Adverse Drug Effects - Types
| Home | | Pharmacology |Chapter: Essential pharmacology : Adverse Drug Effects
These are unwanted but often unavoidable pharmacodynamic effects that occur at therapeutic doses. They can be predicted from the pharmacological profile of a drug and are known to occur in a given percentage of drug recipients. Reduction in dose generally ameliorates the symptoms.
ADVERSE DRUG EFFECTS -
TYPES
Adverse drug effects
may be categorized into:
1. Side Effects
These are unwanted but
often unavoidable pharmacodynamic effects that occur at therapeutic doses. They
can be predicted from the pharmacological profile of a drug and are known to
occur in a given percentage of drug recipients. Reduction in dose generally
ameliorates the symptoms.
A side effect may be
based on the same action as the therapeutic effect, e.g. atropine is used in
pre-anaesthetic medication for its antisecretory action. The same action
produces dryness of mouth as a side effect. Acetazolamide acts as a diuretic by
promoting bicarbonate excretion— acidosis occurs as a side effect due to
bicarbonate loss.
Side effect may also
be based on a different facet of action, e.g. promethazine produces sedation
which is unrelated to its antiallergic action; estrogens cause nausea which is
unrelated to their anti-ovulatory action.
An effect may be
therapeutic in one context but side effect in another context, e.g. codeine
used for cough produces constipation as a side effect but the latter is its
therapeutic effect in traveller’s diarrhoea; depression of AV conduction is the
desired effect of digoxin in atrial fibrillation, but the same may be
undesirable when it is used for CHF.
Many drugs have been
developed from observation of side effects, e.g. early sulfonamides used as
antibacterial were found to produce hypoglycaemia and acidosis as side effects
which directed research resulting in the development of hypoglycaemic
sulfonylureas and carbonic anhydrase inhibitor—acetazolamide.
2. Secondary Effects
These are indirect
consequences of a primary action of the drug, e.g. suppression of bacterial
flora by tetracyclines paves the way for superinfections; corticosteroids
weaken host defence mechanisms so that latent tuberculosis gets activated.
3. Toxic Effects
These are the result
of excessive pharmacological action of the drug due to overdosage or prolonged
use. Overdosage may be absolute (accidental, homicidal, suicidal) or relative
(i.e. usual dose of gentamicin in presence of renal failure). The effects are
predictable and dose related. They result from functional alteration (high dose
of atropine causing delirium) or drug induced tissue damage (hepatic necrosis
from paracetamol overdosage). The CNS, CVS, kidney, liver, lung, skin and blood
forming organs are most commonly involved in drug toxicity.
Toxicity
may result from extension of the therapeutic effect itself, e.g. coma by barbiturates,
complete AV block by digoxin, bleeding due to heparin.
Another action may be
responsible for toxicity, e.g.—
Morphine
(analgesic) causes respiratory failure in overdosage.
Imipramine
(antidepressant) overdose causes cardiac arrhythmia.
Streptomycin
(antitubercular) causes vestibular damage on prolonged use.
Poisoning
Poisoning
may result from large doses of drugs because
‘it is the dose which distinguishes a drug from a poison’. Poison is a
‘substance which endangers life by severely affecting one or more vital
functions’. Not only drugs but other household and industrial chemicals,
insecticides, etc. are frequently involved in poisonings. Specific antidotes
such as receptor antagonists, chelating agents or specific antibodies are
available for few poisons. General supportive and symptomatic treatment is all
that can be done for others, and this is also important for poisons which have
a selective antagonist. These measures are:
1. Resuscitation And Maintenance Of Vital Functions
a. Ensure patent airway, adequate ventilation, give artificial
respiration/100% oxygen inhalation as needed.
b. Maintain blood pressure and heart beat by fluid and
crystalloid infusion, pressor agents, cardiac stimulants, etc, as needed.
c. Maintain body temperature.
d. Maintain blood sugar level by dextrose infusion, especially
in patients with altered sensorium.
2. Termination of exposure (decontamination) by removing the patient to fresh air (for inhaled
poisons), washing the skin and eyes (for poisons entering from the surface),
induction of emesis with syrup ipecac or gastric lavage (for ingested poisons).
Emesis should not be attempted in comatose or haemo-dynamically unstable
patient, as well as for kerosene poisoning due to risk of aspiration into
lungs. These procedures are also contraindicated in corrosive and CNS stimulant
poisoning. Emesis/gastric lavage is not recommended if the patient presents
> 2 hours after ingesting the poison; if the poison/its dose ingested are
known to be non life-threatening, or if the patient has vomited after consuming
the poison.
3.
Prevention of absorption of ingested poisons
A
suspension of 20–40 g (1g/kg) of activated charcoal, which has large surface
area and can adsorb many chemicals, should be administered in 200 ml of water.
However, strong acids and alkalies, metallic salts, iodine, cyanide, caustics,
alcohol, hydrocarbons and other organic solvents are not adsorbed by charcoal.
Charcoal should not be administered if there is paralytic ileus or intestinal
obstruction.
4. Hastening elimination of the poison by inducing
diuresis (furosemide, mannitol) or altering urinary pH (alkalinization for
acidic drugs, e.g. barbiturates). However, excretion of many poisons is not
enhanced by forced diuresis and it is generally not employed now. Haemodialysis
and haemoperfusion (passage of blood through a column of charcoal or adsorbant
resin) are more efficacious procedures.
4. Intolerance
It
is the appearance of characteristic toxic effects of a drug in an individual at
therapeutic doses. It is the converse of tolerance and indicates a low threshold
of the individual to the action of a drug. These are individuals who fall on
the extreme left side of the Gaussian frequency distribution curve for
sensitivity to the drug. Examples are:
§ A single dose of
triflupromazine induces muscular dystonias in some individuals, specially
children.
§ Only few doses of
carbamazepine may cause ataxia in some people.
§ One tablet of
chloroquine may cause vomiting and abdominal pain in an occasional patient.
5. Idiosyncrasy
It is genetically
determined abnormal reactivity to a chemical. The drug interacts with some
unique feature of the individual, not found in majority of subjects, and
produces the uncharacteristic reaction. As such, the type of reaction is restricted
to individuals with a particular genotype (see
p. 64). In addition, certain bizarre drug effects due to peculiarities of an
individual (for which no definite genotype has been described) are included
among idiosyncratic reactions, e.g.:
§ Barbiturates cause
excitement and mental confusion in some individuals.
§ Quinine/quinidine
cause cramps, diarrhoea, purpura, asthma and vascular collapse in some patients.
§ Chloramphenicol
produces nondoserelated serious aplastic anaemia in rare individuals.
6. Drug allergy
It is an
immunologically mediated reaction producing stereotype symptoms which are unrelated
to the pharmacodynamic profile of the drug, generally occur even with much
smaller doses and have a different time course of onset and duration. This is
also called drug hypersensitivity; but does not refer to increased response
which is called supersensitivity.
Allergic
reactions occur only in a small proportion of the population exposed to the drug
and cannot be produced in other individuals at any dose. Prior sensitization is
needed and a latent period of at least 1–2 weeks is required after the first
exposure. The drug or its metabolite acts as antigen (AG) or more commonly hapten (incomplete antigen: drugs have
small molecules which become antigenic only after binding with an endogenous
protein) and induce production of antibody (AB)/sensitized lymphocytes. Presence
of AB to a drug is not necessarily followed by allergy to it. Chemically
related drugs often show cross sensitivity. One drug can produce different
types of allergic reactions in different individuals, while widely different
drugs can produce the same reaction. The course of drug allergy is variable; an
individual previously sensitive to a drug may subsequently tolerate it without
a reaction and vice versa.
Mechanism And Types Of Allergic Reactions
A. Humoral
Type I (anaphylactic) reactions Reaginic antibodies (IgE) are produced which
get fixed to the mast cells. On exposure to the drug, AG: AB reaction takes
place on the mast cell surface (see
Fig. 11.2) releasing mediators like histamine, 5HT, leukotrienes especially LTC4
and D4, prostaglandins, PAF, etc. resulting in urticaria, itching, angioedema,
bronchospasm, rhinitis or anaphylactic shock. The manifestations occur quickly
after challenge and are called immediate
hypersensitivity. Antihistaminic drugs
are beneficial in some of these reactions.
Type II (cytolytic) reactions Drug + component of a specific tissue
cell act as AG. The resulting antibodies (IgG, IgM) bind to the target cells;
on reexposure AG: AB reaction takes place on the surface of these cells,
complement is activated and cytolysis occurs, e.g. thrombocytopenia, agranulocytosis,
aplastic anaemia, haemolysis, organ damage (liver, kidney, muscle), systemic
lupus erythematosus.
Type III (retarded, Arthus)
reactions These are mediated by circulating antibodies (predominantly
IgG, mopping AB). AG: AB complexes bind complement and precipitate on vascular
endothelium giving rise to a destructive inflammatory response. Manifestations
are rashes, serum sickness (fever, arthralgia, lymphadenopathy), polyarteritis
nodosa, Stevens Johnson syndrome (erythema multiforme, arthritis, nephritis,
myocarditis, mental symptoms). The reaction usually subsides in 1–2 weeks.
B. Cell mediated
TypeIV (delayed hypersensitivity) reactions These are mediated through
production of sensi tized Tlymphocytes carrying receptors for the AG. On
contact with the AG these T cells produce lymphokines
which attract granulocytes and generate an inflammatory response, e.g. contact
dermatitis, some rashes, fever, photosensitization. The reaction generally
takes > 12 hours to develop.
Treatment Of Drug Allergy
The
offending drug must be immediately stopped. Most mild reactions (like skin
rashes) subside by themselves and donot require specific treatment.
Antihistamines (H1) are beneficial in some type I reactions
(urticaria, rhinitis, swelling of lips, etc.) and some skin rashes. In case of anaphylactic
shock or angioedema of larynx the resuscitation council of UK has recommended
the following measures:
§ Put the patient in
reclining position, administer oxygen at high flow rate and perform
cardiopulmonary resuscitation if required.
§ Inject adrenaline 0.5
mg (0.5 ml of 1 in 1000 solution) i.m.; repeat every 5–10 min in case patient does
not improve or improvement is transient. This is the only life saving measure.
Adrenaline should not be injected i.v. (can itself be fatal) unless shock is
immediately life threatening. If adrenaline is to be injected i.v., it should
be diluted to 1:10,000 or 1:100,000 and infused slowly with constant
monitoring.
§ Administer a H1
antihistaminic (chlorpheniramine 10–20 mg) i.m./slow i.v. It may have adjuvant
value.
§ Intravenous
glucocorticoid (hydrocortisone sod. succinate 100–200 mg) should be added in severe/recurrent
cases. It acts slowly, but is specially valuable for prolonged reactions and in
asthmatics.
Adrenaline followed by a short course of
glucocorticoids is indicated for bronchospasm attending drug hypersensitivity.
Glucocorticoids are the only drug effective in type II, type III and type IV
reactions.
Drugs frequently causing allergic reactions
Drugs Frequently Causing
Allergic Reactions
Penicillins Salicylates
Cephalosporins Carbamazepine
Sulfonamides Allopurinol
Tetracyclines ACE inhibitors
Quinolones Methyldopa
Antitubercular drugs Hydralazine
Phenothiazines Local anaesthetics
Skin tests (intradermal, patch) or intranasal tests may forewarn in case of Type I
hypersensitivity, but not in case of other types. However, these tests are not
entirely reliable—false positive and false negative results are not rare.
7. Photosensitivity
It
is a cutaneous reaction resulting from drug induced sensitization of the skin
to UV radiation. The reactions are of two types:
Phototoxic Drug or its metabolite
accumulates in the skin, absorbs light and undergoes a photochemical reaction
followed by a photobiological reaction resulting in local tissue damage
(sunburnlike), i.e. erythema, edema, blistering followed by hyperpigmentation
and desquamation. The shorter wave lengths (290–320 nm, UVB) are responsible.
Drugs involved in acute phototoxic reactions are tetracyclines (especially
demeclocycline) and tar products. Drugs causing chronic and low grade
sensitization are nalidixic acid, fluoroquinolones, sulfones, sulfonamides,
phenothiazines, thiazides, amiodarone. This type of reaction is more common
than photoallergic reaction.
Photoallergic Drug or its metabolite
induces a cell mediated immune
response which on exposure to light of longer wave lengths (320–400 nm, UVA)
produces a papular or eczematous contact dermatitis like picture. Rarely
antibodies mediate photoallergy and the reaction takes the form of immediate
flare and wheal on exposure to sun. Drugs involved are sulfonamides, sulfonylureas,
griseofulvin, chloroquine, chlorpromazine.
8. Drug Dependence
Drugs capable of altering
mood and feelings are liable to repetitive use to derive euphoria, withdrawal
from reality, social adjustment, etc. Drug dependence is a state in which use
of drugs for personal satisfaction is accorded a higher priority than other
basic needs, often in the face of known risks to health.
There is a lot of
confusion in terminology and definitions; the following may serve to describe
different aspects of the problem.
Psychological dependence It is said to have developed when the individual believes that
optimal state of wellbeing is achieved only through the actions of the drug. It
may start as liking for the drug effects and may progress to compulsive drug
use in some individuals. The intensity of psychological dependence may vary
from desire to craving. Obviously, certain degree of psychological dependence
accompanies all patterns of self medication.
Reinforcement is the ability of the drug to produce effects that make the user wish to take
it again or to induce drug seeing
behaviour. Certain drugs (opioids, cocaine) are strong reinforcers, while
others (benzodiazepines) are weak reinforcers. Faster the drug acts, more
reinforcing it is.
Physical dependence It is an altered
physiological state produced by repeated administration of a drug which necessitates
the continued presence of the drug to maintain physiological equilibrium.
Discontinuation of the drug results in a characteristic withdrawal (abstinence) syndrome. Since the essence of the process
is adaptation of the nervous system to function normally in the presence of the
drug, it has been called ‘neuroadaptation’.
Drugs
producing physical dependence are— opioids, barbiturates and other depressants
including alcohol and benzodiazepines. Stimulant drugs, e.g. amphetamines,
cocaine produce little or no physical dependence.
Drug abuse Refers to use of a drug by self medication in
a manner and amount that deviates from the approved medical and social patterns
in a given culture at a given time. The term conveys social disapproval of the
manner and purpose of drug use. For regulatory agencies, drug abuse refers to any use of an ilicit drug.
Drug addiction It is a pattern of
compulsive drug use characterized
by overwhelming involvement with the use of a drug. Procuring the drug and
using it takes precedence over other activities. Even after withdrawal most
addicts tend to relapse. Physical dependence, though a strong impetus for continued
drug use, is not an essential feature of addiction. Amphetamines, cocaine, cannabis,
LSD are drugs which produce addiction but little/no physical dependence. On the
other hand, drugs like nalorphine produce physical dependence without imparting
addiction in the sense that there is little drug seeking behaviour.
Drug habituation It denotes less
intensive involvement with the
drug, so that its withdrawal produces only mild discomfort. Consumption of tea,
coffee, tobacco, social drinking are regarded habituating, physical dependence
is absent.
Basically,
habituation and addiction imply different degrees of psychological dependence
and it may be difficult to draw a clearcut line of distinction between the two.
Therefore, it is better to avoid using these terms in describing drug
dependence and related conditions.
9. Drug Withdrawal Reactions
Apart
from drugs that are usually recognised as producing dependence, sudden
interruption of therapy with certain other drugs also results in adverse
consequences, mostly in the form of worsening of the clinical condition for
which the drug was being used, e.g.:
§ Acute adrenal insufficiency
may be precipitated by abrupt cessation of corticosteroid therapy.
§ Severe hypertension,
restlessness and sympathetic overactivity may occur shortly after discontinuing
clonidine.
§ Worsening of angina
pectoris, precipitation of myocardial infarction may result from stoppage of β blockers.
§ Frequency of seizures
may increase on sudden withdrawal of an antiepileptic.
These manifestations
are also due to adaptive changes and can be minimized by gradual withdrawal.
10. Teratogenicity
It refers to capacity
of a drug to cause foetal abnormalities when administered to the pregnant
mother. The placenta does not strictly constitute a barrier and any drug can
cross it to a greater or lesser extent. The embryo is one of the most dynamic
biological systems and in contrast to adults, drug effects are often
irreversible. The thalidomide disaster (1958–61) resulting in thousands of
babies born with phocomelia (seal
like limbs) and other defects focused attention to this type of adverse effect.
Drugs can affect the
foetus at 3 stages—
§ Fertilization and implantation—conception to 17 days—failure of pregnancy which
often goes unnoticed.
§ Organogenesis—18 to 55 days of
gestation— most vulnerable period,
deformities are produced.
§ Growth and development—56 days onwards developmental
and functional abnormalities can occur, e.g. ACE inhibitors can cause hypoplasia
of organs, specially lungs and kidneys; NSAIDs may induce premature closure of
ductus arteriosus.
The type of
malformation depends on the drug as well as the stage of exposure to the teratogen.
Foetal exposure depends on the blood level and duration for which the drug
remains in maternal circulation. The teratogenic potential of a drug is to be
considered against the background of congenital abnormalities occurring
spontaneously, which is ~ 2% of all pregnancies. Majority of implicated drugs are
low grade teratogens, i.e. increase the incidence of malformations only
slightly, which may be very difficult to detect, confirm or refute.
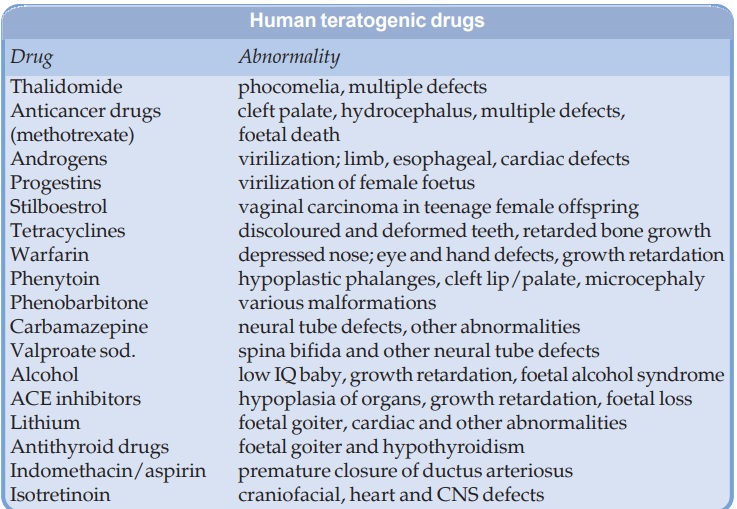
Nevertheless, some drugs have been clearly associated with causing foetal
abnormalities in human beings. These are listed in the box. However, only few
mothers out of those who receive these drugs during the vulnerable period will
get a deformed baby, but the exact risk posed by a drug is difficult to estimate.
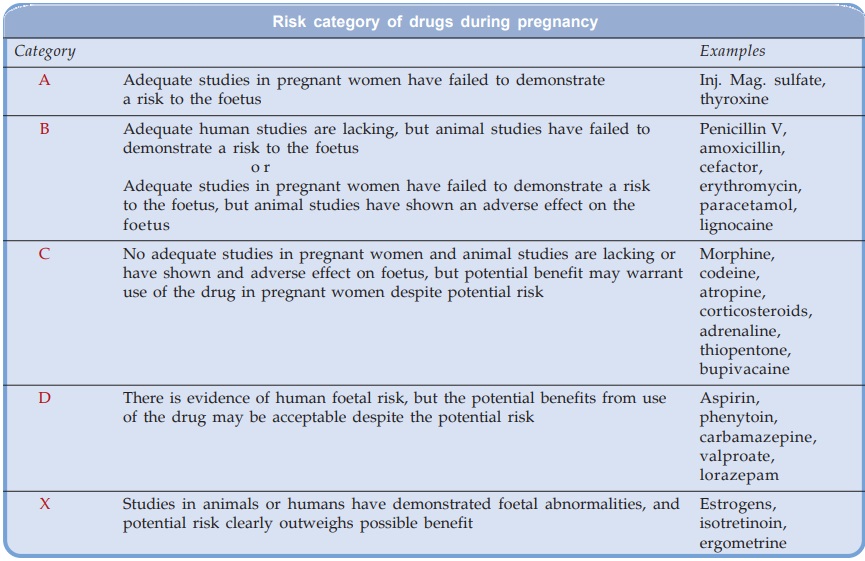
The
USFDA has graded the documentation of risk for causing birth defects into five
categories (see box).
It
is, therefore, wise to avoid all drugs during pregnancy unless compelling
reasons exist for their use regardless of the assigned pregnancy category, or
presumed safety.
Frequency
of spontaneous as well as drug induced malformations, especially neural tube
defects, may be reduced by folate therapy during pregnancy.
11. Mutagenicity And Carcinogenicity
It refers to capacity
of a drug to cause genetic defects and cancer respectively. Usually oxidation
of the drug results in the production of reactive intermediates which affect
genes and may cause structural changes in the chromosomes. Covalent interaction
with DNA can modify it to induce mutations, which may manifest as heritable defects
in the next generation. If the modified DNA sequences code for factors that
regulate cell proliferation/growth, i.e. are protooncogenes, or for proteins
that inhibit transcription of protooncogenes, a tumour (cancer) may be
produced. Even without interacting directly with DNA, certain chemicals can
promote malignant change in genetically damaged cells, resulting in carcinogenesis.
Chemical carcinogenesis generally takes several (10–40) years to develop. Drugs
implicated in these adverse effects are—anticancer drugs, radioisotopes,
estrogens, tobacco. Generally, drugs which show mutagenic or carcinogenic
potential are not approved for marketing/are withdrawn, unless useful in life-threatening
conditions.
12. Drug Induced Diseases
These are also called iatrogenic (physician induced) diseases,
and are functional disturbances (disease) caused by drugs which persist even
after the offending drug has been withdrawn and largely eliminated, e.g.:
Peptic ulcer by
salicylates and corticosteroids.
Parkinsonism by
phenothiazines and other
antipsychotics.
Hepatitis by
isoniazid.
DLE by hydralazine.
Related Topics
