,
uric acid level and electrolyte balance.
·
Shown to have no/minimal effect on quality of
life.
· No adverse foetal effects; can be used during
pregnancy (but can weaken uterine contractions during labour).
In the past few years
large amount of data from controlled trials (HINT, TRENT, SPRINT I, II) and metaanalysis
has consistently indicated increased mortality/reinfarction in patients treated
with standard nifedipine (or other short-acting DHP) formulations. This
increase in mortality is doserelated. Worsening of unstable angina and CHF has
also been noted. The CCBs do not decrease venous return. DHPs may even increase
it and jeopardise haemodynamics in patients with diastolic dysfunction. DHPs
(especially short-acting) also tend to increase HR and c.o. by invoking reflex
sympathetic stimulation. The increased mortality among coronary heart disease
patients has been attributed to repeated surges of adrenergic discharge and
marked swings of BP attending each dose of rapidly acting DHP. However, this
risk cannot be extrapolated to verapamil/ diltiazem as broughtout by DAVIT I,
II and other controlled studies, as well as to slow acting DHPs (amlodipine
type) including nifedipine GITS (gastrointestinal therapeutic system).
The Systolic
hypertension in Europe (Syst-EUR) trial has shown that nitrendipine (long-acting
DHP) reduces cardiovascular morbidity and mortality in elderly hypertensives.
The Hypertension optimal treatment (HOT), and Sweedish trial in old patients
with hypertension-2 (STOP-2) studies
have also found CCBs equi-effective as diuretics/β blockers/ACE
inhibitors in reducing cardiovascular/total mortality. No excess mortality with
the use of amlodipine in post MI and acute coronary syndrome patients has been
noted in the ALL HAT (2002) study. On the other hand, CCBs do not afford
survival benefit in post MI patients as β blockers, ACE
inhibitors or low dose thiazides do. CCBs are also not as effective in
suppressing left ventricular hypertrophy (a major risk factor in ischaemic
heart disease) as ACE inhibitors.
The JNC 7 have considered CCBs to be less suitable for
monotherapy in hypertensives with no other risk factors, because they appear to
afford less prognostic benefits than thiazides, β blockers and ACE
inhibitors/ARBs. However, CCBs are still widely used as one of the first line
monotherapy options because of their high efficacy and excellent tolerability.
They are preferred in the elderly hypertensive. Also there is convincing
evidence of their stroke preventing potential (syst EUR, ALLHAT studies). The long-acting
DHPs are next to ACE inhibitors in reducing albuminuria and slowing disease
progression in hypertensive/diabetic nephropathy. They are the most useful
antihypertensives in cyclosporine induced hypertension in renal transplant
recipients.
Use of rapid acting oral nifedipine for urgent BP lowering in
hypertensive emergencies is out moded. In fact, there is currently no
therapeutic indication for rapid and short-acting oral DHPs in hypertension.
Other concerns in the use of CCBs as antihypertensive are:
· The negative inotropic/dromotropic action of
verapamil/diltiazem may worsen CHF and cardiac conduction defects (DHPs are
less likely to do so).
· By their smooth muscle relaxant action, the
DHPs can worsen gastroesophageal reflux.
· CCBs (especially DHPs) may accentuate bladder voiding
difficulty in elderly males.
β-ADRENERGIC BLOCKERS
The pharmacology and mechanism of antihypertensive action of β blockers is described
in Ch. No. 10. They are mild antihypertensives; do not significantly lower BP
in normotensives. Used alone they suffice in 30–40% patients—mostly mild to
moderate cases. In the large majority of the rest, they can be usefully
combined with other drugs.
The hypotensive response to β blockers develops
over 1–3 weeks and is well sustained. Despite short and differing plasma half
lives, the antihypertensive action of most β blockers is
maintained over 24 hr with a single daily dose.
All β blockers,
irrespective of associated properties, exert similar antihypertensive effect.
Drugs with intrinsic sympathomimetic activity (ISA) cause less reduction of HR
and c.o. but lower vascular resistance by β2 agonism. The nonselective
β blockers slightly
reduce renal blood flow and g.f.r., but this is minimal in the β1 selective ones and
those with ISA.
There are several
contraindications to β blockers, including cardiac, pulmonary and
peripheral vascular disease. The nonselective β blockers have an unfavourable
effect on lipid profile (raise triglyceride level and LDL/HDL ratio). They have
also fared poorly on quality of life parameters like decreased work capacity,
fatigue, loss of libido and subtle cognitive effects (forgetfulness, low
drive), nightmares and increased incidence of antidepressant use. However, most
of these drawbacks are minimized in the β1 selective agents and in
those which penetrate brain poorly. Thus, there are several reasons
to prefer a β1 selective hydrophilic
drug like atenolol over propranolol.
Because of absence of
postural hypotension, bowel alteration, salt and water retention; a low
incidence of side effects, low cost; once a day regimen and cardioprotective
potential, β blockers continue to
be among the first choice drugs recommended by JNC 7 and WHOISH, especially for
relatively young nonobese hypertensives, those prone to psychological stress or
those with ischaemic heart disease—particularly postinfarction. β blockers and ACE
inhibitors are the most effective drugs for preventing sudden cardiac death in
postinfarction patients; all cause mortality has been lowered in long-term
trials. Hypertensives with stable heart failure should be treated with a β blocker that has been
shown to be effective in retarding CHF progression (metoprolol/bisoprolol/carvedilol)
along with an ACE inhibitor/ARB (CIBIS, 1999; MERITHF, 1999, COPERNICUS, 2002
studies). β blockers are considered
less effective and less suitable for the older hypertensive. The LIFE (2002)
and ALLHAT (2002) trials have found β blockers to be inferior to lowdose thiazide
or ACE inhibitor/ARB (losartan) or a combination of these in preventing stroke,
as well as in diabetic patients. As monotherapy, ACE inhibitors/ARBs and CCBs
appear to compromise quality of life less than β blockers. Rebound
hypertension has occurred on sudden discontinuation of β blockers.
β+α ADRENERGIC BLOCKERS
Labetalol
It is a combined α and β blocker; reduces t.p.r. and acts faster than pure β blockers. It has been
used i.v. for rapid BP reduction in cheese reaction, clonidine withdrawal, etc.
Oral labetalol therapy is restricted to moderately severe hypertension not responding
to pure β blocker. Side effects
of both α blocker and β blocker occur with
it.
Carvedilol
This nonselective β + selective α1 blocker produces vasodilatation and has additional
antioxidant/ free radical scavenging properties. Whether these ancilliary
properties confer any superiority is not known. It has also been used in CHF.
Side effects are similar to labetalol; liver enzymes may rise in some.
α-ADRENERGIC BLOCKERS
Prazosin
This prototype
selective α1 antagonist dilates
both resistance and capacitance vessels; effect on the former predominating.
The haemodynamic effects—reduction in t.p.r. and mean BP with only slight
decrease in venous return and c.o. are similar to that produced by a direct
acting vasodilator. However, there is little reflex cardiac stimulation and
renin release during long-term therapy. Tachycardia does not compensate for the
fall in BP, because release inhibitory α2 (presynaptic)
receptors are not blocked: autoregulation of NA release remains intact. It
probably decreases central sympathetic tone also.
Renal blood flow and g.f.r. are maintained but fluid retention
may attend hypotension. Cardiovascular reflexes are not appreciably impaired by
chronic therapy, but postural hypotension and fainting may occur in the
beginning—called ‘first dose effect’, and with dose increments. This disappears
with continued therapy, but may persist in the elderly. For this reason, prazosin
is always started at low dose (0.5 mg) given at bedtime and gradually increased
with twice daily administration till an adequate response is produced (max.
dose 10 mg BD). Patients who develop marked first dose effect generally require
lower maintenance doses (2–6 mg/ day). An oral dose produces peak fall in BP after
4–5 hours and the effect lasts for nearly 12 hours, though plasma t½ is only 3
hours. This may be due to generation of active metabolites.
Other advantages of
prazosin are:
·
Improves carbohydrate metabolism; suitable for
diabetics, but not if neuropathy is present —postural hypotension is
accentuated.
·
Has favourable effect on lipid profile: lowers
LDL cholesterol and triglycerides, increases HDL.
·
Affords symptomatic improvement in coexis ting
PVD or benign prostatic hypertrophy.
MINIPRESS XL: Prazosin
GITS 2.5 mg, 5 mg tabs.; PRAZOPRESS 1, 2 mg tabs.
Adverse Effects
Prazosin is generally
well tolerated at low doses. Apart from postural hypotension related symptoms
(to which tolerance frequently develops), other side effects are headache,
drowsiness, dry mouth, weakness, palpitation, nasal blockade, blurred vision and
rash. Ejaculation may be impaired in males: especially with higher doses. Fluid
retention attending prazosin monotherapy may precipitate CHF.
Prazosin is a
moderately potent antihypertensive with many desirable features, but is not
used as a first line drug because fluid retention and tolerance gradually
develops with monotherapy—necessitating dose increase—more side effects and
risk of CHF. It may be added to a diuretic + β blocker in those not
achieving target BP.
Terazosin, Doxazosin
These are long-acting congeners of prazosin with similar properties
and suitable for once daily dosing (see
p. 134). In the ALL HAT (2002) study doxazosin monotherapy has doubled the
incidence of CHF; but this can occur with any α1 blocker. A higher
incidence of stroke relative to patients receiving a thiazide diuretic was also
noted.
Nonselective α Blockers
(Phentolamine, Phenoxybenzamine)
The conventional α blockers have been
disappointing for routine treatment of hypertension, because fall in t.p.r. is
compensated by increased HR and c.o. They block both α1 and α2 receptors—NA release
is accentuated. They are reserved for special situations like pheochromocytoma,
clonidine withdrawal, cheese reaction, etc., where circulating CAs are
responsible for the rise in BP.
CENTRAL SYMPATHOLYTICS
Clonidine
It is an imidazoline
derivative having complex
actions. Clonidine is a partial agonist with high affinity and high intrinsic
activity at α2 receptors, especially
α2A subtype in brainstem.
The major haemodynamic effects result from stimulation of α2A receptors present
mainly post-junctionally in medulla (vasomotor centre) decrease sympathetic out
flow → fall in BP and
bradycardia (also due to enhanced vagal tone). Plasma NA declines. Though
clonidine is capable of reducing NA release from peripheral adrenergic nerve
endings (release inhibitory prejunctional α2 action), this is not
manifest at clinically used doses. Clonidine is a moderately potent antihypertensive.
Presence of Imidazoline receptors which are
distinct from α2 receptors has now been
confirmed both in the brain as well as periphery. These are activated by
clonidine and related drugs but not by NA. Experimental evidence suggests that
clonidine may first stimulate central imidazoline receptors which then trigger
medullary α2A receptors to reduce
sympathetic outflow. Clonidine also appears to directly stimulate α2A receptors to produce
hypotension and sedation. Rilmenidine
and moxonidine are selective cerebral
imidazoline receptor agonists with low α2 receptor affinity.
Therefore, they have low sedative property but equivalent antihypertensive
action.
Rapid i.v. injection
of clonidine raises BP transiently due to activation of peripheral postsynaptic
vasoconstrictor α2B receptors at the high
concentrations so attained. Oral doses producing lower plasma clonidine levels
cause only fall in BP, because clonidine has lower intrinsic activity on α2B receptors which
predominate in vascular smooth muscle. Probably for the same reason clonidine
exhibits the therapeutic window phenomenon: optimum lowering of BP occurs
between blood levels of 0.2–2.0 ng/ml. At higher concentrations fall in BP is
less marked.
On chronic administration of clonidine decrease in c.o.
contributes more to the fall in BP than decrease in t.p.r. Cardiovascular
reflexes are affected little. Decreased sympathetic flow to the kidney results
in reduced renin release. It does not alter plasma lipid levels.
Pharmacokinetics
Clonidine is well
absorbed orally; peak occurs in 2–4 hours;
1/2 to 2/3 of an oral dose is excreted unchanged in urine, the rest as metabolites.
Plasma t½ is 8–12 hours. Effect of a single dose lasts for 6–24 hours.
Dose: Start with 100 μg OD or BD, max. 300 μg TDS, orally or i.m.
CATAPRES 150 μg tab, ARKAMIN 100 μg tab.
Adverse Effects
Side effects with
clonidine are relatively common.
· Sedation, mental depression, disturbed sleep;
dryness of mouth, nose and eyes (secretion is decreased by central action), constipation
(antisecretory effect on the intestines).
·
Impotence, salt and water retention,
bradycardia (due to reduced sympathetic tone).
·
Postural hypotension occurs, but is mostly
asymptomatic.
· Alarming rise in BP, in excess of pretreatment
level, with tachycardia, restlessness, anxiety, sweating, headache, nausea and
vomiting occur in some patients when doses of clonidine are missed for 1–2
days. The syndrome is very similar to that seen in pheochromocytoma: plasma
catecholamine (CA) concentration is increased. This is due to:
a)
Sudden removal of central sympathetic
inhibition resulting in release of large quantities of stored CAs.
b)
Supersensitivity of peripheral adrenergic
structures to CAs that develops due to chronic reduction of sympathetic tone
during clonidine therapy.
A combination of α blocker with a β blocker, or a potent
vasodilator or clonidine itself can be used to treat the syndrome.
Interactions
Tricyclic
antidepressants and chlorpromazine abolish the
antihypertensive action of clonidine, probably by blocking α receptors on which
clonidine acts.
Use
Clonidine was a
popular antihypertensive in the late 1960s and
1970s, but frequent side effects, risk of withdrawal hypertension and
development of tolerance to its monotherapy have relegated it to a 3rd or 4th
choice drug. At present, it is occasionally used in combination with a
diuretic.
Other indications
1. Opioid withdrawal: Opioid and α2 adrenergic systems
converge on the same effectors in many systems; both activate the Gi regulatory
protein. Clonidine suppresses sympathetic overactivity of opioid withdrawal
syndrome and reduces craving to some extent.
Clonidine has also
facilitated alcohol withdrawal and smoking cessation.
2. Clonidine has
analgesic activity. It has been used to substitute morphine for
intrathecal/epidural surgical and postoperative analgesia.
3. Administered
preoperatively, it diminishes anaesthetic requirement.
4. Clonidine
attenuates vasomotor symptoms of menopausal syndrome.
5. Clonidine has been
used to control loose motions due to diabetic neuropathy—may be acting by α2 receptor mediated
enhancement of salt absorption in gut mucosa.
6. Clonidine suppression test for pheochromocytoma: clonidine
reduces plasma NA concentration to < 0.5 ng/ ml in patients of essential
hypertension but not in those with pheochromocytoma.
Methyldopa
It is the α-methyl analogue of dopa, the precursor of dopamine (DA) and NA. The α methyl-NA (a
selective α2 agonist) formed in
the brain from methyldopa acts on central α2 receptors to decrease
efferent sympathetic activity. Because methyldopa decreases t.p.r. more than HR
or c.o., it may be acting on a different population of neurones in the
vasomotor centre than clonidine. In large doses, methyldopa inhibits the enzyme
dopa decarboxylase in brain and periphery → reduces NA synthesis
and forms the false transmitter methyl-NA in periphery as
well. These mechanisms were
considered to be responsible for the antihypertensive effect; but it was demonstrated
that neither responses to stimulation of sympathetic nerves nor their NA
content was reduced at clinically used antihypertensive doses. Moreover, α methyl NA is as
potent vasoconstrictor as NA. The primary central site of action of methyldopa
has been confirmed.
Methyldopa is a moderate efficacy antihypertensive. Circulating
levels of NA and renin tend to fall due to reduction in sympathetic tone. Inhibition
of postural reflexes is mild.
Pharmacokinetics
Though methyldopa is
transported actively by intestinal
amino acid carrier, less than 1/3 of an oral dose is absorbed. It is partly
metabolized and partly excreted unchanged in urine. Antihypertensive effect
develops over 4–6 hours and lasts for 12–24 hours.
Dose: 0.25–0.5 g BD–QID
oral.
EMDOPA, ALPHADOPA 250
mg tab.
Adverse Effects
Sedation, lethargy and
reduced mental capacity are common
side effects.
Cognitive impairment may develop. Dryness of mouth, nasal
stuffiness, headache, fluid retention, weight gain, impotence.
Postural hypotension is generally mild but more common than with
clonidine; occurs especially in the elderly patients and in those receiving a
diuretic.
Positive Coomb’s test
occurs in 1/6 patients, few develop haemolytic anaemia. Fever, rash, hepatitis,
‘flu’ like illness, thrombocytopenia and rarely lupus syndrome occur.
Rebound hypertension
on sudden withdrawal of methyldopa is mild and less common.
Interactions
Tricyclic antidepressants
reverse its action by blocking its active
transport into the adrenergic neurones.
Use
Methyldopa was a
widely used antihypertensive, especially in combination with a diuretic.
However, it is infrequently used now, except to treat hypertension during
pregnancy wherein it has a long track record of safety, both for the mother as
well as the foetus.
VASODILATORS
Hydralazine/Dihydralazine
It is a directly acting arteriolar vasodilator with little
action on venous capacitance vessels; reduces t.p.r. It causes greater
reduction of diastolic than systolic BP. Reflex compensatory mechanisms are
evoked which cause tachycardia, increase in c.o. and renin release → increased aldosterone
→ Na+ and water
retention. The disproportionate cardiac stimulation appears to involve direct
augmentation of NA release and myocardial contractility as well. Thus, a
hyperdynamic circulatory state is induced—angina may be precipitated due to
increased cardiac work as well as steal phenomenon. There is no reduction in renal
blood flow despite fall in BP. However, fluid retention and edema may occur by
the above mechanism. Tolerance to the hypotensive action develops unless
diuretics or β blockers or both are
given together to block the compensatory mechanisms.
The mechanism of
vascular smooth muscle relaxant action of hydralazine is not clearly known. It
is partly endothelium dependent: may involve generation of NO (nitric oxide) and
stimulation of cGMP. Direct effects on membrane potential and on Ca2+ fluxes
have also been proposed.
Pharmacokinetics
Hydralazine is well absorbed orally, and is subjected to
first pass metabolism in liver. The chief metabolic pathway is acetylation which
exhibits a bimodal distribution in the population: there are slow and fast
acetylators. Bioavailability is higher in slow acetylators, but these patients
are more prone to develop the lupus syndrome.
Hydralazine is completely metabolized both in liver and plasma;
the metabolites are excreted in urine, t½ 1–2 hours. However, hypotensive
effect lasts longer (12 hours), probably because of its persistence in the
vessel wall.
Dose: 25–50 mg OD–TDS; NEPRESOL 25 mg tab.
Adverse Effects are frequent and mainly
due to vasodilatation.
1. Facial flushing, conjunctival injection, throbbing headache,
dizziness, palpitation, nasal stuffiness, fluid retention, edema, CHF.
2. Angina and MI may be precipitated in patients with coronary
artery disease.
3. Postural hypotension is not prominent because of little
action on veins: venous return and c.o. are not reduced.
4. Paresthesias, tremor, muscle cramps, rarely peripheral
neuritis.
5. Lupus erythematosus or rheumatoid arthritis like symptoms
develop on prolonged use of doses above 100 mg/day. It is more common in women
and in slow acetylators. It is slowly reversible on stopping treatment.
Use
Hydralazine is used in moderate-to-severe hypertension not controlled by the first line
drugs. Usually, low doses are added to the diuretic and blocker already being
administered. It is not used alone. Large doses are not recommended for long
periods.
Hydralazine can be used in patients with renal involvement, but
is contraindicated in older patients and in those with ischaemic heart disease.
It is one of the preferred antihypertensives during pregnancy because of
decades of experience and record of safety. It can also be used parenterally in
hypertensive emergencies.
The arteriolar dilator
action of hydralazine can be employed in the management of CHF (see p. 504–505).
Minoxidil
It is a powerful
vasodilator, the pattern of action resembling
hydralazine, i.e. direct relaxation of arteriolar smooth muscle with little
effect on venous capacitance. Marked vasodilatation elicits strong compensatory
reflexes: increased renin release and proximal tubular Na+ reabsorption → marked Na+ and water
retention → edema and CHF may
occur; increased sympathetic activity → palpitation, increased c.o. To offset these,
it has to be used along with a loop diuretic and a blocker.
Minoxidil is a
prodrug—converted to an active metabolite (by sulfate conjugation) which is an
opener of ATP operated K+ channels; acts by hyperpolarizing smooth muscle.
Minoxidil is indicated
only rarely in severe or life-threatening hypertension.
Use in alopecia Oral minoxidil
increases growth of body hair. Applied
topically (2% twice daily) it promotes hair growth in male pattern baldness and alopecia
areata. The response is slow (takes 2– 6 months) and incomplete, but upto
60% subjects derive some benefit, albeit for short periods. Baldness recurs
when therapy is discontinued. The mechanism of increased hair growth is not
known; may involve:
·
Enhanced microcirculation around hair
follicles.
·
Direct stimulation of resting hair follicles.
·
Alteration of androgen effect on genetically
programmed hair follicles.
Local irritation,
itching and burning sensation are frequent. Dermatological reaction and systemic
side effects (headache, dizziness, palpitation)occur in 1–3% cases.
MINTOP, GROMANE 2%
scalp lotion, MULTIGAIN 2% topical solution and metered spray, MANEXIL 5% gel;
apply twice a day.
Diazoxide
This K+ channel opener dilator of arterioles was used in the past for rapid reduction of BP
in hypertensive emergencies. It is administered by rapid i.v. injection in
fractional doses (50–100 mg) repeated every 5–10 min, as required. Slow i.v.
injection or infusion is less effective because it binds tightly to plasma
proteins before binding to vessel wall.
The duration of action
is long (6–24 hours) because of tight binding to plasma and tissue proteins. It
is employed in place of nitroprusside when regulated i.v. infusion or close
monitoring is not possible.
Sodium nitroprusside
It is a rapidly (within seconds) and
consistently acting vasodilator; has brief duration of action (2–5
min)—vascular tone can be titrated with the rate of i.v. infusion. It relaxes
both resistance and capacitance vessels: reduces t.p.r. as well as c.o. (by
decreasing venous return). Myocardial work is reduced—ischaemia is not
accentuated, as occurs with selective arteriolar dilators (hydralazine). Little
reflex tachy cardia is produced in supine posture. Plasma renin is increased.
In patients with heart failure and ventricular dilatation,
nitroprusside improves ventricular function and CO by reducing cardiac preload
and afterload.
Endothelial cells, RBCs (and may be other cells) split
nitroprusside to generate NO which relaxes vascular smooth muscle. The enzymes
involved are different from those that produce NO from glyceryl trinitrate.
Moreover, nitroprusside is nonenzymatically converted to NO (and CN) by
glutathione. This may be responsible for the different pattern of vasodilator
action compared to nitrates, as well as for the fact that no nitrate like
tolerance develops to nitroprusside action.
Nitroprusside has gained popularity in the management of
hypertensive emergencies; 50 mg is added to a 500 ml bottle of saline/glucose
solution. The infusion is started at 0.02 mg/min and titrated upward with the
response: 0.1–0.3 mg/min is often needed. It decomposes at alkaline pH and on
exposure to light: the infusion bottle should be covered with black paper.
Nitroprusside is split to release cyanide. The latter is
converted in liver to thiocyanate which is excreted slowly. If larger doses are
infused for more than 1–2 days, excess thiocyanate may accumulate and produce
toxicity, including psychosis.
Side effects mainly due to vasodilatation are— palpitation,
nervousness, vomiting, perspiration, pain in abdomen, weakness, disorientation,
and lactic acidosis (caused by the released cyanide).
Nitroprusside has also been used to produce controlled
hypotension, in refractory CHF, pump failure accompanying MI and in acute
mitral regurgitation.
SONIDE, PRUSIDE,
NIPRESS 50 mg in 5 ml inj.
ADRENERGIC NEURONE BLOCKERS
Reserpine
It is an alkaloid from
the roots of Rauwolfia serpentina (sarpgandha)
indigenous to India which has been used in ‘Ayurvedic’ medicine for centuries.
The pure alkaloid was isolated in 1955 and later found to act by causing CA and
5HT depletion. It was a popular antihypertensive of the late 1950s and early
1960s, but is now used only as a pharmacological tool.
Reserpine acts at the
membrane of intraneuronal granules which store monoamines (NA, 5HT, DA) and
irreversibly inhibits the active amine transporters → the monoamines are gradually
depleted and degraded by MAO. The effects last long after the drug is
eliminated (hit and run drug) because tissue CA stores are restored only
gradually.
Higher doses deplete
CAs and 5HT in the brain as well; cause sedation and mental depression.
Antipsychotic effect (mild) and extrapyramidal symptoms are produced due to DA
depletion.
SERPASIL 0.25 mg tab;
1 mg/ml inj.
Guanethidine
It is a polar
guanidine compound which is taken up into the
adrenergic nerve endings by active amine transport, and has three important
facets of action:
·
Displaces NA from storage granules
stoichiometrically.
·
Inhibits nerve impulse coupled release of NA.
·
Engages and blocks NA uptake mechanism at the
axonal membrane.
Guanethidine has gone out
of use now due to marked side effects.
Treatment Of Hypertension
The aim of
antihypertensive therapy is to prevent morbidity and mortality associated with
persistently raised BP by lowering it to an acceptable level, with minimum
inconvenience to the patient. Both systolic and diastolic BP predict the likelihood
of target organ damage and complications such as:
1.
Cerebrovascular disease, transient ischaemic
attacks, stroke, encephalopathy.
2.
Hypertensive heart disease—left ventricular
hypertrophy, CHF.
3.
Coronary artery disease (CAD), angina, myocardial
infarction, sudden cardiac death.
4.
Arteriosclerotic peripheral vascular disease,
retinopathy.
5.
Dissecting aneurysm.
6.
Glomerulopathy, renal failure.
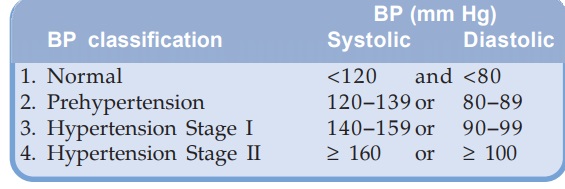
The JNC 7 (2003) has
reclassified BP readings as:
Since the risk of
complications depends not only on the level of BP, but also on other risk
factors (see box) and existing target
organ damage (TOD), these have also to be considered in deciding when to start
drug therapy, in selection of drugs and in devising therapeutic regimens.
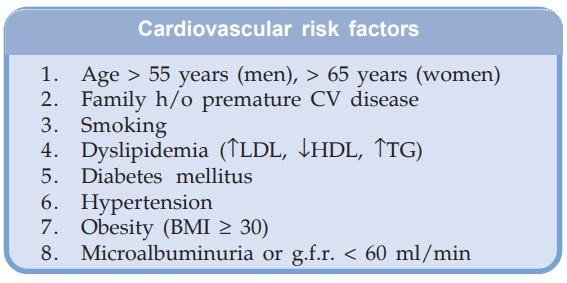
Cardiovascular risk factors
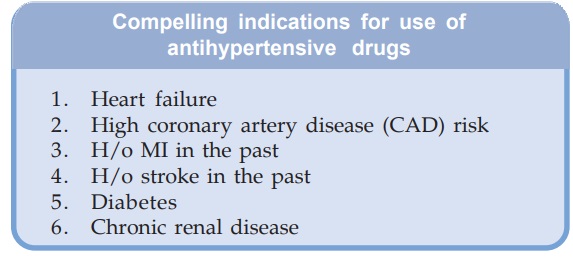
The JNC7 have also
identified compelling indications (see
box) which may mandate use of specific antihypertensive drugs even in patients
with BP values in the ‘prehypertension’ range. Moreover, presence of compelling
indications may suggest fixing a lower target BP value to be attained by drug
therapy.
Beneficial effects of
lowering BP has been established in all patients having BP above 140/ 90 mm Hg,
and even in the 120–139 (systolic) or 80–89 mm Hg (diastolic) range in those
with compelling indications or cardiovascular risk factors; e.g. in diabetics,
lowering diastolic BP to 80 mmHg was found to reduce cardiovascular events more
than reducing it upto 90 mm Hg.
If the cause of
hypertension can be identified (hormonal, vascular abnormality, tumours, renal
disease, drugs) all efforts should be made to remove it. Nonpharmacological
measures (life style modification—diet, Na+ restriction, aerobic activity or
exercise, weight reduction, moderation in alcohol intake, mental relaxation,
etc.) should be tried first and concurrently with drugs. The level to which BP
should be lowered is uncertain. A value of < 140 systolic and < 90 mmHg
diastolic is considered adequate response, because it clearly reduces morbidity
and mortality, though risk reduction may continue upto 120/80 mmHg in terms of
CAD, heart failure, stroke, etc. When significant cardiovascular and/or renal
damage has already occurred, lowering BP to normotensive level may not be
tolerated: edema, CHF, angina, rise in blood urea and syncope may be
precipitated: reduce BP gradually and only to the level tolerated.
The Swedish trial in
old patients with hypertension2 (STOP2, 1999) conducted over 5 years in 6614
hypertensives aged 70–84 years has shown that conventional therapy with
diuretic and/or β blockers is as effective in reducing BP and risk of major
cardiovascular events as are ACE inhibitors or CCBs. The ALLHAT (2002) study
comparing chlorthalidone, lisinopril and amlodipine has also found no
difference in the primary outcomes of death and MI. The results convey that
efficacywise there is little to choose among the 4 classes of drugs; choice of
initial drug has to be guided by associated features/contraindications and
acceptable side effects in individual patients.
With the establishment
of at least five groups (ACE inhibitors; AT1 antagonists, CCBs, β blockers, diuretics)
of first choice drugs and their evaluation in large multicentric trials, an
‘individualized care approach’ can be adopted for the selection of initial
monotherapy, followed if needed, by stepped combination therapy. The principle
of this approach is to match the lifestyle issues, tolerability and concomitant
medical conditions of individual patients with the pharmacological and clinical
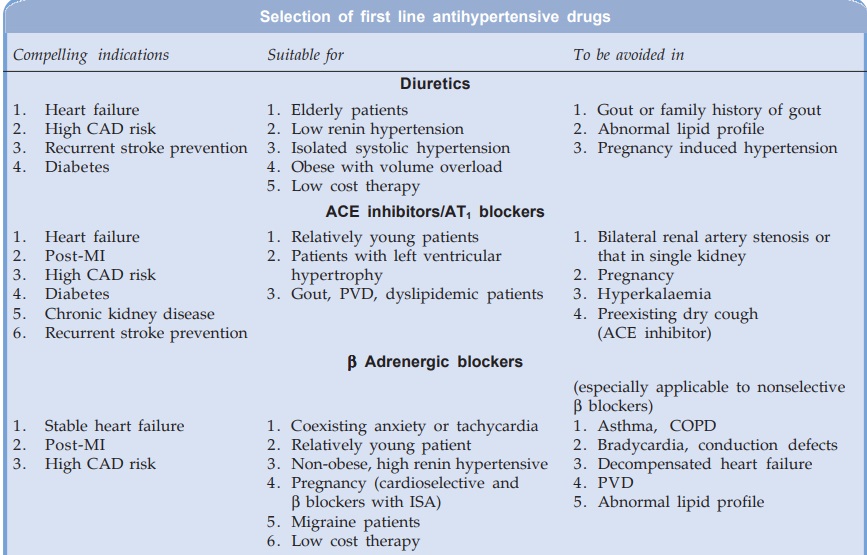
properties of an appropriate antihypertensive drug. For each class of
antihypertensive drugs, certain patients can be identified who are best suited
to be treated with that drug as first choice therapy, and those in whom it
should be avoided (see box).
The general principles of antihypertensive therapy enunciated in
JNC7 and WHOISH guidelines may be summarized as:
1. Except for stage II hypertension, start with a
single most appropriate drug which for majority of patients is a thiazide.
However, a β
blocker,
ACE inhibitor, ARB or CCB may also be considered. The CCBs may be less suitable
for monotherapy due to less convincing prognostic benefits, except in the
elderly and for stroke prevention.
2.
Initiate therapy at low dose; if needed
increase dose moderately. Thiazide dose should be 12.5–25 mg/day hydrochlorothiazide
or equivalent.
3. Majority of stage II hypertensives are started
on a 2 drug combination; one of which usually is a thiazide diuretic.
4.
If only partial response, add a drug from
another complimentary class or change to low dose combination.
5.
If no response, change to a drug from another
class, or low dose combination from other classes.
6.
In case of side effect to the initially chosen
drug, either substitute with drug of another class or reduce dose and add a
drug from another class.
With the above approach 50–70% stage I hypertensives can be
successfully treated, at least initially, with mono-drug therapy. A simple
regimen with once or twice daily drug dosing is most likely to be complied
with. Because most stage I and some stage II hypertension patients are asymptomatic,
a drug which makes them symptomatic (one or the other side effect) is not
likely to be accepted for prolonged periods. Effect of the drug on quality of
life measured by sense of wellbeing, energy level, mental acuity, drive,
libido, sleep, life satisfaction, etc. is an important criterion in drug
selection.
Combination Therapy
Though both JNC 7 and WHOISH emphasise on single drug therapy, the
addition of a second (and third) drug when monotherapy fails or is not tolerated,
is also highlighted. In practice, a large majority of hypertensives ultimately
require 2 or more drugs. In the HOT study 70% patients who achieved target BP
were being treated with 2 drugs.
Since BP is kept up by several interrelated factors, an attempt
to block one of them tends to increase compensatory activity of the others. It
is rational in such cases to combine drugs with different mechanisms of action
or different patterns of haemodynamic effects:
· Drugs which increase plasma renin activity—
diuretics, vasodilators, CCBs, ACE inhibitors may be combined with drugs which
lower plasma renin activity—β blockers, clonidine, methyldopa.
·
All sympathetic inhibitors (except β blockers) and
vasodilators cause fluid retention: used alone tolerance develops. Addition of
a diuretic checks fluid retention and development of tolerance.
·
Hydralazine and DHPs cause tachycardia which
is counteracted by β blockers, while the initial increase in t.p.r. caused by nonselective
β blockers is
counteracted by the vasodilator.
· ACE inhibitors/ARBs are particularly synergistic
with diuretics; this combination is very good for patients with associated CHF
and left ventricular hypertrophy.
· Other useful combinations are: ACE
inhibitor/ARB + CCB ACE inhibitor/ARB + β blocker β blocker + prazosin
Combination therapy
with low doses of each component allows BP reduction in nonresponsive patients
with fewer side effects: antihypertensive action of the components adds up,
while side effects being different do not. Use of combined formulation improves
compliance and lowers cost.
A three drug
combination therapy may be needed in a few patients (of severe or nonresponsive
hypertension). Commonly used triple drug combinations are:
CCB + ACE inhibitor/ARB + diuretic
CCB + β blocker + diuretic
ACE inhibitor/ARB + β blocker + diuretic
Combinations including
prazosin or clonidine or hydralazine are infrequently used. Patients who fail
to reach the goal BP despite being adherent to full doses of an appropriate 3
drug (including a diuretic) regimen, have been labelled by JNC7 as ‘resistant
hypertension’. In them even 4 drug therapy may have to be given to achieve the
target BP. However, the patient must be reevaluated and factors like noncompliance,
pseudo-tolerance, need for a loop diuretic, drug interactions, secondary
hypertension, etc. must be first excluded.
Combinations To Be Avoided
·
An α or β adrenergic blocker with clonidine: apparent
antagonism of clonidine action has been observed.
·
Nifedipine (or other DHPs) with diuretic:
synergism between these drugs is unproven.
·
Hydralazine with a DHP or prazosin: similar
pattern of haemodynamic action.
· Verapamil or diltiazem with β blocker: marked bradycardia, AV block.
·
Methyldopa with clonidine or any two drugs of
the same class.
Some Antihypertensive Combinations
1. Amlodipine 5 mg +
Lisinopril 5 mg—AMLOPRESL, LISTRILAM
2. Amlodipine 5 mg + Atenolol
50 mg—AMCARDAT, AMLOPINAT, AMLOPRESAT
3. Amlodipine 5 mg + Enalapril
5 mg—AMACE,
AMTASE
4. Atenolol 25 mg or
50 mg + chlorthalidone 12.5 mg—TENOCLOR,
TENORIC
5. Enalapril 10
mg + Hydrochlorothiazide 25 mg—
ENACED,
VASONORMH
6. Ramipril 2.5 mg +
Hydrochlorothiazide 12.5 mg— CARDACEH
7. Losartan 50 mg + Hydrochlorothiazide 12.5 mg— LOSARH, TOZAARH,
LOSACARH
8. Lisinopril 5 mg +
Hydrochlorothiazide 12.5 mg— LISTRIL PULS, LISORILHT
9. Losartan 50
mg + Ramipril
2.5 mg or
5 mg— TOZAARR, LAPIDOR
10. Losartan 50 mg + Amlodipine
5 mg—AMCARDLP, AMLOPRESSZ,
LOSACARA
11. Losartan 50 mg + Ramipril 2.5 mg + Hydrochlorothiazide 12.5
mg—LOSANORMHR
12. Irbesartan 150 mg + Hydrochlorothiazide 12.5 mg— IROVELH, XARBH.
When the BP has been well controlled for > 1 year, stepwise reduction
in dose and/or withdrawal of one or more components of a combination may be
attempted to workout a minimal regimen that will maintain the target BP.
However, in most patients of essential hypertension, drug therapy is usually
lifelong.
Related Topics
