Anthelmintic Drugs
| Home | | Pharmacology |Chapter: Essential pharmacology : Antiamoebic And Other Antiprotozoal Drugs
Anthelmintics are drugs that either kill (vermicide) or expel (vermifuge) infesting helminths.
ANTHELMINTIC DRUGS
Anthelmintics are
drugs that either kill (vermicide) or expel (vermifuge) infesting helminths.
Helminthiasis is
prevalent globally (1/3rd of world’s population harbours them), but is more
common in developing countries with poorer personal and environmental hygiene.
Multiple infestations in the same individual are not infrequent. In the human
body, g.i.t. is the abode of many helminths, but some also live in tissues, or
their larvae migrate into tissues. They harm the host by depriving him of food,
causing blood loss, injury to organs, intestinal or lymphatic obstruction and
by secreting toxins. Helminthiasis is rarely fatal, but is a major cause of ill
health.
Malefern and
chenopodium had been used for worm infestations for centuries. Many drugs were
discovered in the early part of the present century. However, over the past 4
decades many new, highly efficacious and well tolerated anthelmintics have been
developed. These have largely replaced the older drugs. The choice of drug for
each worm infestation is based not only on efficacy, but also on lack of side effects/toxicity,
ease of administration (preferably single dose) and low cost.
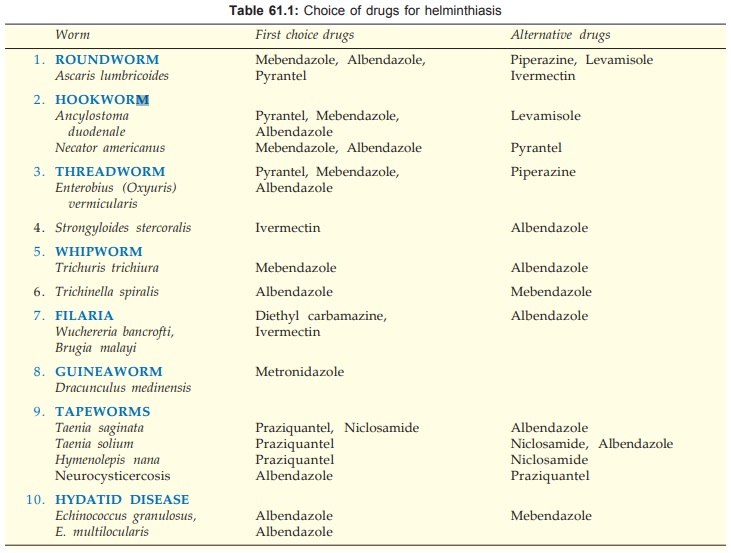
Development of
resistance has not been a problem in the clinical use of anthelmintics. The
current choice of drugs for worm infestations common in the Indian subcontinent
is given in Table 61.1.
Mebendazole
It is a benzimidazole
introduced in 1972. This congener of thiabendazole became very popular because
it retained the broad-spectrum anthelmintic activity but not the toxicity of
its predecessor. It has produced nearly 100% cure rate/reduction in egg count
in roundworm, hook worm (both species), Enterobius
and Trichuris infestations, but is
much less active on Strongyloides.
Upto 75% cure has been reported in tapeworms, but H. nana is relatively insensitive. It expels Trichinella spiralis from intestines, but efficacy in killing
larvae that have migrated to muscles is uncertain. Prolonged treatment has been
shown to cause regression of hydatid cysts in the liver. Treatment after
resection of the cyst may prevent its regrowth.
The immobilizing and lethal action of mebendazole on worms is rather slow: takes 2–3 days to develop. It acts probably by blocking glucose uptake in the parasite and depletion of its glycogen stores. Intracellular microtubules in the cells of the worm are gradually lost. The site of action of mebendazole appears to be the microtubular protein ‘βtubulin’ of the parasite. It binds to βtubulin of susceptible worms with high affinity and inhibits its polymerization.
Hatching of nematode eggs and their larvae are also inhibited.
Ascaris ova are killed.
Pharmacokinetics
Absorption of mebendazole from intestines is
minimal; 75–90% of an oral dose is passed in the faeces. The fraction absorbed
is excreted mainly as inactive metabolites in urine/ faeces.
Adverse Effects
Mebendazole is well tolerated even by patients in poor
health. Diarrhoea, nausea and abdominal pain have attended its use in heavy
infestation. Incidents of expulsion of Ascaris
from mouth or nose have occurred, probably due to starvation of the parasite
and their slow death. Allergic reactions, loss of hair and granulocytopenia
have been reported with high doses.
Safety of mebendazole during pregnancy is not known, but it is
contraindicated on the basis of animal data.
Uses And Administration: Mebendazole
is available as: MEBEX, WORMIN 100 mg chewable
tab and
100 mg/5 ml suspension. MEBAZOLE 100 mg tab
The dose and duration of treatment is the same for children
above 2 years as for adults; ½ dose for 1–2 yr age.
Roundworm
Hookworm
Whipworm
*100 mg twice a day for 3
consecutive days. No fasting, purging or any other preparation of the patients
is needed.
Enterobius: 100 mg single dose,
repeated after 2–3 weeks (to kill the
ova that have developed later). Strict hygienic measures and simultaneous treatment
of all children in the family or class is advocated to cut down autoinfection
and person to person infection. This holds true of enterobiasis, irrespective
of drug used.
Trichinella spiralis: 200 mg BD for 4 days;
less effective than albendazole.
Hydatid disease: 200–400 mg BD or TDS
for 3–4 weeks; less effective than
albendazole.
Mebendazole is one of the preferred drugs for treatment of
multiple infestations and is more effective than albendazole in trichuriasis.
It has also been used for mass treatment, but need for multiple doses is a
drawback.
Albendazole
It is a subsequently introduced congener of mebendazole: retains
the broad-spectrum activity and excellent tolerability of its predecessor, and
has the advantage of single dose administration in many cases. One dose treatment
has produced cure rates in ascariasis, hookworm (both species) and enterobiasis
which are comparable to 3 day treatment with mebendazole. Results in trichuriasis
have been inferior to mebendazole. In strongyloidosis, it is more effective
than mebendazole: a 3 day course has achieved nearly 50% cure, and a second
course repeated after 3 weeks cured practically all patients. Three day
treatment has been found necessary for tapeworms including H. nana. Results in hydatid disease and hookworm have been superior to mebendazole. Albendazole
has weak microfilaricidal action, kills cysticerci, hydatid larvae, ova of
ascaris/hookworm and is also effective in cutaneous larva migrans. The
mechanism of action of albendazole is similar to that of mebendazole.
Absorption of albendazole after oral administration is moderate,
but inconsistent. It is enhanced when the drug is taken with fatty meal (may
help in treating neurocysticercosis and hydatid disease). The fraction absorbed
is converted by first pass metabolism to its sulfoxide metabolite which is
active in contrast to the metabolites of mebendazole and thiabendazole.
Albendazole sulfoxide is widely distributed in the body, enters brain and is
excreted in urine with a t½ of 8.5 hours. Thus, albendazole is able to exert
antihelmintic activity in tissues as well.
Albendazole is well
tolerated; only gastrointestinal side effects have been noted. Few patients
have felt dizziness. Prolonged use, as in hydatid or in cysticercosis, has
caused headache, fever, alopecia, jaundice and neutropenia.
ZENTEL, ALMINTH,
ALBEZOLE, COMBANTRINA 400 mg tab, 200 mg/5 ml suspension.
No preparation or post-drug
fasting/ purging is required. For intestinal worms it should be given on empty
stomach, while for cysticercosis, hydatid and cutaneous larva migrans it should
be given with a fatty meal.
Ascaris,
hookworm, Enterobius and Trichuris: a single dose of 400 mg (for adults and children above 2 yrs, 200 mg
for 1–2 yr age).
Tapeworms and
strongyloidosis: 400 mg daily for 3 consecutive days.
Trichinosis: Three day treatment
expels the adult worm from intestine, but has limited effect on larvae that
have migrated to muscles. They are not killed but symptomatic relief occurs.
Corticosteroids are added if systemic manifestations are severe.
Neurocysticercosis: Albendazole is the
anthelmintic of choice for the treatment of neurocysticercosis (see later). Usually 8–15 days course of
400 mg BD (15 mg/kg/day) is employed. Cysticercosis of other tissues (muscles,
subcutaneous area) also responds, but no drug should be given for ocular
cysticercosis—blindness can occur due to the reaction.
Cutaneous larva
migrans: Albendazole 400 mg daily for 3 days is the drug of choice; kills
larvae and relieves symptoms.
Hydatid disease: 400 mg BD for 4
weeks, repeat after 2 weeks (if required), up to 3 courses. It is the preferred
treatment given before and after surgery as well as to inoperable cases.
Filariasis: Added to
diethylcarbamazine (DEC) or ivermectin, albendazole has adjuvant value in
treating lymphatic filariasis. A single dose of its combination with either DEC
or ivermectin given yearly has been used in mass programmes to suppress micro-filaraemia
and disease transmission.
Because it has exhibited
embryotoxicity in animals, use in pregnant women is contraindicated. It should
be given with caution to patients with hepatic or renal disease.
Thiabendazole
It was the first
benzimidazole poly-anthelmintic introduced in 1961, which covered practically
all species of nematodes infesting the g.i.t.—roundworm, hookworm, Enterobius, Trichuris, Strongyloides and
Trichinella spiralis. It also inhibits
development of the eggs of worms and kills larvae. Thiabendazole affords
symptomatic relief in cutaneous larva migrans and skeletal muscle symptoms
produced by migration of Trichinella spiralis
larvae to muscles. Symptomatic relief also occurs in guinea worm disease.
The mechanism of
action of thiabendazole is the same as described for mebendazole. Thiabendazole
has anti-inflammatory, analgesic and antipyretic actions. These may contribute to
its effect in cutaneous larva migrans and other inflammatory conditions
produced by larvae or worms in tissues.
Since thiabendazole is
well absorbed from g.i.t., systemic adverse effects are frequent and often
interfere with normal activity.
Nausea, vomiting, loss
of appetite, headache, giddiness are most common. It can impair
alertness—driving and operation of machinery should be prohibited.
Itching, abdominal pain,
diarrhoea and a variety of other symptoms are also produced.
Dose 25 mg/kg/day in two
divided doses taken after meals. Tablets must be
chewed;
Uses
Because of frequent
side effects and poor patient acceptability,
thiabendazole is used only when other better tolerated drugs are ineffective.
1. Strongyloidosis
2. Cutaneous larva migrans
3. Trichinosis—intestinal
infestation and larvae in muscles
*Give a 2 day course. If inadequate,
repeat after a gap of 2 days.
Trichinella larvae in muscles are often
not killed, but symptomatic relief
occurs quickly.
Pyrantel Pamoate
It was introduced in
1969 for threadworm infestation in children; use soon extended to roundworm and
hookworm as well. Efficacy against Ascaris,
Enterobius and Ancylostoma is
high and comparable to that of mebendazole. Lower cure rates (about 60%) have
been obtained in case of Necator
infestation. It is less active against Strongyloides
and inactive against Trichuris and other worms.
Pyrantel causes
activation of nicotinic cholinergic receptors in the worms resulting in
persistent depolarization → slowly developing contracture and spastic
paralysis. Worms are then expelled. An anticholinesterase action has also been
demonstrated. Because piperazine causes hyperpolarization and flaccid paralysis,
it antagonizes the action of pyrantel. Cholinergic receptors in mammalian
skeletal muscle have very low affinity for pyrantel.
Only 10–15% of an oral
dose of pyrantel pamoate is absorbed: this is partly metabolized and excreted
in urine.
Adverse Effects
Pyrantel pamoate is
remarkably free of side effects:
occasional g.i. symptoms, headache and dizziness is reported. It is tasteless,
nonirritant; abnormal migration of worms is not provoked. Its safety in
pregnant women and in children below 2 years has not been established.
Use And Administration
For Ascaris, Ancylostoma and Enterobius:
a single dose of 10 mg/kg is recommended. A 3 day course for Necator and for Strongyloides has been suggested.
No fasting, purging or
other preparation of the patient is needed.
NEMOCID, ANTIMINTH,
EXPENT 250 mg tab, 50 mg/ ml suspension (10 ml bottle).
Piperazine
Introduced in 1950, it
is a highly active drug against Ascaris
and Enterobius; achieves 90–100% cure
rates. However, it is now considered a second choice drug even for these worms.
Piperazine causes hyperpolarization of Ascaris
muscle by a GABA agonistic action opening Cl¯ channels that causes relaxation
and depresses responsiveness to contractile action of ACh. No. Flaccid
paralysis occurs and worms are expelled alive. They recover if placed in
piperazine free medium. Therefore, often a purgative (senna) is given with it,
but is not necessary. No fasting or patient preparation is required. Piperazine
does not excite Ascaris to abnormal
migration. It does not affect neuromuscular transmission in man.
Pharmacokinetics
A considerable
fraction of the oral dose of
piperazine is absorbed. It is partly metabolized in liver and excreted in
urine.
Adverse Effects
Piperazine is safe and
well tolerated. Nausea, vomiting, abdominal discomfort and urticaria are occasional.
Dizziness and
excitement occur at high doses; toxic doses produce convulsions; death is due
to respiratory failure. It is contraindicated in renal insufficiency and in
epileptics, but is safe in the pregnant.
Dose: For roundworm
infestation 4 g once a day for 2 consecutive days;
children 0.75 g/year of age (max. 4 g) is considered curative. Because of its
capacity to relax ascarids, it is of particular value in intestinal obstruction
due to roundworms. It can be used during pregnancy while other drugs cannot be
used.
Enterobiasis—50 mg/kg
(max. 2 g) once a day for 7 days or 75 mg/kg (max. 4 g) single dose, repeated
after 3 weeks.
PIPERAZINE CITRATE
0.75 g/5 ml elixir in 30 ml, 115 ml bottle; 0.5 g (as phosphate) tablets; Combination of any
other anthelmintic (except piperazine) with a purgative in the same formulation
is banned in India.
Levamisole, Tetramisole
Tetramisole was
developed in the late 1960s. It is recemic; its levo isomer (levamisole) was
found to be more active and is preferred now. Both are active against many
nematodes, but use is restricted to ascariasis and ancylostomiasis, because
action on other worms is poor. Strongyloides
larvae are killed, but adult worms are
not sensitive. The ganglia in worms are stimulated causing tonic paralysis and
expulsion of live worms. Interference with carbohydrate metabolism (inhibition
of fumarate reductase) may also be contributing.
Uses
For Ascaris infestation a single dose of levamisole 50 mg for children 10–19 kg body
weight, 100 mg for 20–39 kg and 150 mg for >40 kg and adults is advocated.
It achieves >90% cure rate.
Levamisole is a second
line drug for A. duodenale; 2 doses
at 12 hour interval are suggested— achieves 70–90% cure. It is less efficacious
against Necator.
Tetramisole: DECARIS 50, 150 mg tab.
Levamisole: DEWORMIS, VERMISOL 50, 150 mg tab, 50 mg/5 ml syr.
Levamisole is an
immunomodulator as well: restores depressed T cell function. It was used as a
disease modifying drug in rheumatoid arthritis and as an adjunct in malignancies,
aphthous ulcers and recurrent herpes, but repeated doses produce severe
reactions; not used now.
Adverse Effects
One or two doses used
in helminthiasis are well
tolerated. Incidence of side effects—nausea, abdominal pain, giddiness,
fatigue, drowsiness or insomnia is low.
Diethyl Carbamazine Citrate (DEC)
Developed in 1948, it
is the first drug for filariasis. DEC is absorbed after oral ingestion,
distributed all over the body (V = 3–5 L/kg), metabolized in liver and excreted
in urine. Excretion is faster in acidic urine. Plasma t½ of usual clinical
doses is 4–12 hours, depending on urinary pH.
Diethylcarbamazine has
a highly selective effect on microfilariae (Mf). A dose of 2 mg/kg TDS clears
Mf of W. bancrofti and B. malayi from peripheral blood in 7 days.
However, Mf present in nodules and transudates (hydrocoele) are not killed. The
most important action of DEC appears to be alteration of Mf membranes so that
they are readily phagocytosed by tissue fixed monocytes, but not by circulating
phagocytes. Muscular activity of the Mf and adult worms is also affected
causing hyperpolarization due to the piperazine moiety, so that they are
dislodged. Prolonged treatment may kill adult B. malayi and probably W.
bancrofti worms also.
DEC is active against
Mf of Loa loa and Onchocerca volvulus. The adult worm of L. loa but not O. volvulus is
killed. DEC reduces worm burden in ascariasis, but efficacy is low.
Uses
Filariasis: 2 mg/kg TDS produces
rapid symptomatic relief; Mf
disappear from blood and patient becomes noninfective to mosquitoes in 7 days.
However, the adult worm survives in the lymphatics and gives rise to
intermittent micro-filaraemia and symptoms. Prolonged treatment with different
schedules has been found to achieve radical cure in most patients. A total dose
of 72–126 mg/kg spread over 12 days to 3 weeks has been found satisfactory;
more than one course may be needed with a gap of 3–4 weeks. Elephantiasis due
to chronic lymphatic obstruction is not affected by DEC, because fibrosis of lymphatics
is irreversible. Yearly treatment with a combination of DEC and albendazole on
mass scale has brought down transmission of filariasis by reducing micro-filaraemia.
Tropical
Eosinophilia: DEC (2–4 mg/kg TDS) for 2–3 weeks produces dramatic improvement in the signs and symptoms
of eosinophilic lung or tropical eosinophilia. The benefit probably reflects
anti-microfilarial action: the symptoms of the disease being presumably due to
reaction to the Mf.
HETRAZAN, BANOCIDE 50, 100 mg tab, 120 mg/5 ml syr; 50 mg/ 5 ml pediatric
syr; to be taken after meals.
Loa loa and O. volvulus infections can also be treated with DEC, but it is imperative
to give small (25–50 mg) test dose initially to avoid severe reaction to dying
Mf. Ivermectin does not produce such severe reactions and is preferred for
initial treatment.
Adverse Effects
These are common but generally not serious. Nausea,
loss of appetite, headache, weakness and dizziness are the usual complaints.
A febrile reaction with rash, pruritus, enlargement of lymph nodes
and fall in BP may occur due to mass destruction of Mf and adult worms. This is
usually mild, but may be severe. The reaction can be minimized by starting with
a low dose (0.5 mg/kg). When it occurs, DEC should be temporarily withheld and
antihistaminics and/ or corticosteroids given. Subsequent administration of DEC
does not cause such reaction. Leukocytosis and mild albuminuria are also noted.
Ivermectin
It is an extremely
potent semisynthetic derivative of the anti-nematodal principle obtained from Streptomyces avermitilis, that has been
used in other countries for long, but marketed in India only recently.
Ivermectin is the drug of choice for single dose treatment of onchocerciasis
and strongyloidosis, and is comparable to DEC for bancroftian and brugian filaria.
It is also highly effective in cutaneous larva migrans and ascariasis, while
efficacy against Enterobius and Trichuris is moderate. Certain insects,
notably scabies and head lice are
killed by ivermectin.
Nematodes develop
tonic paralysis when exposed to ivermectin. It acts through a special type of
glutamate gated Cl¯ channel found only in invertebrates. Such channels are not
involved in the motor control of flukes and tapeworms which are unaffected by
ivermectin. Potentiation of GABAergic transmission in the worm has also been
observed. The lack of GABA-related actions in man could be due to its low
affinity for mammalian GABA receptors and its exclusion from the brain,
probably by P-glycoprotein mediated efflux at the blood brainbarrier.
A single 10–15 mg (0.2
mg/kg) oral dose of ivermectin, preferably with 400 mg albendazole, given
annually for 5–6 years has been used for filariasis. Single 0.15–0.2 mg/kg dose
has yielded highest cure rate in strongyloidosis and reduces burden of other intestinal
nematodes as well.
Ivermectin has
replaced DEC for onchocerciasis and has been used in the ‘river blindness’
control programme of WHO in Africa and Latin America. One dose of ivermectin is
given at 6–12 month intervals—produces long lasting reduction of Mf counts in
eye and skin, without affecting the adult worm. Though it does not cure O. volvulus infection, ocular
inflammation/damage as well as lymphadenopathy
are suppressed with only mild ocular or systemic reactions.
Ivermectin is the only drug effective orally in scabies and
pediculosis. Single 0.2 mg/kg dose cures most patients.
IVERMECTOL, IVERMEC, VERMIN 3, 6 mg tabs; to be taken on empty stomaCh.
No.
Ivermectin is well absorbed orally, widely distributed in the
body, but does not enter CNS, sequestrated in liver and fat, and has a long
terminal t½ of 48–60 hours. Side effects have been mild—pruritus, giddiness,
nausea, abdominal pain, constipation, lethargy and transient ECG changes, but
more important are the reactions due to degeneration products of the Mf, which
are similar to those occurring after DEC.
Niclosamide
Niclosamide is a
highly effective drug against cestodes infesting man—Taenia saginata, T. solium,
Diphyllobothrium latum and Hymenolepis nana, as well as threadworm. The drug appears to
act by inhibiting oxidative phosphorylation in mitochondria and interfering
with anaerobic generation of ATP by the tapeworm. Injured by niclosamide, the
tapeworms are partly digested in the intestine. In cases of T. solium, digestion of the dead segments
can be hazardous, because the ova released from them may develop into larvae in
the intestine, penetrate its wall and cause visceral cysticercosis. Many
experts do not use niclosamide now for T.
solium infestation.
Regimen For Tapeworm: Niclosamide is available
as 0.5 g tab (NICLOSAN). After a light
breakfast, 2 tablets are to be chewed and swallowed with water, followed by
another 2 tablets after 1 hr (total 2 g); total dose for children 2–6 years is
1 g. A saline purge is given 2 hours after the later dose to wash off the worm.
The scolex should be searched in the stools to be sure that the worm will not
grow again. Cure rate of 85–95% has been obtained by one day treatment. A
thorough purge is essential in the cases of T.
solium so that all segments are passed out and cysticercosis does not occur. Because praziquantel does not lead
to digestion of the worm and kills encysted larvae as well, it is the drug of
choice for T. solium.
For H. nana, the 2 g dose is repeated daily
for 5 days. This is needed because cysticerci of H. nana (which are not affected by niclosamide) develop in the
jejunal villi of the same host and worms appear in the intestinal lumen after 4
days. However, no purgative is required. In some cases treatment may
have to be repeated after
10 days.
Praziquantel is now
preferred due to single dose treatment.
Adverse Effects
Niclosamide is
tasteless and nonirritating. It is
minimally absorbed from g.i.t.— no systemic toxicity occurs. It is well tolerated;
minor abdominal symptoms are produced occasionally. Malaise, pruritus and light
headedness are rare. Niclosamide is safe during pregnancy and in patients with
poor health.
Praziquantel
This novel
anthelmintic has wide ranging activity against Schistosomes, other trematodes, cestodes and their larval forms but
not nematodes. It is rapidly taken up by susceptible worms and appears to act
by causing leakage of intracellular calcium from the membranes → contracture and
paralysis. The tapeworms lose grip of the intestinal mucosa and are expelled.
Flukes and schistosomes are also dislodged in tissues and veins. Praziquantel
is active against adult as well as juvenile and larval stages of tapeworms.
At relatively higher
concentrations, it causes vacuolization of the tegument and release of the
contents of tapeworms and flukes followed by their destruction by the host.
This action appears to be more important in cases of schistosomes and flukes.
Pharmacokinetics
Praziquantel is
rapidly absorbed from intestines and absorption is enhanced by ingesting it
with food. It undergoes high first pass metabolism in liver which limits its
systemic bioavailability. Phenytoin, carbamazepine and possibly dexamethasone induce
praziquantel metabolism and further reduce its bioavailability. Patients of
neurocysticercosis are often receiving these drugs—may contribute to
therapeutic failure of praziquantel. It crosses bloodbrain barrier and attains
therapeutic concentrations in the brain and CSF. The plasma t½ is short (1.5
hours). Metabolites are excreted chiefly in urine.
Adverse Effects
Despite systemic
absorption, praziquantel has
exhibited no systemic toxicity.
It tastes bitter: can produce nausea and abdominal pain. Other
side effects are headache, dizziness and sedation. When used for schistosomes
and visceral flukes, symptoms like itching, urticaria, rashes, fever and
bodyache occur as a reaction to the destroyed parasites.
No interaction with food, alcohol or tobacco has been noted.
Uses
1. Tapeworms: Praziquantel
administered as a single dose has
achieved 90–100% cure rate in all human tapeworms. This level of activity is
similar to that of niclosamide and even better in case of H. nana.
T. saginata, T. solium: 10 mg/kg single dose
in morning. It is especially valuable in case of T. solium, because it kills the tapeworm larvae within the cysts and there are no chances of systemic
cysticercosis developing.
H. nana, D. latum: 15–25 mg/kg single
dose in morning. This is much simpler
compared to 5 day treatment needed with niclosamide for eradication of H. nana. In case of heavy infestation,
retreatment after one week is desirable.
2. Neurocysticercosis: Praziquantel was the
first drug found to be effective in
neurocysticercosis: 50–100 mg/kg daily in 3 divided doses for 15 days kills the
larvae lodged in brain and other tissues. However, it is now the 2nd choice
drug to albendazole (see below).
Praziquantel or albendazole are contraindicated in ocular
cysticercosis.
3. Schistosomes: All 3 species can be
treated with 40–75 mg/kg given once
or in instalments in one day.
4.
Other flukes: Praziquantel is the drug of choice for all schistosome and fluke
infestations except Fasciola hepatica.
The flukes respond to 75 mg/ kg/day given
for one day in most and two days in some cases.
CYSTICIDE 500 mg tab,
DISTOCIDE 600 mg tab.
