Anti-Retrovirus Drugs
| Home | | Pharmacology |Chapter: Essential pharmacology : Antiviral Drugs
These are drugs active against human immunodeficiency virus (HIV) which is a retrovirus. They are useful in prolonging and improving the quality of life and postponing complications of acquired immunodeficiency syndrome (AIDS) or AIDSrelated complex (ARC), but do not cure the infection.
ANTI-RETROVIRUS DRUGS
These are drugs active against human immunodeficiency virus
(HIV) which is a retrovirus. They are useful in prolonging and improving the
quality of life and postponing complications of acquired immunodeficiency
syndrome (AIDS) or AIDS-related complex (ARC), but do not cure the infection.
The clinical efficacy of anti-retrovirus drugs is monitored primarily by plasma
HIV-RNA assays and CD4 lymphocyte count carried out at regular intervals.
The first antiretrovirus (ARV) drug Zidovudine was developed in 1987. Over the past 20 years, 20 drugs
belonging to 3 classes have been introduced and a large number of others are
under development.
NUCLEOSIDE REVERSE TRANSCRIPTASE INHIBITORS (NRTIS)
Zidovudine It is a thymidine analogue (azidothymidine,
AZT), the prototype NRTI. After phosphorylation in the host cell—zidovudine
triphosphate selectively inhibits viral reverse transcriptase (RNAdependent DNA
polymerase) in preference to cellular DNA polymerase.
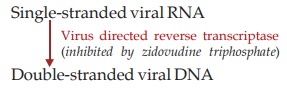
On the template of single-stranded
RNA genome of HIV a double-stranded DNA copy is produced by viral reverse
transcriptase. This DNA translocates to the nucleus and is integrated with
chromosomal DNA of the host cell, which then starts transcribing viral genomic
RNA as well as viral mRNA. Under the direction of viral mRNA, viral regulatory
and structural proteins are produced. Finally, viral particles are assembled and
matured. Zidovudine thus prevents infection of new cells by HIV, but has no
effect on virus directed DNA that has already integrated into the host
chromosome. It is effective only against retroviruses. Zidovudine itself gets
incorporated into the growing viral DNA and terminates chain elongation.
Resistance to AZT occurs by point mutations which alter reverse transcriptase
enzyme. In the past, when AZT was used alone, >50% patients became nonresponsive
to AZT within 1–2 years therapy due to growth of resistant mutants.
Pharmacokinetics The oral absorption of
AZT is rapid, but bioavailability
is ~65%. It is quickly cleared by hepatic glucuronidation (t½ 1 hr); 15–20% of
the unchanged drug along with the metabolite is excreted in urine. Plasma protein
binding is 30% and CSF level is ~50% of that in plasma. It crosses placenta and
is found in milk.
Dose Adults 300 mg BD;
Children 180 mg/m2 (max 200 mg) 6–8 hourly.
RETROVIR, ZIDOVIR 100 mg cap, 300 mg tab, 50 mg/5 ml syr VIROZ,
ZIDOMAX, ZYDOWIN 100 mg cap, 300 mg tab. (to be taken with
plenty of water).
Adverse Effects Toxicity is mainly due
to partial inhibition of
cellular DNA polymerase. Anaemia and neutropenia are the most important and
doserelated adverse effects.
Nausea, anorexia, abdominal pain, headache, insomnia and myalgia
are common at the start of therapy but diminish later.
Myopathy, lactic acidosis, hepatomegaly, convulsions and
encephalopathy are infrequent.
Interactions Paracetamol increases AZT toxicity, probably by competing for glucuronidation.
Azole antifungals also inhibit AZT metabolism. Other nephrotoxic and
myelosuppressive drugs and probenecid enhance toxicity. Stavudine and
zidovudine exhibit mutual antagonism by competing for the same activation
pathway.
Use
Zidovudine is used in HIV infected patients only in combination with at least 2 other ARV
drugs. However, its efficacy as monotherapy in AIDS has been confirmed in the
past. HIVRNA titer is reduced to undetectable levels and CD4 count increases
progressively. Immune status is improved and opportunistic infections become
less common. There is a sense of wellbeing and patients gain weight. AZT also
reduces neurological manifestations of AIDS and new Kaposi’s lesions do not
appear. Mortality among AIDS patients is reduced. It has also been shown to
slow the progression of HIV infection, including escalation of ARC to full
blown AIDS. However, beneficial effects are limited from a few months to a couple
of years after which progressively non-responsiveness develops.
AZT, along with one or two other ARV drugs is the standard
choice for post exposure prophylaxis of HIV, as well as mother to offspring
transmission.
Didanosine (ddI) It is a purine nucleoside analogue which after intracellular conversion
to didanosine triphosphate
competes with ATP for incorporation in viral DNA, inhibits HIV reverse
transcriptase and terminates proviral DNA. Antiretroviral activity of
didanosine is equivalent to AZT. Mutational resistance develops, but only few
AZT resistant mutants are nonresponsive to didanosine also. Now it is used only
in combination regimens.
Dose: 200 mg BD (for > 60 kg BW), 125 mg BD (< 50 kg BW) 1 hour before or 2 hour after meals.
DINEX EC, DDRETRO,
VIROSINE DR 250 mg, 400 mg tabs.
Oral absorption of
didanosine is somewhat erratic due to acid lability. It is metabolized as well
as excreted unchanged; t½ 1 to 1.5 hr. In contrast to AZT, it does not cause
myelosuppression. The major doserelated toxicity is peripheral neuropathy and
rarely pancreatitis. Diarrhoea, abdominal pain and nausea are the side effects.
Stavudine (d4T) It is also a thymidine
analogue which acts in the same
way as AZT. By utilizing the same thymidine kinase for activation, AZT
antagonises the effect of stavudine. Resistance to stavudine develops as for
other NRTIs.
It is well absorbed
orally and rapidly metabolized (t½ 1.5 hr). The antiHIV efficacy of stavudine
is comparable to AZT, and it is used in combination regimens. Peripheral
neuropathy, lipodystrophy and rarely pancreatitis are the serious toxicies which
have restricted its use.
Dose: 40 mg BD ( > 60 kg
BW), 30 mg BD (< 60 kg BW) STAG, STAVIR, VIROSTAV
30, 40 mg caps.
Lamivudine (3TC) This deoxycytidine
analogue is phosphorylated
intracellularly and inhibits HIV reverse transcriptase as well as hepatitis B
virus (HBV) DNA polymerase. Its incorporation into DNA results in chain
termination. Most human DNA polymerases are not affected and systemic toxicity
of 3TC is low. Point mutation in HIVreverse transcriptase and HBVDNA polymerase
gives rise to rapid lamivudine resistance. Certain lamivudineresistant mutants
become slow growing. Some crossresistance with ddI has been noted among HIV.
Oral bioavailability of 3TC is high and plasma t½ longer (6–8
hours). Intracellular t½ is still longer (> 12 hr). It is mainly excreted
unchanged in urine.
Lamivudine is used in combination with other antiHIV drugs, and
appears to be as effective as AZT. It is also frequently used for chronic
hepatitis B. HBVDNA titre is markedly reduced and biochemical as well as histological
indices of liver function improve. However, viral titres rise again after
discontinuation. Even with continued medication HBV viraemia tends to return
after 1 year due to emergence of resistant mutants.
Dose: For chronic hepatitis
B—100 mg OD For HIV infection— 150 mg
BD.
LAMIVIR 150 mg tab, 150 mg/ 5 ml soln; LAMIVIRHBV 100 mg tab;
HEPTAVIR, LAMIDAC, LAMUVID, VIROLAM 100, 150 mg tabs;
Lamivudine is generally well tolerated. Side effects are
few—headache, fatigue, nausea, anorexia, abdominal pain. Pancreatitis and
neuropathy are rare. Hematological toxicity does not occur.
Abacavir (ABC) This guanosine analogue
is a potent ARV drug that
acts after intracellular conversion to carbovir triphosphate. Resistance to ABC
develops slowly, and it exhibits little cross resistance with other NRTIs. Its
oral bioavailability is 80% and it is mainly eliminated by metabolism. The
plasma t½ is 1–1.5 hour, but intracellular t½ of active metabolite is >12
hours. Hypersensitivity reactions such as rashes, fever, flulike symptoms are
the major problems. Some fatalities have occurred when patients developing the
reaction were given further doses of ABC. Avoidance of alcohol is advised.
Dose: 300 mg BD or 600 mg
OD.
ABAVIR, ABAMUNE 300 mg
tab.
NON-NUCLEOSIDE REVERSE TRANSCRIPTASE INHIBITORS (NNRTIS)
Nevirapine (NVP) and Efavirenz (EFV) These are nucleoside unrelated compounds which directly
inhibit HIV reverse transcriptase without the need for intracellular
phosphorylation. Their locus of action on the enzyme is also different. They
are more potent than AZT on HIV1, but do not inhibit HIV2. Viral resistance to
these drugs develops by point mutation and cross resistance is common among
different NNRTIs, but not with NRTIs or PIs.
Nevirapine is well
absorbed orally and is extensively metabolized in liver with a t½ of 30 hours.
Oral absorption of efavirenz is incomplete (50%), but t½ is longer (48 hours)
and it is totally metabolized. Both NVP and EFV modestly induce CYP 3A4, 2D6
enzymes and enhance their own metabolism as well as that of other drugs.
The NNRTIs are
indicated in combination regimens for HIV, and have succeeded in reducing HIVRNA
levels when an earlier regimen has failed.
Nevirapine Dose 200 mg/day, may be increased later to 200 mg BD.
NEVIMUNE, NEVIVIR,
NEVIPAN, NEVIRETRO 200 mg tab
Rashes (commonest),
nausea, headache are the usual side effects. Fever and rise in liver enzymes
can occur. Nevirapine is potentially hepatotoxic. Avoid enzyme inducers
(rifampin) and enzyme inhibitors (ketoconazole).
Efavirenz: Dose 600 mg OD on empty stomaCh. No. EFAVIR, VIRANZ 200 mg tab., EVIRENZ 200 mg
cap, 600 mg tab.
Side effects are
headache, rashes, dizziness, insomnia and a variety of neuropsychiatric
symptoms. It induces the metabolism of certain drugs and inhibits that of
others.
RETROVIRAL PROTEASE INHIBITORS (PIS)
An aspartic protease
enzyme encoded by HIV is involved in the production of structural proteins and
enzymes (including reverse transcriptase) of the virus. The large viral
polyprotein is broken into various functional components by this enzyme. This
protease acts at a late step in HIV replication, i.e. maturation of the new
virus pCh. No.s when the RNA genome acquires the core proteins and enzymes.
Five protease inhibitors—Indinavir (IDV),
Nelfinavir (NFV), Saquinavir (SQV),
Ritonavir (RTV) and Lopinavir (in
combination with ritonavir LPV/r) have been marketed in India for use against
HIV. They bind to the protease molecule, interfere with its cleaving function,
and are more effective viral inhibitors than AZT. Because they act at a late
step of viral cycle, they are effective in both newly and chronically infected
cells. Under their influence, HIV-infected cells produce immature noninfectious
viral progeny—hence prevent further rounds of infection.
Oral bioavailability of PIs is variable (IDV and RTV ~65%, NFV
>20%, SQV 15%) and their plasma t½ ranges from 2–5 hours. All are
extensively metabolized by CYP3A4 and other CYP isoenzymes. All (especially
ritonavir and lopinavir) are potent inhibitors of CYP3A4, while few other CYP
isoenzymes are induced. The PIs interact with many drugs. Nelfinavir and ritonavir
induce their own metabolism.
Monotherapy with one of these drugs in previously AZT treated
patients reduced HIV viral levels, increased CD4 cell count and improved the
clinical condition. However, viral resistance developed against the PIs over months
due to selection of resistant mutants in a stepwise manner. Combination of
NRTIs with PIs has been found more effective than either drug given alone, and
triple therapy is more effective than double therapy. Current recommendations
are to use a PI in combination with either two NRTIs or one NRTI + one NNRTI.
Because different PIs both inhibit and induce specific CYP isoenzymes
to different extents, drug interactions with them are common and often
unpredictable. Manufacturer’s package inserts should be consulted while co-prescribing
any other drug. Specifically, metabolism of PIs is induced by rifampin and
other enzyme inducers rendering them ineffective. Another problem in their use
is the large tablet load. In case of different PIs, 6–18 tablets are to be
taken daily, some on empty stomach, but others with meals; and this has to go
on for months and years. Patient acceptability and compliance are often low.
One of the strategies adopted to reduce the dose of IDV, LPV and SQV is to
combine them with a low and subtherapeutic dose (100 mg) of ritonavir. By
reducing first pass metabolism, ritonavir increases the bioavailability of the
companion PI. This ‘boosted PI regimen’ permits reduction in the
number/frequency of tablets to be taken each day. Lopinavir is marketed only in
combination with ritonavir. Nelfinavir is not to be combined with ritonavir.
The most prominent adverse
effects of PIs are gastrointestinal intolerance, asthenia, headache, dizziness,
limb and facial tingling, numbness and rashes. Of particular concern are
lipodystrophy (abdominal obesity, buffalo hump with wasting of limbs and face)
and dyslipidaemia (raised triglycerides and cholesterol) which may necessitate
hypolipidaemic drugs. Diabetes may be exacerbated. Indinavir crystalises in urine
and increases risk of urinary calculi.
Indinavir It is to be taken on empty stomach; g.i. intolerance is common; excess fluids must be
consumed to avoid nephrolithiasis.
Dose: 800 mg TDS (BD if
taken with 100 mg RTV).
INDIVAN, INDIVIR,
VIRODIN 400 mg cap.
Nelfinavir It is to be taken with meals and bioavailability is erratic. Often produces
diarrhoea and flatulence; clinical efficacy may be somewhat lower than other
PIs.
Dose: 750 mg TDS; NELFIN, NELVIR, NEIVEX
250 mg tab.
Ritonavir It is a potent PI; also a potent CYP3A4 inhibitor. Drug interactions, nausea,
diarrhoea, paresthesias, fatigue and lipid abnormalities are prominent.
Dose: 600 mg BD, to be taken
with food.
RITOMUNE, RITOMAX 100
mg cap; RITOVIR 250 mg tab.
Saquinavir Two types of formulations (hard gel and soft gel capsules) with differing, but low
oral bioavailability have been produced. The tablet load is large and side
effects are frequent; photosensitivity can occur. It is a weak inhibitor of CYP3A4.
Dose: 1200 mg TDS on full stomach;
1000 mg BD (with RTV 100 mg).
SAQUIN 200 mg tab.
Lopinavir It is available only in combination with RTV to improve bioavailability.
Diarrhoea, abdominal pain, nausea and dyslipidaemias are more common.
Dose: 400 mg (with ritonavir
100 mg) BD with food.
RITOMAXL: lopinavir
133.3 mg + ritonavir 33.3 mg cap.
