Antiemetics
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs For Emesis, Reflux And Digestive Disorders
These are drugs used to prevent or suppress vomiting.
ANTIEMETICS
These are drugs used
to prevent or suppress vomiting.
Classification
1. Anticholinergics
Hyoscine, Dicyclomine
2. H1 Antihistaminics
Promethazine, Diphenhydramine,
Dimenhydrinate, Doxylamine, Cyclizine, Meclozine, Cinnarizine.
3. Neuroleptics (D2 blockers)
Chlorpromazine, Prochlorperazine,
Haloperidol, etc.
4. Prokinetic drugs
Metoclopramide, Domperidone,
Cisapride, Mosapride Tegaserod
5. 5-HT3 antagonists
Ondansetron, Granisetron
6. Adjuvant
Dexamethasone, antiemetics
Benzodiazepines, Cannabinoids.
ANTICHOLINERGICS
Hyoscine (0.2–0.4 mg oral, i.m.) is the most effective drug for motion sickness. However,
it has a brief duration of action; produces sedation and other anticholinergic side
effects; suitable only for short brisk journies. It acts probably by blocking
conduction of nerve impulses across a cholinergic link in the pathway leading
from the vestibular apparatus to the vomiting centre and is not effective in vomiting
of other etiologies.
A transdermal patch
containing 1.5 mg of hyoscine, to be delivered over 3 days has been developed.
Applied behind the pinna, it suppresses motion sickness while producing only
mild side effects.
Dicyclomine (10–20 mg oral) has been used for prophylaxis of motion sickness and for
morning sickness. It has been cleared of teratogenic potential.
H1 ANTIHISTAMINICS
Some anti-histaminics
are antiemetic. They are useful mainly in motion sickness and to a lesser extent
in morning sickness, postoperative and some other forms of vomiting. Their
antiemetic effect appears to be based on anticholinergic, antihistaminic and
sedative properties.
Promethazine, Diphenhydramine, Dimenhydrinate These drugs afford
protection of motion sickness for 4–6
hours, but produce sedation and dryness of mouth. By their central
anticholinergic action they block the extrapyramidal side effects of
metoclopramide while supplementing its antiemetic action. Their combination is
used in chemotherapy induced vomiting.
Promethazine Theoclate (AVOMINE
25 mg tab.) It has been specially promoted
as an antiemetic, but the action does not appear to be significantly different
from promethazine HCl.
Doxylamine It is a sedative H1 antihistaminic with prominent
anticholinergic activity. Marketed in combination with pyridoxine, it is
specifically promoted in India for ‘morning sickness’ (vomiting of early
pregnancy) although such use is not made in the USA, UK and many other
countries.
After over 2 decades
of worldwide use of a combination product of doxylamine for morning sickness,
some reports of foetal malformation appeared and the product was withdrawn in
1981. Subsequent studies have both supported and refuted its teratogenic potential.
Though the USFDA and CSM in UK found no credible evidence of increase in birth
defects, they did not rule out the possibility. The product remains suspended
in these countries, probably to avoid litigation, but not due to safety or
efficacy concerns. In USA and UK doxylamine is available for treatment of allergic
reaction, cough and cold.
Oral absorption of doxylamine is slow, and its t½ is 10 hr. The
side effects are drowsiness, dry mouth, vertigo and abdominal upset.
Dose: 10– 20 mg at bed time;
if needed additional doses may be
given in morning and afternoon.
DOXINATE, GRAVIDOX, VOMNEX, NOSIC: 10 mg with pyridoxine 10 mg
tab.
Cyclizine, Meclizine These are less
sedative and less anticholinergic.
Meclizine is long-acting, protects against sea sickness for nearly 24 hours.
MAREZINE: Cyclizine 50
mg tab; DILIGAN: Meclizine 12.5 mg + nicotinic acid 50 mg tab; PREGNIDOXIN: Meclizine
25 mg + Caffeine 20 mg tab.
Cinnarizine It is an antivertigo drug, and is also protective for motion sickness. It probably
acts by inhibiting influx of Ca2+ from endolymph into the vestibular sensory
cells which mediates labyrinthine reflexes.
Anticholinergic-antihistaminic
antiemetics are the first choice drugs for motion
sickness. Antidopaminergic and antiHT3 drugs are less effective.
All antimotion sickness drugs act better when taken ½–1 hour before commencing
journey. Once sickness has started, it is more difficult to control; higher
doses/parenteral administration may be needed.
The antihistaminics
are suspected to have teratogenic potential, but there is no conclusive proof.
Nevertheless, it is better to avoid them for morning sickness. Most cases of
morning sickness can be managed by reassurance and dietary adjustment. If an
antiemetic has to be used, dicyclomine, promethazine, prochlorperazine or metoclopramide
may be prescribed in low doses.
NEUROLEPTICS
These are potent
antiemetics; act by blocking D2 receptors in the CTZ; antagonize apomorphine
induced vomiting and have additional antimuscarinic as well as H1
antihistaminic property. They have broad spectrum antiemetic action effective
in:
·
Drug induced and post-anaesthetic nausea and
vomiting.
·
Disease induced vomiting: gastroenteritis,
uraemia, liver disease, migraine, etc.
· Malignancy associated and cancer chemotherapy
(mildly emetogenic) induced vomiting.
·
Radiation sickness vomiting (less effective).
·
Morning sickness: should not be used except in
hyperemesis gravidarum.
They are less
effective in motion sickness: the vestibular pathway does not involve dopaminergic
link.
Most of these drugs
produce significant degree of sedation. Acute muscle dystonia may occur after a
single dose, especially in children and girls. The antiemetic dose is generally
much lower than antipsychotic doses. These agents should not be administered
until the cause of vomiting has been diagnosed; otherwise specific treatment of
conditions like intestinal obstruction, appendicitis may be delayed due to
symptom relief.
Prochlorperazine This D2 blocking
phenothiazine is a labyrinthine suppressant, has selective antivertigo and
antiemetic actions. It is highly effective when given by injection in vertigo
associated with vomiting and to some extent in cancer chemotherapy associated
vomiting. Prochlorperazine is used as an antiemetic rather than as
antipsychotic. Muscle dystonia and other extrapyramidal side effects are the
most important limiting features.
STEMETIL 5, 25 mg
tabs., 12.5 mg/ml inj, 1 ml amp, 10 ml vial.
PROKINETIC DRUGS
These are drugs which
promote gastrointestinal transit and speed gastric emptying by enhancing
coordinated propulsive motility.
Metoclopramide
Metoclopramide is
chemically related to procainamide, but has no pharmacological similarity with
it. Introduced in early 1970s as a ‘gastric hurrying’ agent, it is now a widely
used antiemetic.
Actions
GIT: It has more prominent effect on upper g.i.t.; increases gastric peristalsis while
relaxing the pylorus and the first part of duodenum → speeds gastric emptying,
especially if it was slow. This action is independent of vagal innervation, but
is more prominent when vagus is intact. Lower esophageal sphincter (LES) tone
is increased and gastroesophageal reflux is opposed. It also increases
intestinal peristalsis to some extent, but has no significant action on colonic
motility and gastric secretion.
CNS: Metoclopramide is an
effective antiemetic; acting on the CTZ,
blocks apomorphine induced vomiting. The gastro-kinetic action may contribute
to the antiemetic effect. However, it has no chlorpromazine (CPZ) like neuroleptic
action, though it does share the extrapyramidal and prolactin secretion
augmenting action of CPZ.
Mechanism Of Action: Metoclopramide acts through both dopaminergic and serotonergic
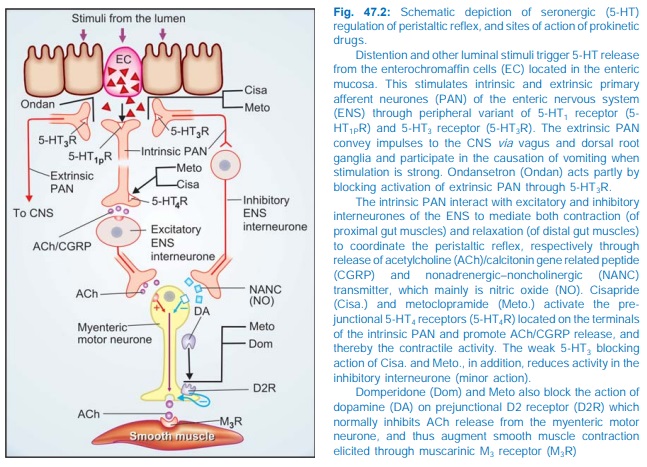
receptors (see Fig. 47.2)
D2 Antagonism
Dopamine (acting through D2 receptors) is an inhibitory
transmitter in the g.i.t.— normally acts to delay gastric emptying when food is
present in stomach. It also appears to cause gastric dilatation and LES
relaxation attending nausea and vomiting. Metoclopramide blocks D2 receptors
and has an opposite effect— hastening gastric emptying and enhancing LES tone
by augmenting ACh release. However, clinically this action is secondary to that
exerted through 5HT4 receptors.
The central antidopaminergic (D2) action of metoclopramide on
CTZ is clearly responsible for its antiemetic property. Other manifestations of
D2 blockade are antagonism of apomorphine induced vomiting, CPZ like
extrapyramidal effects and hyper-prolactinaemia.
5HT4
Agonism
Metoclopramide acts in
the g.i.t. to enhance ACh
release from myenteric motor neurones. This results from 5HT4
receptor activation on primary afferent neurones (PAN) of the ENS via excitatory inter-neurones (Fig.
47.2). The gastric hurrying and LES tonic effects are mainly due to this
action which is synergised by bethanechol and attenuated by atropine.
5HT3
Antagonism
At high concentrations metoclopramide can block 5HT3
receptors present on inhibitory myenteric inter-neurones and in NTS/CTZ. The
peripheral action can augment ACh release in the gut, but appears to be minor.
The central anti 5HT3 action appears to be significant only when
large doses are used to control chemotherapy induced vomiting.
Pharmacokinetics
Metoclopramide is rapidly absorbed orally,
enters brain, crosses placenta and is secreted in milk. It is partly conjugated
in liver and excreted in urine within 24 hours; t½ is 3–6 hours. Orally it acts
in ½–1 hr, but within 10 min after i.m. and 2 min after i.v. injection. Action
lasts for 4–6 hours.
Interactions
It hastens the absorption of many drugs, e.g. aspirin,
diazepam, etc. by facilitating gastric emptying. It reduces the extent of
absorption of digoxin by allowing less time for it. Bioavailability of
cimetidine is also reduced.
By blocking DA receptors in basal ganglia, it abolishes the therapeutic
effect of levodopa.
Adverse Effects
Metoclopramide is
generally well tolerated.
Sedation, dizziness, loose stools, muscle dystonias (especially
in children) are the main side effects.
Long-term use can cause parkinsonism, galactorrhoea and gynaecomastia.
It should not be used
to augment lactation. Though the amount secreted in milk is small, but suckling
infant may develop loose motions, dystonia, myoclonus.
Dose: 10 mg (children
0.2–0.5 mg/kg) TDS oral or i.m. For
chemotherapy induced vomiting 0.3–1.0 mg/kg slow i.v./i.m. PERINORM, MAXERON,
REGLAN, SIGMET, 10 mg tab; 5 mg/5 ml syr; 10 mg/2 ml inj.; 50 mg/ 10 ml inj.
Uses
1.
Antiemetic: Metoclopramide is an
effective and popular drug for many
types of vomiting— postoperative, drug induced, disease associated (especially
migraine), radiation sickness, etc, but is less effective in motion sickness.
Though ondansetron is preferred, metoclopramide continues to be used for prophylaxis
and treatment of vomiting induced by highly emetic anticancer drugs (cisplatin,
etc.). A higher dose (1 mg/kg i.v.) is often needed, but is effective when
phenothiazines and antihistamines do not work. Promethazine, diphenhydramine,
diazepam or lorazepam injected i.v. along with metoclopramide supplement its
antiemetic action and reduce the attending dystonic reactions. Dexamethasone
i.v. also augments the efficacy of metoclopramide.
Though no teratogenic
effects have been reported, metoclopramide should be used for morning sickness
only when not controlled by other measures.
2.
Gastrokinetic: to accelerate gastric
emptying:
· When emergency general anaesthesia has to be
given and the patient has taken food less than 4 hours before.
·
To relieve post-vagotomy or diabetes
associated gastric stasis.
·
To facilitate duodenal intubation. Clinical
efficacy is moderate.
3.
Dyspepsia and other functional
g.i. disorders. Metoclopramide may succede in stopping persistent hiccups.
4. Gastroesophageal Reflux
Disease (GERD) Metoclopramide may
afford symptomatic relief in milder cases of GERD, but is much less effective than
PPIs/H2 blockers. It does not aid healing of esophagitis. It may be
used as adjuvant to acid suppressive therapy, but additional benefit is
uncertain.
Domperidone
It is a D2 antagonist, chemically related to haloperidol,
but pharmacologically related to metoclopramide. It has lower ceiling
antiemetic and prokinetic actions. Unlike metoclopramide, its prokinetic action
is not blocked by atropine and is based only on D2 receptor blockade in upper
g.i.t. Domperidone crosses blood-brain barrier poorly. Accordingly, extrapyramidal
side effects are rare, but hyper-prolactinaemia can occur. However, it does act
on CTZ which is not protected by blood-brain barrier. Antiemetic efficacy is
lower than metoclopramide. Administered with levodopa or bromocriptine, it
counteracts their dose limiting emetic action without affecting the therapeutic
effect in parkinsonism.
Domperidone is absorbed orally, but bioavailability is only ~15%
due to first pass metabolism. It is completely bio-transformed and metabolites
are excreted in urine. Plasma t½ is 7.5 hr.
Side Effects
Are much less than
with metoclopramide: dry mouth, loose stools, headache, rashes, galactorrhoea.
Cardiac arrhythmias have developed on rapid i.v. injection.
Dose: 10–40 mg (Children
0.3–0.6 mg/kg) TDS. Its indications
are similar to that of metoclopramide, but it is a less efficacious
gastrokinetic and not useful against high emetogenic chemotherapy.
DOMSTAL, DOMPERON, NORMETIC 10 mg tab, 1 mg/ml susp, MOTINORM 10
mg tab, 10 mg/ml drops.
Cisapride
It is a prokinetic
drug with little antiemetic property,
because it lacks D2 receptor antagonism. Effects of cisapride on gastric motility
resemble metoclopramide—gastric emptying is accelerated, LES tone is improved and
esophageal peristalsis is augmented. It restores and facilitates motility
throughout the g.i.t., including colon (metoclopramide/domperidone do not
accelerate colonic transit). Cisapride often produces loose stools. Its
prokinetic action is exerted mainly through 5HT4 agonism which promotes
ACh release from myenteric neurones, aided by weak 5HT3 antagonism
which suppresses inhibitory transmission in myenteric plexus. Enteric neuronal
activation via 5HT4
receptor also promotes cAMP-dependent Cl– secretion in the colon, increasing
water content of stools. Cisapride is devoid of action on CTZ and does not
produce extrapyramidal symptoms or hyper-prolactinaemia.
Oral bioavailability
of cisapride is ~33%. It is primarily inactivated by hepatic metabolism by CYP3A4
with a t½ of ~10 hr. Dose needs to be reduced in liver disease.
Cisapride is a
prokinetic drug without antidopaminergic side effects, but abdominal cramps and
diarrhoea can occur. Other side effects are dizziness and occasional rise in
serum transaminases.
Primary indication of
cisapride has been GERD. Some patients derive symptomatic relief, but this is
less complete compared to PPIs/H2 blockers. Healing of esophageal
lesions is infrequent. Other indications of cisapride are nonulcer dyspepsia, impaired
gastric emptying and chronic constipation, though usefulness in these
conditions also is limited.
Safety of cisapride
was challenged by reports of serious ventricular arrhythmias and death, mainly
among patients who took CYP3A4 inhibitors like azole antifungals, macrolide
antibiotics, antidepressants, HIV protease inhibitors, etc. concurrently. At
high concentrations, cisapride blocks delayed rectifying K+ channels in
heart—prolongs QTc interval and predisposes to torsades de pointes/ventricular fibrillation. It has been
withdrawn in USA and some other countries, but is available in India.
Dose: 10–20 mg TDS; SYSPRIDE, UNIPRIDE,
NUPRIDE 10 mg tab; MOTEN, PULSID 10 mg tab, 5 mg/5 ml susp.; CIZA also
20 mg tab
Mosapride
A newer congener of cisapride with similar gastrokinetic
and LES tonic action due to 5HT4 agonistic (major) and 5HT3
antagonistic (minor) action in the myenteric plexus, but has not caused QTc
prolongation or arrhythmias. Like cisapride, it has no clinically useful
antiemetic action and does not produce extrapyramidal/hyper-prolactinaemic side
effects due to absence of D2 blocking property. Indications and side effects
are similar to cisapride.
Dose: 5 mg (elderly 2.5 mg)
TDS.
MOZA, MOZASEF, NORMAGUT 2.5, mg, 5 mg tabs; MOZA MPS: 5 mg + methylpolysiloxane
125 mg tab.
Tegaserod
It is a recently
introduced selective 5HT4
partial agonist, with no action on 5HT3 and other receptors, which
mainly augments colonic motility along with promotion of gastric emptying and intestinal
transit, and less effect on LES tone. The 5HT4 agonistic action also
increases colonic Cl– (and water) secretion. The current indication of
tegaserod is constipation predominant irritable bowel syndrome (described in Ch.
No. 48). Its possible use as a gastro-kinetic is being explored.
5HT3 ANTAGONISTS
Ondansetron
It is the prototype of
a new class of antiemetic
drugs developed to control cancer chemotherapy/radiotherapy induced vomiting,
and later found to be highly effective in postoperative nausea and vomiting as
well. It blocks the depolarizing action of 5HT through 5HT3
receptors on vagal afferents in the g.i.t. as well as in NTS and CTZ. Cytotoxic
drugs/ radiation produce nausea and vomiting by causing cellular damage → release of mediators
including 5HT from intestinal mucosa → activation of vagal afferents in the gut → emetogenic impulses
to the NTS and CTZ. Ondansetron blocks emetogenic impulses both at their
peripheral origin and their central relay. It does not block dopamine receptors
and apomorphine or motion sickness induced vomiting. A weak gastrokinetic
action due to 5HT3 blockade has been detected, but it is clinically
insignificant. A minor 5HT4 antagonistic action has also been shown.
Pharmacokinetics:
Oral bioavailability
of ondansetron is 60–70% due to first pass metabolism. It is hydroxylated by
CYP 1A2, 2D6 and 3A, but no clinically significant drug interactions have been
noted. It is eliminated in urine and faeces, mostly as metabolites; t½ being
3–5 hrs, and duration of action 4–12 hr.
Dose and efficacy: For cisplatin and other highly emetogenic drugs—8 mg i.v. by slow injection
over 15 min ½ hr before chemotherapeutic infusion, followed by 2 similar doses
4 hour apart. To prevent delayed emesis 8 mg oral is given twice a day for 3–5
days. For postoperative nausea/vomiting 4–8 mg i.v. given before induction is
repeated 8 hourly. For less emetogenic drugs and for radiotherapy an oral dose
of 8 mg is given 1–2 hr prior to the procedure and repeated twice 8 hrly. It is
effective in 60–80% cases; similar to or better than high doses of metoclopramide,
and does not cause dystonias or sedation like the latter.
EMESET, VOMIZ,
OSETRON, EMSETRON 4,8 mg tabs, 2 mg/ml inj in 2 ml and 4 ml amps.
Patients who do not
obtain optimum protection by ondansetron alone, addition of dexamethasone,
promethazine/diazepam or both enhances antiemetic efficacy. Adjuvant drugs are
more often required for delayed phase vomiting that occurs on the second to
fourth day of cisplatin therapy, because 5HT3 antagonists alone are
less effective.
Other Types Of Vomiting: Efficacy of 5HT3 antagonists in prevention and treatment of
postoperative nausea and vomiting is now well established. Since this vomiting
is multifactorial in origin, 5HT3 blockers are not as completely
efficacious as in chemotherapy induced vomiting, and many other classes of antiemetic
drugs are also protective. In comparative trials, superiority of ondansetron in
terms of efficacy as well as lack of side effects and drug interactions has been
demonstrated. Administered before surgery ondansetron (4–8 mg i.v.) repeated
after 4 hours has become the first choice antiemetic at many centres.
Reports of efficacy in
vomiting associated with drug overdosage, side effect of cotrimoxazole and
fluvoxamine, uraemia and certain neurological injuries are also available.
Some 5HT3
antagonists have produced symptomatic relief in diarrhea-predominant irritable
bowel syndrome.
Side Effects:
Ondansetron is generally well tolerated: the only common side
effect is headache. Mild constipation or diarrhoea and abdominal discomfort
occur in few patients. Rashes and allergic reactions are reported, especially
after i.v. injection.
Granisetron
It is 10–15 times more potent than ondansetron and
probably more effective during the repeat cycle of chemotherapy. The weak 5HT4
blockade seen in ondansetron has not been detected in granisetron. Its plasma
t½ is longer (8–12 hrs) and it needs to be given only twice on the day of
chemotherapy. Side effect profile is similar to ondansetron.
Dose: 10 μg/kg i.v. 30 min
before chemotherapy, repeated after
12 hr. For less emetogenic regimen 2 mg oral 1 hr before chemotherapy or 1 mg
before and 1 mg 12 hr after it.
GRANICIP, GRANISET 1
mg, 2 mg tabs; 1 mg/ml inj. (1, 3 ml amps).
Dolasetron,
Tropisetron, and
Palonasetron are the other selective 5HT3 antagonists.
ADJUVANT ANTIEMETICS
Corticosteroids
(e.g. dexamethasone 8–20 mg i.v.) can alleviate nausea and
vomiting due to moderately emetogenic chemotherapy, but are more often employed
to augment the efficacy of other primary antiemetic drugs like metoclopramide
and ondansetron for highly emetogenic regimens and for cisplatin induced
delayed emesis. They also serve to reduce certain side effects of the primary
antiemetic. However, because of their metabolic effects, they should be used
only in selected and refractory cases.
Benzodiazepines
The weak antiemetic
property of BZDs is primarily
based on the sedative action. Used as adjuvant to metoclopramide/ondansetron,
diazepam/ lorazepam (oral/i.v.) help by relieving anxiety, anticipatory
vomiting and produce amnesia for the unpleasant procedure. They also suppress
dystonic side effects of metoclopramide.
Cannabinoids
9 Tetrahydrocannabinol ( 9 THC) is the active principle of the hallucinogen Cannabis indica. It possesses antiemetic
activity against moderately emetogenic chemotherapy. It probably acts at higher
centres or at vomiting centre itself by activating CB1 subtype of
cannabinoid receptors. The disorienting and other central effects of 9 THC limit
its clinical utility.
Dronabinol, a synthetic 9 THC, is less hallucinogenic and more
antiemetic than 9 THC. Dronabinol has been used for chemotherapy induced
vomiting in patients who cannot tolerate other antiemetics or are unresponsive
to them.
It has also been tried
as an appetite stimulant in cachectic/AIDS patients. Nabilone is another cannabinoid with antiemetic property.
