Alternative routes of delivery
| Home | | Pharmaceutical Drugs and Dosage | | Pharmaceutical Industrial Management |Chapter: Pharmaceutical Drugs and Dosage: Drug delivery systems
For systemic action of drugs, the oral route has been the preferred route of administration.
Alternative routes
of delivery
For systemic action of drugs, the oral route has been the preferred route of administration. However, when administered by the oral route, many therapeutic agents are subjected to extensive presystemic elimination by GI degradation and/or hepatic metabolism. Delivery of drugs via the absorp-tive mucosa in various easily accessible body cavities (Figure 14.7), like the buccal, nasal, ocular, sublingual, rectal, and vaginal mucosae, offers distinct advantages over peroral administration for systemic drug delivery, since these alternative routes of drug delivery avoid the first-pass effect of drug clearance.
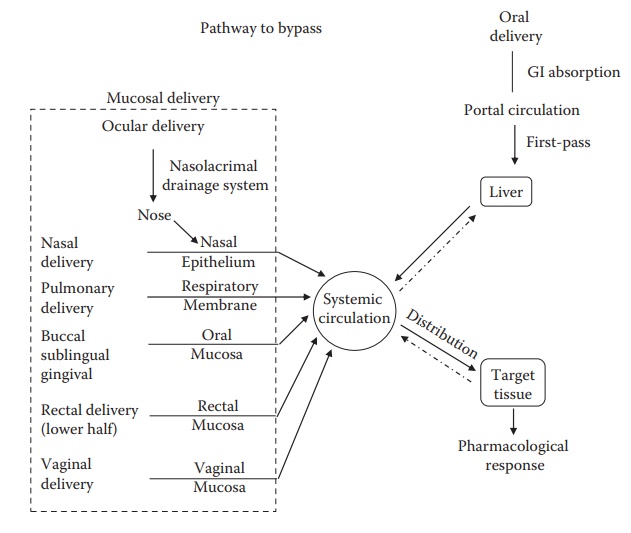
Figure 14.7 Various mucosal routes that bypass hepatic first-pass metabolism associated with oral administration.
Buccal and sublingual drug delivery
The buccal and sublingual mucosae in the oral cavity provide an excel-lent alternative for the delivery of certain drugs. Oral transmucosal absorption is generally rapid because of the rich vascular supply to the mucosa. These routes provide improved delivery for certain drugs that are inactivated by first-pass intestinal/hepatic metabolism or by proteolytic enzymes in the GI tract.
The
sublingual mucosa is relatively permeable and is suitable for delivery of
low-molecular-weight lipophilic drugs when a rapid onset of action with
infrequent dosing is required. Sublingual DDSs are generally of two differ-ent
designs: (a) rapidly disintegrating tablets and (b) soft gelatin capsules
filled with a drug in solution. Such systems create a very high drug
concen-tration in the sublingual region before the drug is systemically
absorbed across the mucosa. Therefore, rapidly disintegrating sublingual
tablets are frequently used for prompt relief from an acute angina attack.
The
buccal mucosa is considerably less permeable than the sublingual area and is
generally not able to provide rapid absorption properties. The buccal mucosa
has an expanse of smooth muscle and relatively immobile mucosa, which makes it
a more desirable region for retentive systems used for oral transmucosal drug
delivery. Thus, the buccal mucosa is suitable for sustained delivery
applications, delivery of less permeable molecules, and perhaps peptide drugs.
One of the major disadvantages associated with buccal drug is the low flux,
which results in low drug bioavailabil-ity. Therefore, buccal DDSs usually
include a penetration (permeability enhancer) to increase the flux of drugs
through the mucosa. Another limitation associated with this route of
administration is the poor drug retention at the site of absorption.
Consequently, bioadhesive polymers have been extensively employed in buccal
DDSs. The duration of mucosal adhesion depends on the type and viscosity of the
polymer used. Nicotine in a gum vehicle when chewed is absorbed through the
buccal mucosa. Glyceryl trinitrite has been found quite effective when
administered through this route.
Nasal drug delivery
Although
nasal route is traditionally used for locally acting drugs, this route is
getting more attention for the systemic delivery of various peptide drugs that
are poorly absorbed via the oral route. The major advantages of nasal
administration include the fast absorption, rapid onset of action, and
avoidance of hepatic and intestinal first-pass effects. There are three major
barriers to drug absorption across nasal mucosa. These include a physical
barrier composed of the mucus and epithelium, a temporal barrier con-trolling
the mucosal clearance, and an enzymatic barrier acting principally on protein
and peptide drugs. The physical barrier consists of a lipoidal pathway and an
aqueous pore pathway. Nasally administered drugs have to pass through the
epithelial cell layer to reach the systemic circulation. Nasal absorption of
weak electrolytes is dependent on the degree of ioniza-tion, with higher nasal
absorption of a drug at a pH lower than its pKa.
Dosage
forms for nasal absorption must deposit and remain in the nasal cavity long
enough to allow effective absorption. Commonly used dosage forms administered
through this route are nasal sprays and drops. The nasal spray deposits drug in
the proximal part of the nasal atrium, whereas nasal drops are dispersed
throughout the nasal cavity. A nasal spray requires that the particles have a
diameter larger than 4 μm
to be retained in the nose and to minimize the passage into the lungs. Nasal
sprays are commercially available for buserelin, desmopressin, oxytocin, and
calcitonin.
Pulmonary drug delivery
The
respiratory tract includes the nasal mucosa, hypopharynx, and large and small
airway structures (trachea, bronchi, bronchioles, and alveoli). This tract
provides a large mucosal surface for drug absorption. Lung epi-thelium is
highly permeable and has low metabolic activity compared with the liver and
intestine. With a large surface area and highly permeable mem-brane, alveolar
epithelium permits rapid absorption. This route of adminis-tration is useful
for treating pulmonary conditions and for drug delivery to other organs via the
circulatory systems. In general, lipid-soluble molecules are absorbed rapidly
from the respiratory tract, and thus, an increasing number of drugs is being
administered by this route, including bronchodi-lators (e.g., beclometasone),
corticosteroids, antibiotics, antifungal agents, antiviral agents, and
vasoactive drugs.
Since
the lung has a large surface area and a highly permeable mem-brane, the lung is
an ideal site for absorption of macromolecules, such as proteins, peptides,
oligonucleotides, and genes. For example, DNase alpha (Pulmozyme®, Genentech),
an enzyme used to reduce the viscosity of mucus in the airways of patients with
cystic fibrosis, is most effective when inhaled. This protein is thus delivered
directly to its site of action by nebuli-zation. The recent approval of inhaled
human insulin by the FDA for use in diabetes mellitus stands as a major
advancement in the field of pulmonary delivery of macromolecules and
systemically acting drugs.
Ocular drug delivery
Drugs
are usually topically applied to the eyes in the form of drops or ointments for
local action. Following topical administration, the drug is eliminated from the
eye by nasolacrimal drainage, tear turnover, produc-tive corneal absorption,
and nonproductive conjunctival uptake. There are two barriers to ocular drug adsorption:
(a) the blood–aqueous barrier and (b) the blood–retina barrier. The
blood–aqueous barrier is composed of the ciliary epithelium, the epithelium of
the posterior surface of the iris, and blood vessels within the iris. Drugs
enter the aqueous humor at the ciliary epithelium and at blood vessels. Many
substances are transported out of the vitreous humor at the retinal surface.
The
cornea and the conjunctiva are covered with a thin film, the tear film, which
protects the cornea from dehydration and infection. For drugs administered
through the topical route, the cornea is the main barrier to drug absorption.
The cornea consists of three parts: the epithelium, the stroma, and the
endothelium. Both the endothelium and the epithelium have high lipid content
and thus are penetrated by drugs in their union-ized lipid-soluble forms. The
stroma lying between these two structures has a high water content, and thus,
drugs that have to negotiate the corneal barrier successfully must be both
lipid soluble and water soluble to some extent.
Ocular
drug absorption depends on both drug ionization and tear turn-over. For
example, the pH 5 solution induces more tear flow than the pH 8 solution, thus
the concentration gradient is reduced, and transport of both ionized and
nonionized drugs is less at pH 5. The duration of drug action in the eye can be
extended by two approaches: (1) by reducing drainage using viscosity-enhancing
agents, suspensions, emulsions, ointments, and polymeric matrices and (2) by
improving corneal drug penetration using ionophores and liposomes.
Prodrug
derivatization can be employed to overcome low corneal per-meability of
water-soluble drugs. The drug molecules can be chemically modified to obtain
suitable structural configuration and physicochemical properties to afford
maximal corneal adsorption. However, a prodrug must be converted enzymatically
or chemically to the parent drug in vivo to elicit its effect. Choline
esterases, which are abundant in the corneal epithelium, can be used for delivery
of more lipophilic esterified prodrugs of water-soluble compounds to the eye.
Rectal drug delivery
Rectal
administration provides rapid absorption of many drugs and is an alternative
when oral administration is inconvenient because of the inability to swallow or
because of GI side effects such as nausea, vomit-ing, and irrigation. More
importantly, rectal drug administration has the advantage of minimizing or
avoiding hepatic first-pass metabolism. The rectal bioavailability of lidocaine
in human is 65%, as compared with an oral bioavailability of 30%. Rectal route
is used to administer diazepam to children who are suffering from epileptics,
in whom it is difficult to estab-lish IV access. However, rectal administration
of drugs is inconvenient and has irregular drug absorption. Moreover, rectal
administration should be avoided in immunosuppressed patients in whom even
minimal trauma could lead to the formation of an abscess.
Vaginal drug delivery
Vaginal
epithelium is permeable to a wide range of substances, including steroids,
prostaglandins, antibiotics, estrogens, and spermicidal agents. Most steroids
are readily absorbed by vaginal epithelium, leading to their higher
bioavailability compared with their oral administration, because of a reduced
first-pass metabolism. For drugs with high membrane permeability, vaginal
absorption is determined by permeability of the aqueous diffusion layer,
whereas for drugs with low membrane permeability, such as testosterone and
hydrocortisone, vaginal absorption is determined by mem-brane permeability.
Vaginal ointments and creams contain drugs such as anti-infectives, estrogenic
hormone substrates, and contraceptive agents. Contraceptive creams contain
spermicidal agents and are used just before intercourse.
Related Topics
