Amphotericin B (AMB)
| Home | | Pharmacology |Chapter: Essential pharmacology : Antifungal Drugs
The name polyene is derived from their highly double-bonded structure. Amphotericin B is described as the prototype.
AMPHOTERICIN B (AMB)
It is obtained from Streptomyces nodosus.
Chemistry And Mechanism Of Action
The polyenes possess a macrocyclic ring, one side of which has several conjugated double bonds and is highly lipophilic, while the other side is hydrophilic with many OH groups. A polar amino-sugar and a carboxylic acid group are present at one end in some. They are all insoluble in water and unstable in aqueous medium.
The polyenes have high affinity for ergosterol present in fungal cell membrane: combine with it, get inserted into the membrane and several polyene molecules together orient themselves in such a way as to form a ‘micropore’. The hydrophilic side forms the interior of the pore through which ions, amino acids and other water-soluble substances move out. The micropore is stabilized by membrane sterols which fill up the spaces between the AMB molecules on the lipophilic side—constituting the outer surface of the pore. Thus, cell permeability is markedly increased.
Cholesterol, present in host cell membranes, closely resembles ergosterol; the polyenes bind to it as well, though with lesser affinity. Thus, the selectivity of action of polyenes is low, and AMB is one of the most toxic systemically used antibiotics, though it is the least toxic polyene. Bacteria do not have sterols and are unaffected by polyenes. It has been found that AMB enhances immunity in animals, and this may aid immunocompromised individuals in handling fungal infection.
Antifungal Spectrum
AMB is active against a wide range of yeasts and fungi—Candida albicans, Histoplasma capsulatum, Cryptococcus neoformans, Blastomyces dermatitidis, Coccidioides immitis, Torulopsis, Rhodotorula, Aspergillus, Sporothrix, etc. Dermatophytes are inhibited in vitro, but concentrations of AMB attained in infected skin are low and ineffective. It is fungicidal at high and static at low concentrations.
Resistance to AMB during therapy has been rarely noted among Candida in a selected group of leucopenic cancer patients, but it is not a problem in the clinical use of the drug.
AMB is also active on various species of Leishmania.
Pharmacokinetics
AMB is not absorbed orally; it can be given orally for intestinal candidiasis without systemic toxicity. Administered i.v. as a suspension made with the help of deoxycholate (DOC), it gets widely distributed in the body, but penetration in CSF is poor. It binds to sterols in tissues and to lipoproteins in plasma and stays in the body for long periods. The terminal elimination t½ is 15 days. About 60% of AMB is metabolized in the liver. Excretion occurs slowly both in urine and bile, but urinary concentration of active drug is low.
Administration And Dose
Amphotericin B can be administered orally (50–100 mg QID) for intestinal moniliasis; also topically for vaginitis, otomycosis, etc.: FUNGIZONE OTIC 3% ear drops.
For systemic mycosis, it is available as dry powder along with DOC for extemporaneous dispersion before use: FUNGIZONE INTRAVENOUS, MYCOL 50 mg vial. It is first suspended in 10 ml water and then diluted to 500 ml with glucose solution (saline tends to make the suspension coarse). Initially 1 mg test dose is injected i.v. over 20 minutes. If no serious reaction follows, 0.3 mg/kg is infused over 4–8 hours. Daily dose may be gradually increased to 0.7 mg/kg depending on tolerance of the patient. The total dose of AMB for majority of cases is 3– 4 g given over 2–3 months.
Intrathecal injection of 0.5 mg twice weekly has been given in fungal meningitis.
New Amphotericin B Formulations
In an attempt to improve tolerability of i.v. infusion of AMB, reduce its toxicity and achieve targeted delivery, 3 new lipid formulations of AMB have been produced.
a) Amphotericin B Lipid Complex (ABLC): Contains 35% AMB incorporated in ribbon like pCh. No.s of dimyristoyl phospholipids.
b) Amphotericin B Colloidal Dispersion (ABCD): Disc shaped pCh. No.s containing 50% each of AMB and cholesteryl sulfate are prepared as aqueous dispersion.
c) Liposomal Amphotericin B (Small Unilamellar Vesicles; SUV): Consists of 10% AMB incorporated in uniform sized (60–80 nM) unilamellar liposomes made up of lecithin and other biodegradable phospholipids.
The special features of these preparations are:
• They, except ABCD, produce milder acute reaction (especially liposomal formulation) on i.v. infusion.
• They can be used in patients not tolerating infusion of conventional AMB formulation.
• They have lower nephrotoxicity.
• They cause minimal anaemia.
• The liposomal preparation delivers AMB particularly to reticulo-endothelial cells in liver and spleen—especially valuable for kala azar and in immuno-compromised patients.
However, some preparations, especially ABLC and ABCD, produce lower AMB levels and their clinical efficacy relative to conventional formulation appears to be lower. Though none of the above formulations is more effective in deep mycosis than conventional AMB, the liposomalAMB produces equivalent blood levels, has similar clinical efficacy with less acute reaction and renal toxicity. It thus appears more satisfactory, can be infused at higher rates (3–5 mg/kg/day), but is many times costlier than conventional AMB. Its specific indications are—as empirical therapy in febrile neutropenic patients not responding to antibacterial antibiotics, critically ill deep mycosis cases and in kala azar.
FUNGISOME (liposomal AMB) 10 mg, 25 mg, 50 mg per vial inj.
Adverse Effects
The toxicity of AMB is high.
a) Acute Reaction: This occurs with each infusion and consists of chills, fever, aches and pain all over, nausea, vomiting and dyspnoea lasting for 2–5 hour, probably due to release of cytokines (IL, TNFα). When these are severe—the dose is increased gradually. Usually the intensity of reaction decreases with continued medication. Injection of hydrocortisone 0.6 mg/kg with the infusion may reduce the intensity of reaction.
Thrombophlebitis of the injected vein can occur.
b) Long-Term Toxicity: Nephrotoxicity is the most important. It occurs fairly uniformly and is doserelated: manifestations are—azotemia, reduced g.f.r., acidosis, hypokalaemia and inability to concentrate urine. It reverses slowly and often incompletely after stoppage of therapy. Anaemia: Most patients develop slowly progressing anaemia which is due to bone marrow depression. It is largely reversible.
CNS toxicity: occurs only on intrathecal injection—headache, vomiting, nerve palsies, etc.
Uses
Amphotericin B can be applied topically for oral, vaginal and cutaneous candidiasis and otomycosis.
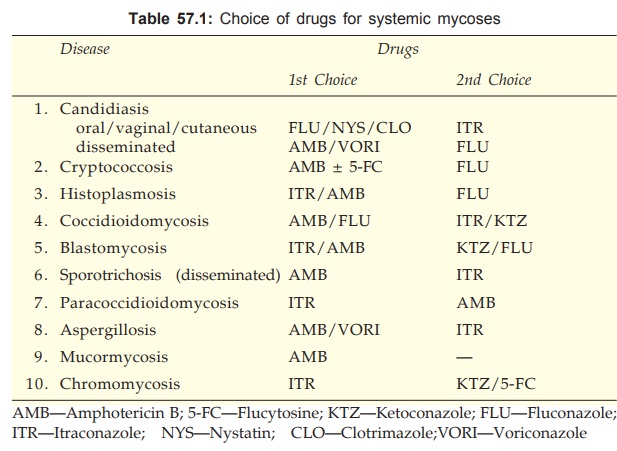
It is the most effective drug for various types of systemic mycoses and is the gold standard of antifungal therapy. However, because of higher toxicity of AMB, the azole antifungals are now preferred in conditions where their efficacy approaches that of AMB (see Table 57.1).
Leishmaniasis: AMB is the most effective drug for resistant cases of kala azar and mucocutaneous leishmaniasis (see Ch. No. 60).
Interactions
Flucytosine has supra-additive action with AMB in the case of fungi sensitive to both (AMB increases the penetration of 5FC into the fungus).
Rifampin and minocycline, though not antifungal in their own right, potentiate AMB action.
